JTG 2025 Poster Gallery
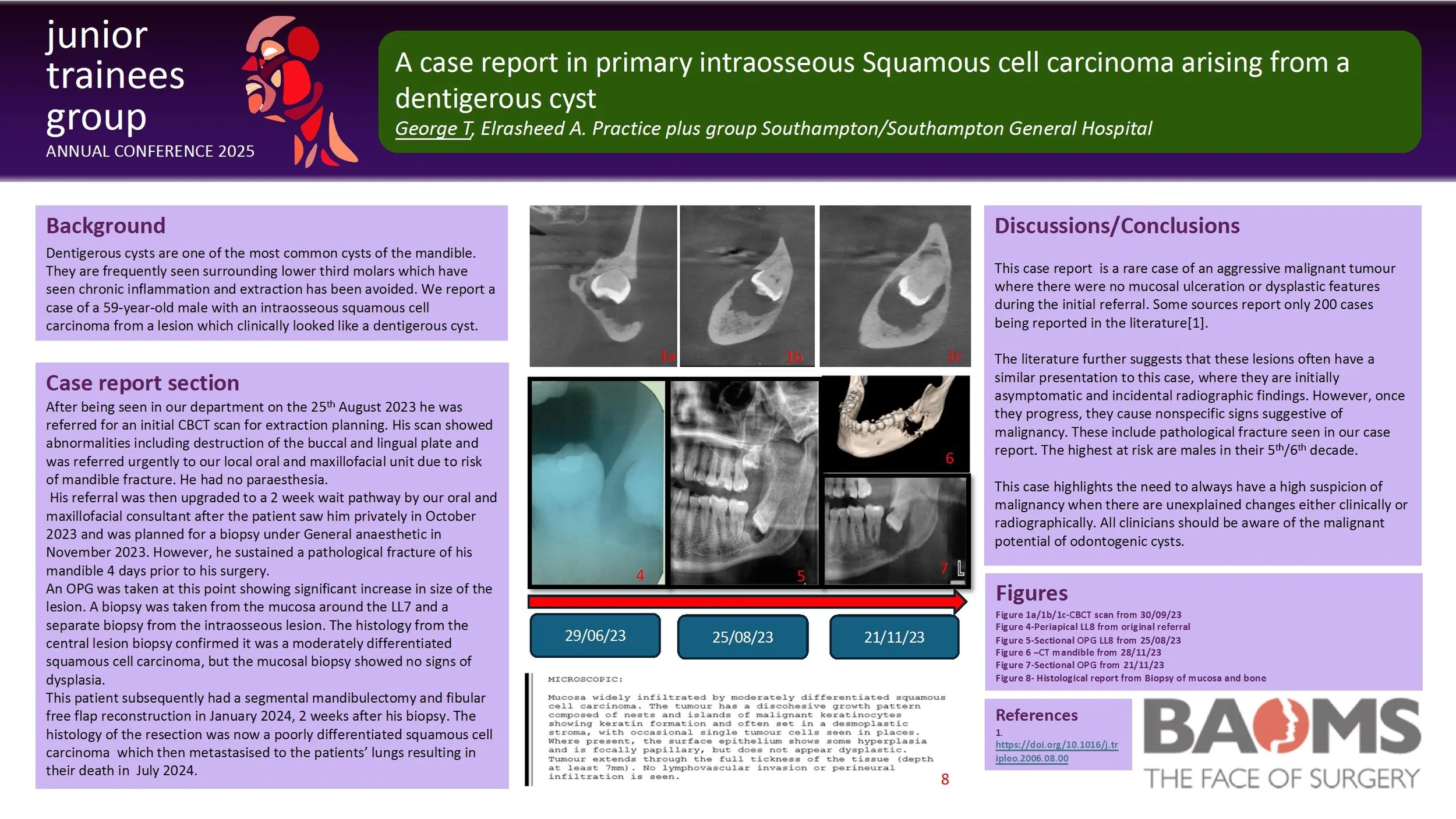
A case report in primary intraosseous Squamous cell carcinoma arising from a dentigerous cyst
Dentigerous cysts are one of the most common cysts of the mandible. They are frequently seen surrounding lower third molars which have seen chronic inflammation and extraction has been avoided. We report a case of a 59-year-old male with an intraosseous squamous cell carcinoma from a lesion which clinically looked like a dentigerous cyst.
He was referred by his General Dental Practitioner to our oral surgery department for extraction of a symptomatic LL8 in June 2023. His initial CBCT scan showed abnormalities including destruction of the buccal and lingual plate and was referred urgently to our local oral and maxillofacial unit due to risk of mandible fracture. He had no paraesthesia.
His referral was then upgraded to a 2 week wait pathway by our oral and maxillofacial consultant after the patient saw him privately in October 2023 and was planned for a biopsy under General anaesthetic in November 2023. However, he sustained a pathological fracture of his mandible 4 days prior to his surgery. An OPG was taken at this point showing significant increase in size of the lesion.
A biopsy was taken from the mucosa around the LL7 and a separate biopsy from the intraosseous lesion. The histology from the central lesion biopsy confirmed it was a moderately differentiated squamous cell carcinoma, but the mucosal biopsy showed no signs of dysplasia.
This patient subsequently had a segmental mandibulectomy and fibular free flap reconstruction in January 2024, 2 weeks after his biopsy. The histology of the resection was now a poorly differentiated squamous cell carcinoma.
This highlights an unusual case of an aggressive malignant tumour where there was no mucosal ulceration or dysplastic features. It emphasises the importance of reassessing the patient’s clinical picture and to be aware of the potential malignant change of odontogenic cysts.
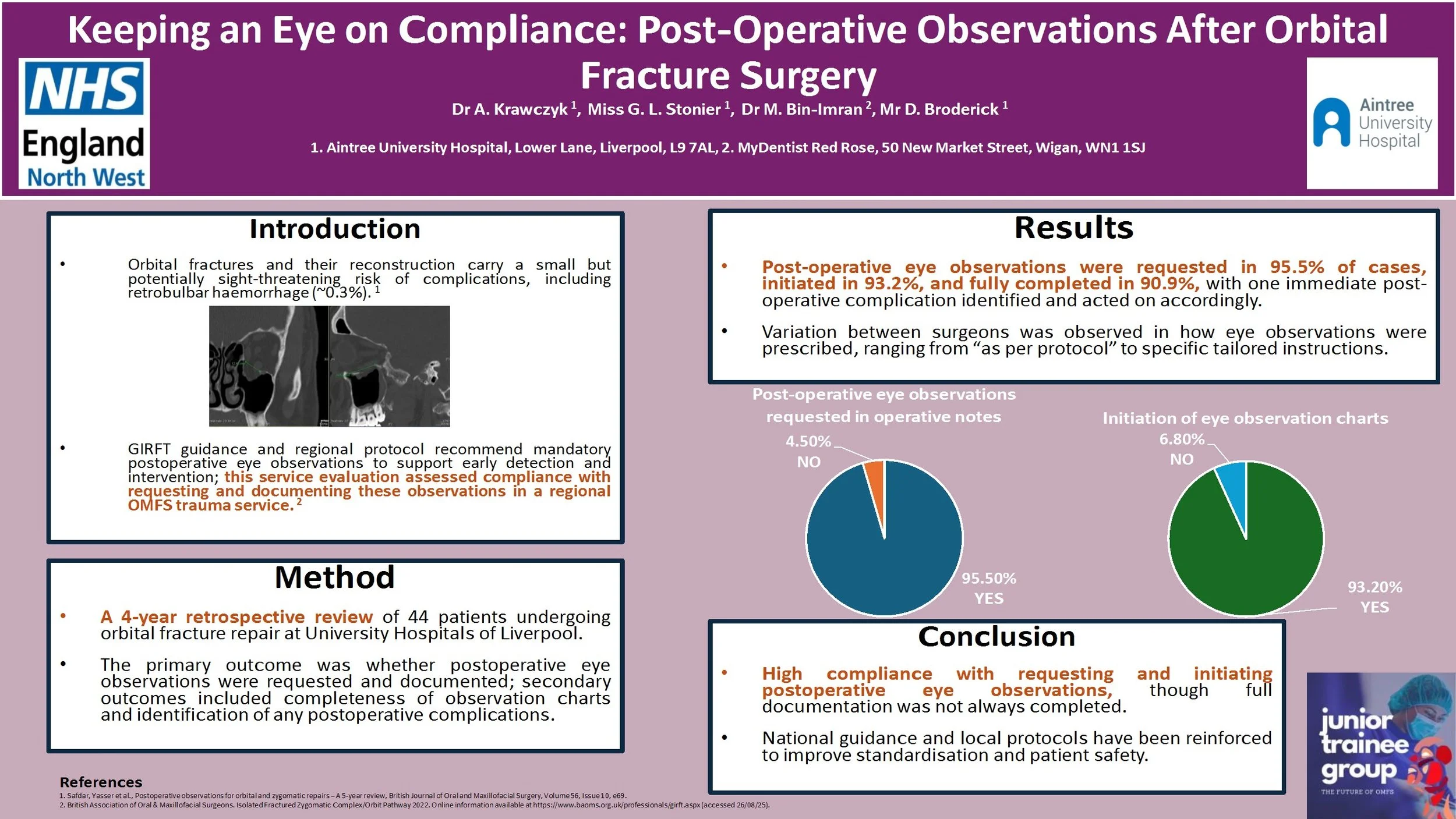
Keeping an Eye on Compliance: Post-Operative Observations After Orbital Fracture Surgery
Introduction:
Orbital fractures and the following reconstructive surgery carries a risk of sight-threatening complications, including retrobulbar haemorrhage (~0.3%).1 The Getting It Right First time (GIRFT) guidance2 and our regional protocol recommends mandatory postoperative eye observations to allow for early recognition and therefore intervention in case of developing sight‐threatening complications. This service evaluation assessed compliance of a regional Oral and Maxillofacial trauma service with requesting and documenting eye observations following orbital fracture surgery.
Method:
A retrospective review of 44 consecutive patients undergoing orbital fracture repair between 2020 and 2024 was conducted at University Hospitals of Liverpool Group. Information was recorded using an electronic data collection tool. The primary outcome was whether post-operative eye observations were requested and documented, with secondary outcomes including whether eye observation charts were completed fully and any complications identified.
Results:
Of the 44 patients, post-operative eye observations were requested in operative notes in 95.5% of cases. Majority (93.2%) of patients had eye observation charts initiated, with complete documentation recorded in 90.9%. One case displayed an immediate post-operative complication. Variation in practice between surgeons was noted, with some prescribing eye observations ‘as per protocol’ and others outlining specific recommendation.
Conclusion:
Compliance with requesting and initiating documentation of post-operative eye observations was high but full completion was inconsistent. National guidance and local protocol have been reinforced to optimise patient safety.
References:
1. Safdar, Yasser et al., Postoperative observations for orbital and zygomatic repairs – A 5-year review, British Journal of Oral and Maxillofacial Surgery, Volume 56, Issue 10, e69.
2. British Association of Oral & Maxillofacial Surgeons. Isolated Fractured Zygomatic Complex/Orbit Pathway, 2022. Online information available at https://www.baoms.org.uk/professionals/girft.aspx (accessed 26/08/25).
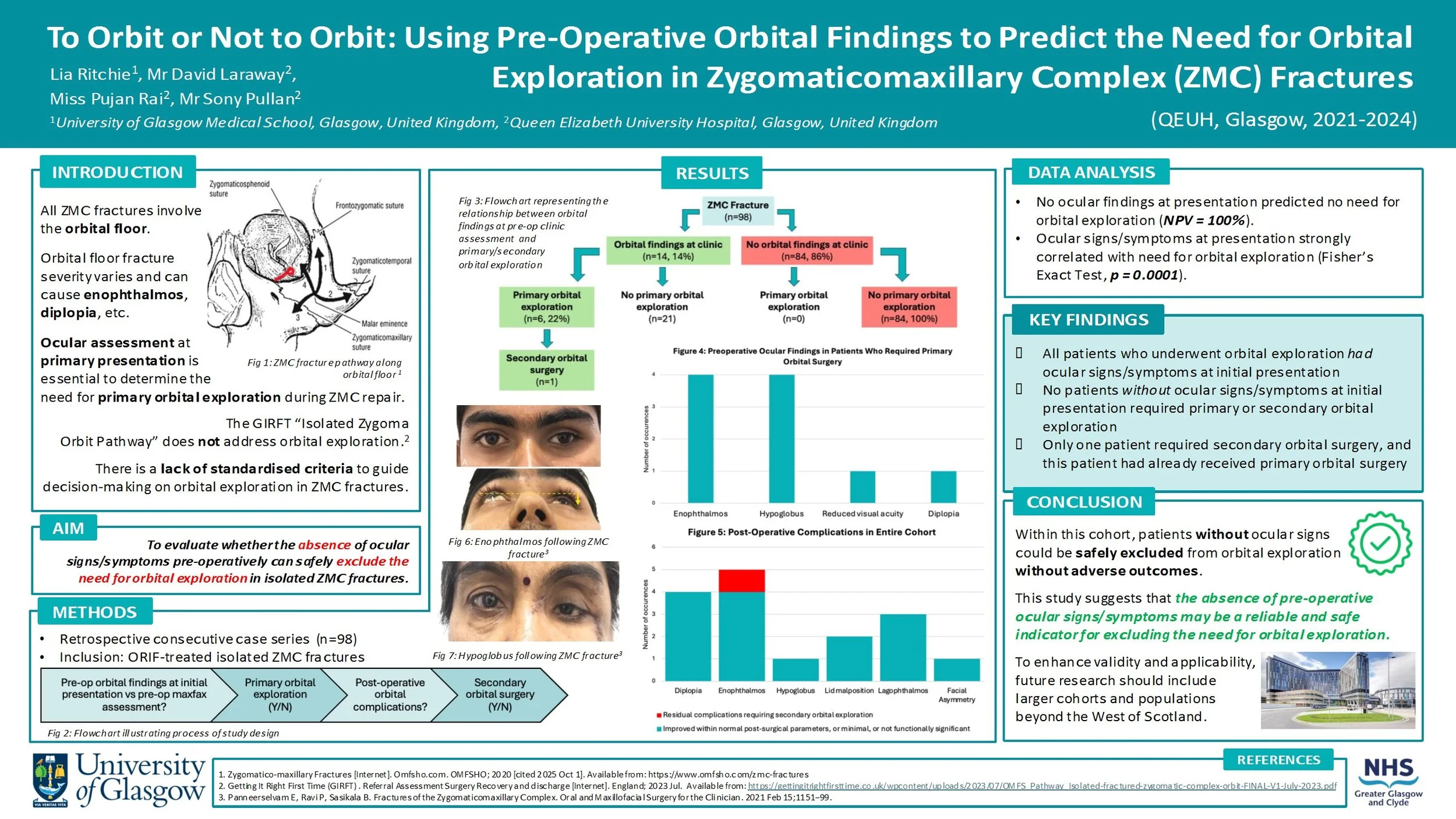
To Orbit or Not to Orbit: Using Pre-Operative Orbital Findings to Predict the Need for Orbital Exploration in Zygomaticomaxillary Complex (ZMC) Fractures
Introduction:
All ZMC fractures involve orbital fractures, with orbital floor fracture severity varying depending on the mechanism and energy of injury. Disruption of the orbital floor changes the orbital volume, increasing the risk of ocular signs/symptoms (e.g. enophthalmos, diplopia). This must be assessed at primary presentation to decide if primary orbital surgery should be performed alongside ZMC repair.
There is currently no standardised set of criteria to guide the decision-making process for orbital exploration in ZMC fractures. This study will evaluate whether the absence of ocular signs/symptoms pre-operatively can safely exclude the need for orbital exploration.
Method:
Data was retrospectively collected from a consecutive series of 98 patients who had ZMC fractures requiring ORIF intervention at the QEUH between 2021-2024. The presence/absence of ocular signs/symptoms at initial assessment was recorded. The cohort was then assessed to determine which patients underwent primary orbital exploration. Post-operative outcomes were reviewed, including whether any patients subsequently required secondary orbital surgery.
Results:
27 patients (28%) presented with ocular signs/symptoms, 6 of them underwent primary orbital surgery. Among the 71 patients (72%) who had no ocular findings at initial presentation, none required orbital surgery. Only 1 patient in the cohort required secondary orbital surgery, and this patient had also undergone primary orbital surgery.
Conclusion:
The absence of pre-operative ocular signs/symptoms may be a reliable indicator for excluding the need for orbital exploration. No patients who did not receive primary orbital exploration needed secondary orbital exploration, proving there were no late ocular complications from this approach.
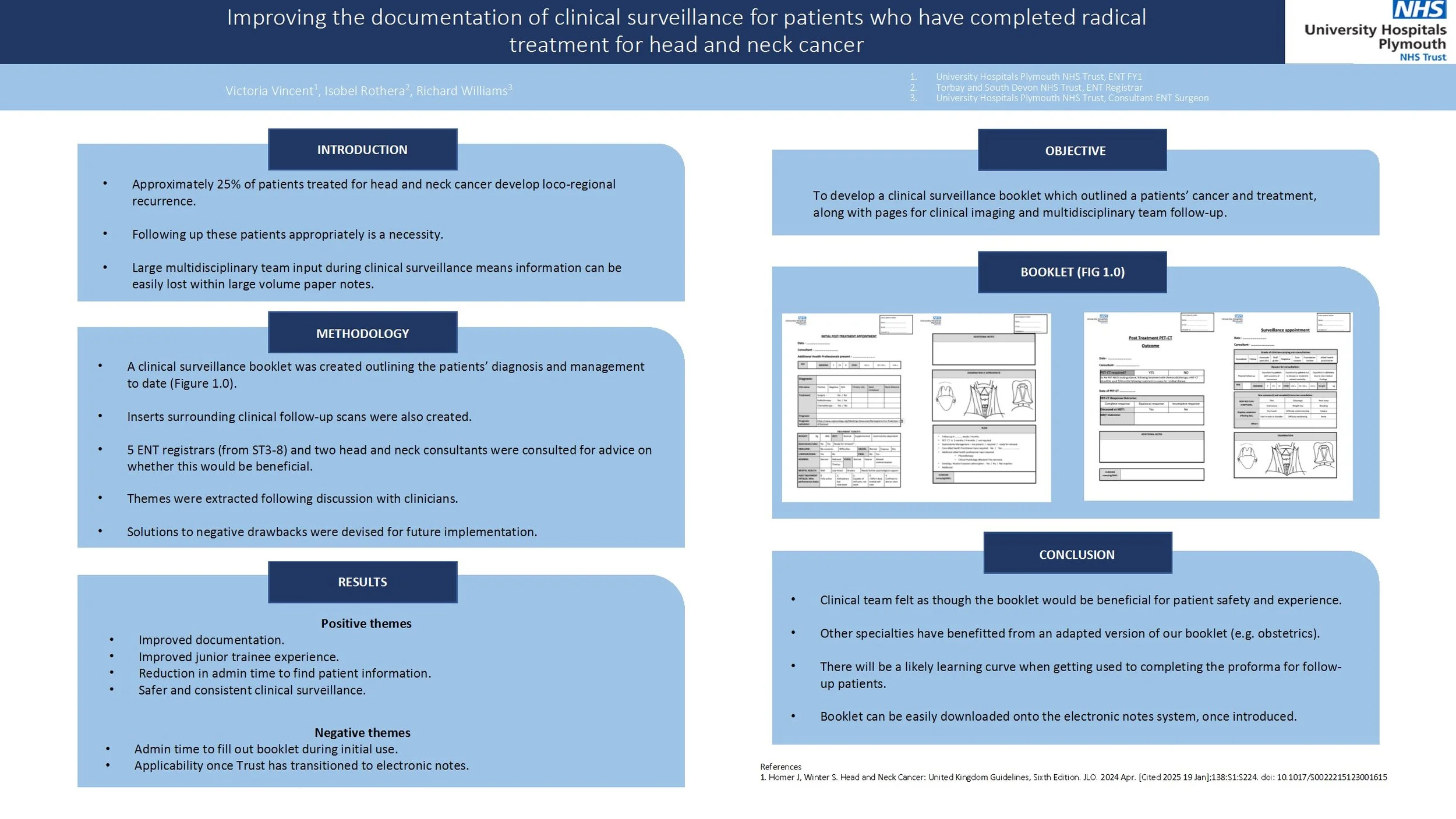
Improving the documentation of clinical surveillance for patients who have completed radical treatment for head and neck cancer
Approximately 25% of patients treated for head and neck cancer develop loco-regional recurrence. Therefore, ensuring that we are following up these patients appropriately is a necessity. With large multidisciplinary team input during clinical surveillance, it is easy for information to get lost within a large volume of paper notes. Therefore, the aim of this project was to develop a clinical surveillance booklet which outlined the patients’ cancer and treatment, along with pages for clinical imaging and MDT follow-up.
A clinical surveillance booklet was created outlining the patients’ diagnosis and management to date. Inserts surrounding clinical follow-up and scans were also created. Before printing, five ENT registrars ranging from ST3-8 and two head and neck consultants were consulted for advice on whether this would be beneficial.
The main positive themes from interview were surrounding improved documentation, improved junior trainee experience, reduction in admin time to find patient information and safer clinical surveillance.
Main positive themes were surrounding admin time to fill out the booklet and use once the trust has transitioned to electronic notes.
Overall, the clinical team feel as though a clinical surveillance booklet would be beneficial for patient safety and experience. Other specialties, such as obstetrics, have benefitted from an adapted version of our proposed booklet. There will likely be a learning curve when getting used to completing the proforma for follow-up patients. The booklet can be easily downloaded to the electronic notes system, once it has been introduced.
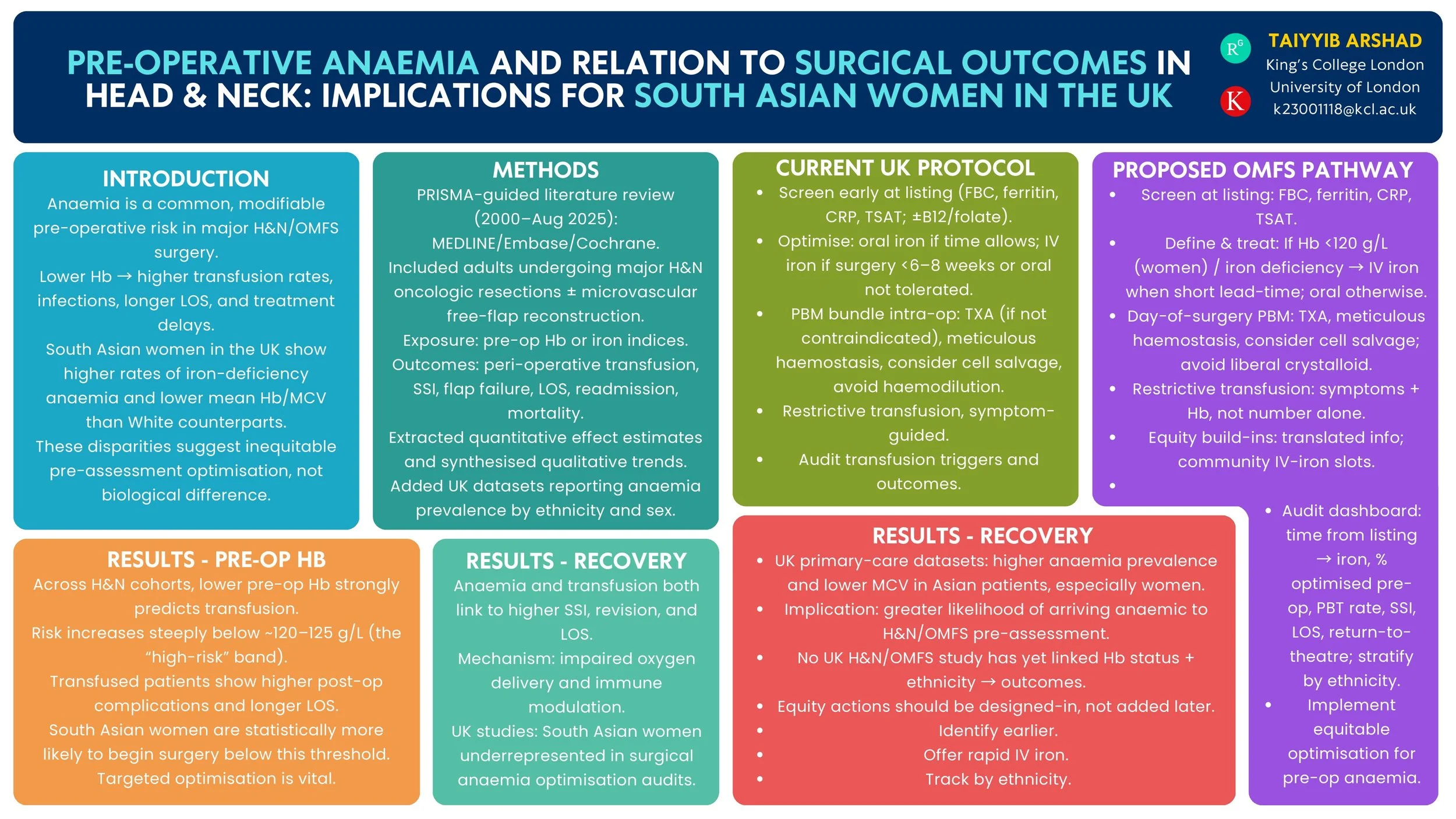
Pre-operative Anaemia and Surgical Outcomes in Head & Neck Surgery: Implications for South Asian Women in the UK
Introduction
Pre-operative anaemia is a modifiable risk factor that increases complications after head & neck (H&N) surgery. UK primary-care data show a higher burden of anaemia among women of Asian heritage than White women. We reviewed the evidence on pre-operative anaemia and H&N/OMFS surgical outcomes and summarised UK epidemiology by ethnicity to inform equity-focused peri-operative pathways.
Method
PRISMA-guided review (MEDLINE/Embase/Cochrane, 2000–Aug 2025). Inclusion: studies of H&N/OMFS surgery reporting pre-operative haemoglobin/iron indices vs peri-operative outcomes (transfusion, surgical-site infection, return to theatre, flap failure, length of stay, readmission, mortality, oncological endpoints). We additionally summarised UK population/primary-care studies reporting anaemia prevalence in women by ethnicity and current UK peri-operative anaemia guidance.
Results
Across H&N cohorts and syntheses, lower pre-operative haemoglobin independently associates with higher peri-operative transfusion and adverse outcomes; a high-risk transfusion threshold is consistently observed around ~120 g/L. UK guidance recommends routine pre-operative screening and optimisation (including intravenous iron) for major surgery. UK primary-care datasets demonstrate higher anaemia prevalence and lower mean haemoglobin/MCV among Asian compared with White patients, indicating that women of South Asian heritage are more likely to present anaemic before surgery. No UK H&N/OMFS study has yet quantified outcome differences by both anaemia status and ethnicity.
Conclusion
Robust evidence links pre-operative anaemia with worse H&N surgical outcomes, and UK datasets show higher anaemia prevalence in Asian women. These findings support a standardised OMFS/H&N anaemia optimisation pathway—early case-finding, iron studies, rapid IV iron, and transfusion-sparing strategies—with particular attention to access and uptake among South Asian women. Future UK multicentre analyses should test whether ethnicity modifies anaemia-related surgical risk and evaluate pathway impact on complications and treatment delays.
Quality Improvement Project – analysing compliance of Russells Hall Hospital OMFS department against SDCEP Anticoagulant guidelines
Introduction
The Royal College of Anaesthetists (RCA) highlights key considerations when selecting anaesthetic modalities, including operator experience, diagnosis severity, and peri-operative compliance. This Quality Improvement Project (QIP) aimed to assess anaesthetic use in secondary care against RCA guidance and develop a long-term strategy to reduce reliance on CEPOD where possible. Benefits include minimising risks of GA-associated mortality, enabling immediate management, reducing anticipatory stress for children and parents, and optimising resource allocation by alleviating CEPOD pressures.
Method
A retrospective pilot cycle was conducted at University Hospital Wales, followed by two prospective cycles at Dudley Group Hospitals and Royal Wolverhampton Trusts. Each cycle included 20 paediatric OMFS presentations from the emergency department. Data collected comprised age, gender, diagnosis, mechanism of injury, pre-operative compliance, management, anaesthetic modality, and peri-operative compliance. Between the second and third cycle, an action plan was presented to paediatric and OMFS teams.
Results
In the first cycle (mean age 4.75; 70% male), 90% were managed with GA, 5% with inhalation sedation, and 5% with LA. The second cycle (mean age 9.7; 75% male) showed 25% GA, 5% inhalation sedation, and 70% LA. In the third cycle (mean age 8; 70% male), 40% were managed with GA, 5% inhalation sedation, 5% ketamine sedation, and 50% with LA.
Conclusion
The QIP demonstrated varied anaesthetic modalities with increasing uptake of sedation between the second and third cycles. Future improvements include implementing a proforma for children undergoing GA to evaluate alternative modalities, ensuring safer, more efficient decision-making. Incorporating Patient Reported Outcomes from parents and children could further inform service development, providing insights into waiting times, cosmetic results, and anxiolysis during treatment.
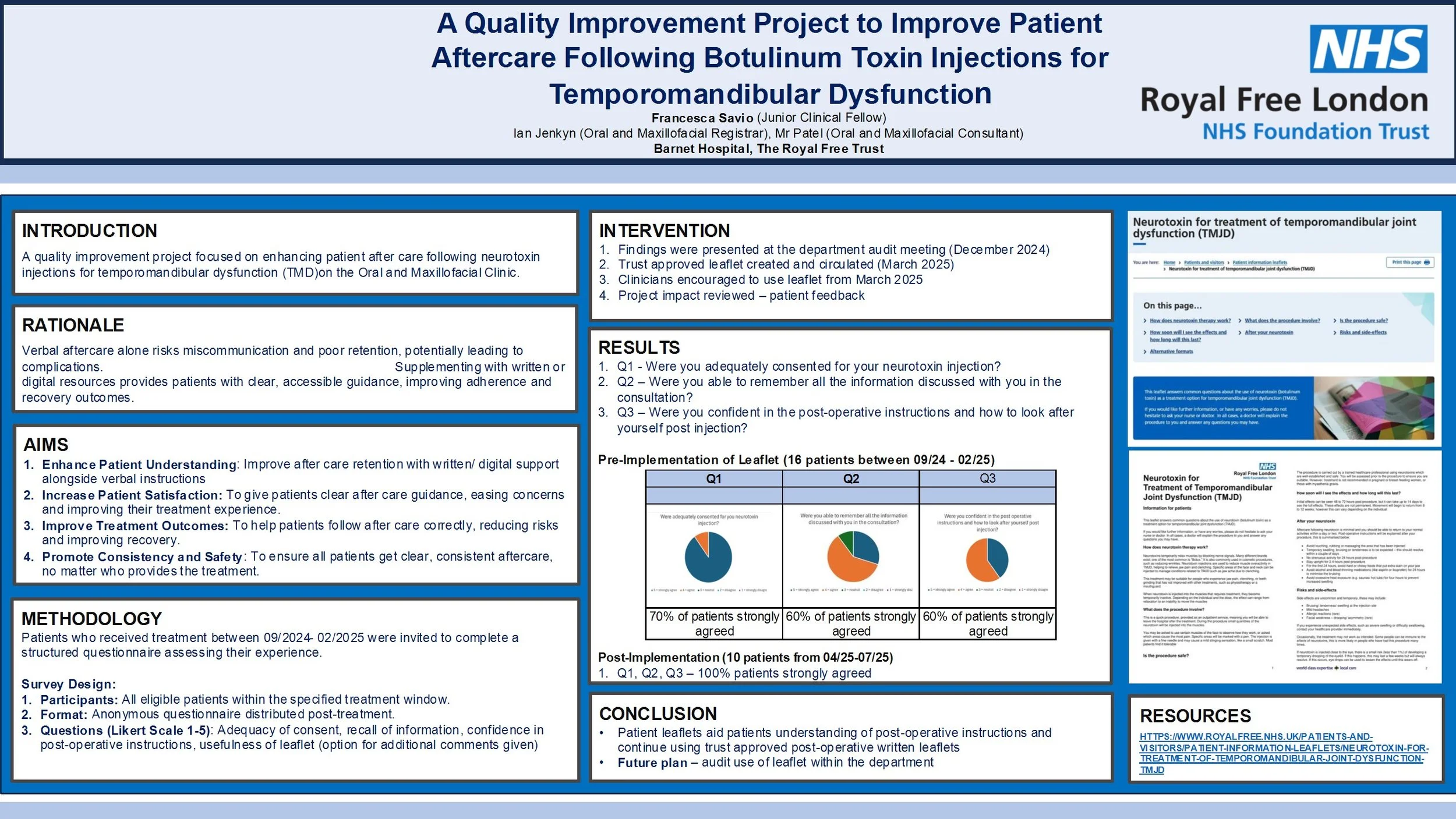
A Quality Improvement Project to Improve Patient Aftercare Following Botulinum Toxin Injections for Temporomandibular Dysfunction
Introduction
Temporomandibular dysfunction (TMD) is increasingly managed with botulinum toxin injections. However, current practice at the Royal Free London NHS Foundation Trust involves providing only verbal aftercare instructions, which may be insufficient for optimal patient understanding and recovery. This quality improvement project aimed to enhance patient aftercare by introducing written resources to supplement verbal guidance.
Method
Two audit cycles were conducted. In Cycle 1 (Feb 2025), patients who received botulinum toxin injections for TMD between Sept 2024 and Feb 2025 were surveyed via telephone using a structured questionnaire. Questions assessed consent quality, recall of verbal instructions, confidence in post-operative care, and interest in written materials. Following Cycle 1, a trust-approved patient leaflet was introduced. Cycle 2 (June 2025) repeated the audit for patients treated after April 2025, evaluating the impact of the leaflet.
Results
Cycle 1 included 16 patients (14 female, 2 male; average age 45). Of the 10 respondents, 90% strongly agreed they were adequately consented, 60% agreed they remembered the verbal instructions, and 100% expressed interest in written aftercare materials. In Cycle 2, patients were surveyed post-leaflet implementation. All respondents (100%) found the written instructions useful and agreed they improved their confidence in post-treatment care.
Conclusion
The introduction of written aftercare materials significantly improved patient satisfaction and confidence in managing post- injections care for TMD. The audit supports continued use of written leaflets as standard practice and highlights the importance of multimodal communication in clinical care. Future audits will monitor long-term outcomes and adherence to aftercare protocols.
An Audit on the Use of Physiotherapy Referral as Part of First-Line Management for Myogenic TMD In An OMFS Department
Title: A Quality Improvement Project on the Use of Physiotherapy Referral as Part of First-Line Management for Myogenic TMD in an OMFS Department
Background:
Myogenic TMD is a common condition managed primarily with conservative treatment, including physiotherapy. National guidance from Getting It Right First Time (GIRFT) highlights physiotherapy as a key first-line intervention. However, referral practices can be inconsistent, risking suboptimal patient outcomes.
Aim:
To assess whether new patients diagnosed with myogenic TMD were appropriately being diagnosed and referred for physiotherapy in an Oral and Maxillofacial Surgery department, and to evaluate the impact of targeted interventions.
Standards:
100% of new myogenic TMD patients should be considered for physiotherapy referral, in line with GIRFT and departmental guidelines.
Methods:
Two audit cycles (n=50 each) were completed. Inclusion criteria: new patients diagnosed with myogenic TMD. Exclusion criteria: arthrogenic or trauma-related TMD, or those beyond initial management. Data were collected retrospectively from electronic records.
Between cycles, a structured intervention was implemented, including:
• Creation of a dedicated Cerner physiotherapy referral pathway
• Departmental teaching and governance presentations
• Visual prompts and email reminders
Results:
Referral rates improved from 14% in Cycle 1 to 70% in Cycle 2. Patient demographics were comparable across cycles, with no significant gender or age-related differences in referral patterns.
Conclusion:
Initial referral rates were significantly below expected standards. Following simple, targeted interventions, compliance improved fivefold. This highlights the effectiveness of education and system-based changes in improving adherence to evidence-based TMD management.
Recommendations:
Further efforts should focus on standardising diagnosis documentation, embedding referral prompts, and re-auditing to ensure sustained improvement. Consideration should also be given to evaluating patient outcomes and physiotherapy attendance in future cycles.
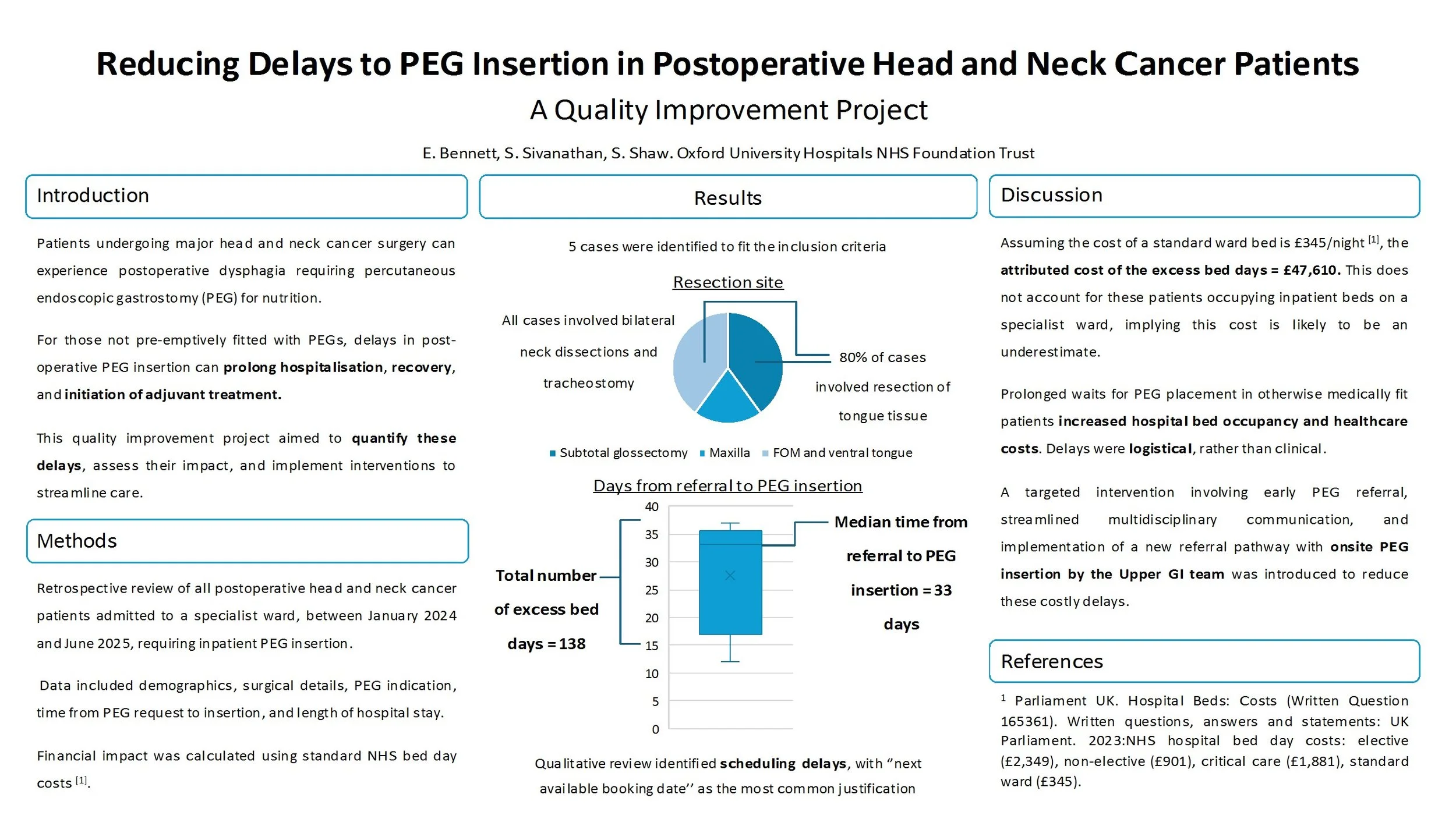
Reducing Delays to PEG Insertion in Postoperative Head and Neck Cancer Patients - A Quality Improvement Project
Reducing Delays to PEG Insertion in Postoperative Head and Neck Cancer Patients: A Quality Improvement Project
Introduction:
Patients undergoing major head and neck cancer surgery can experience postoperative dysphagia requiring percutaneous endoscopic gastrostomy (PEG) for nutrition. For those not pre-emptively fitted with PEGs, delays in post-operative PEG insertion can prolong hospitalisation, recovery, and initiation of adjuvant treatment. This quality improvement project aimed to quantify these delays, assess their impact, and implement interventions to streamline care.
Methods:
A retrospective review of all postoperative head and neck cancer patients admitted to a specialist ward, in a single centre, between January 2024, and June 2025, requiring inpatient PEG insertion was done. Data included demographics, surgical details, PEG indication, time from PEG request to insertion, and length of hospital stay. Financial impact was calculated using standard NHS bed day costs.
Results:
Five patients met inclusion criteria. All had extensive surgical procedures including bilateral neck dissections and tracheostomy. Median time from PEG request to insertion was 33 days (range: 12–37 days). Qualitative review revealed scheduling delays, with “next available booking date” as the most common justification. These delays accounted for 138 excess bed days, equating to an estimated cost of £47,610.
Discussion:
Prolonged waits for PEG placement in otherwise medically fit patients increased hospital bed occupancy and healthcare costs. Delays were logistical, rather than clinical. A targeted intervention involving early PEG referral, streamlined multidisciplinary communication, and onsite PEG insertion by the Upper GI team was introduced.
Conclusion:
Delayed PEG insertion in postoperative head and neck cancer patients leads to avoidable hospitalisation, financial burden, and may delay adjuvant treatment. Reasons for delay were specific to logistical factors within the unit. Results were presented and led to the implementation of an onsite referral pathway and improved interdepartmental coordination in order to offer a sustainable solution.
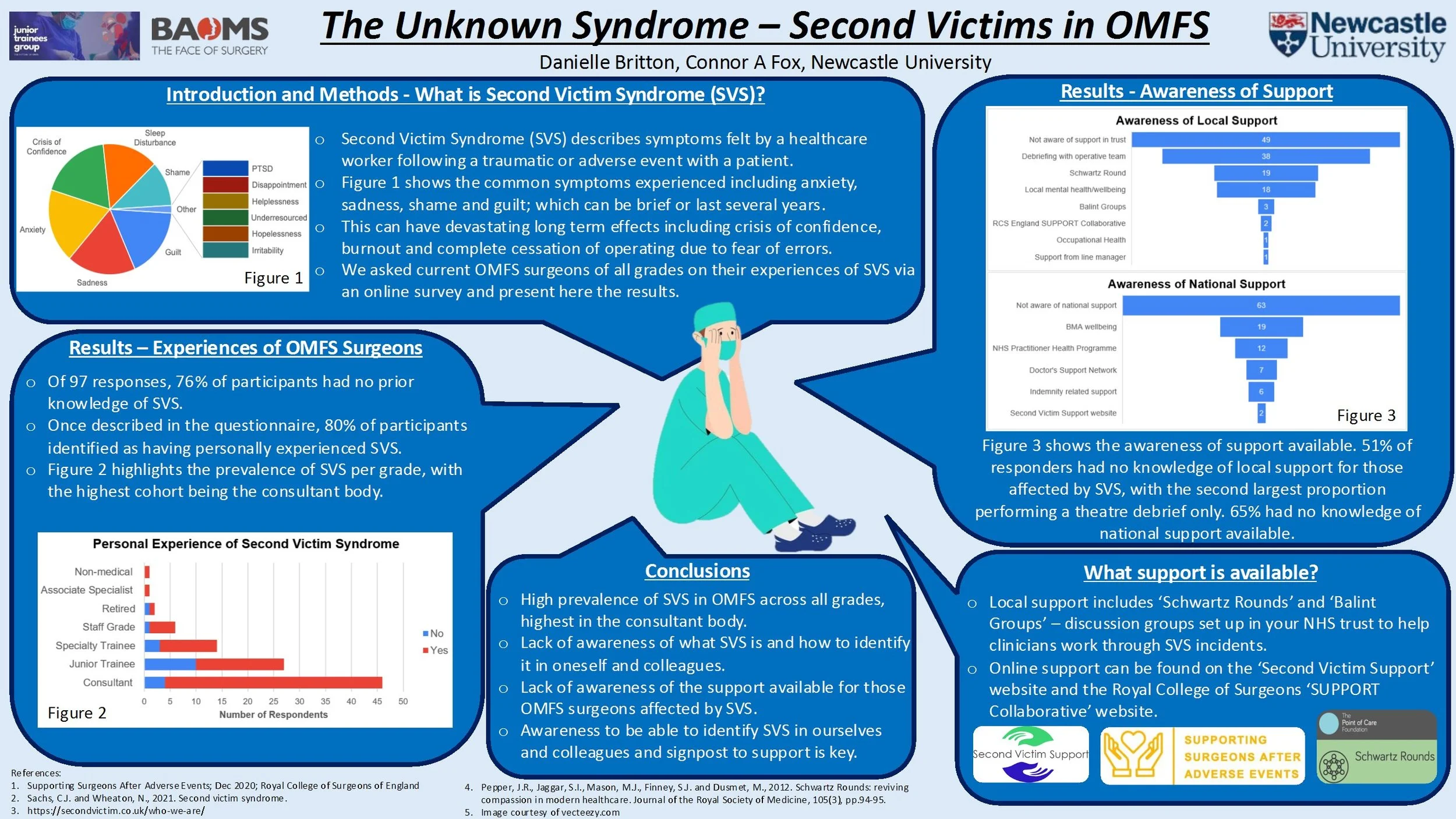
The Unknown Syndrome – Second Victims in OMFS
Second victim syndrome within surgery encompasses the psychological and physical symptoms surgeons can experience after an adverse event. Post-traumatic symptoms amongst surgeons equal those experienced by military personnel returning from conflict. These symptoms can lead to workplace errors, crises of self-confidence and, over time, complete cessation of operating.
The Royal College of Surgeons of England (RCS) recently developed guidance on supporting surgeons after adverse events and the “SUPPORT” collaborative to help those affected. At the time of writing, no work has been conducted into increasing awareness or evaluating the impacts of second victim syndrome within OMFS in the UK, nor how we as a specialty can best support those affected.
Performed as part of the BAOMS student bursary, this research assesses the prevalence of second victim symptomatology within OMFS colleagues of all levels (junior trainees to consultant level) through the use of electronic surveys. These surveys gathered information including awareness of second victim syndrome, knowledge of support currently available, anonymous personal experiences, and what further support could be beneficial for those affected.
With the knowledge gained, this project aims to provide education and increase awareness of second victim syndrome, its symptoms, signpost to support currently available for OMFS surgeons and trainees, and highlight how clinical leads can improve post-trauma support within their own units.
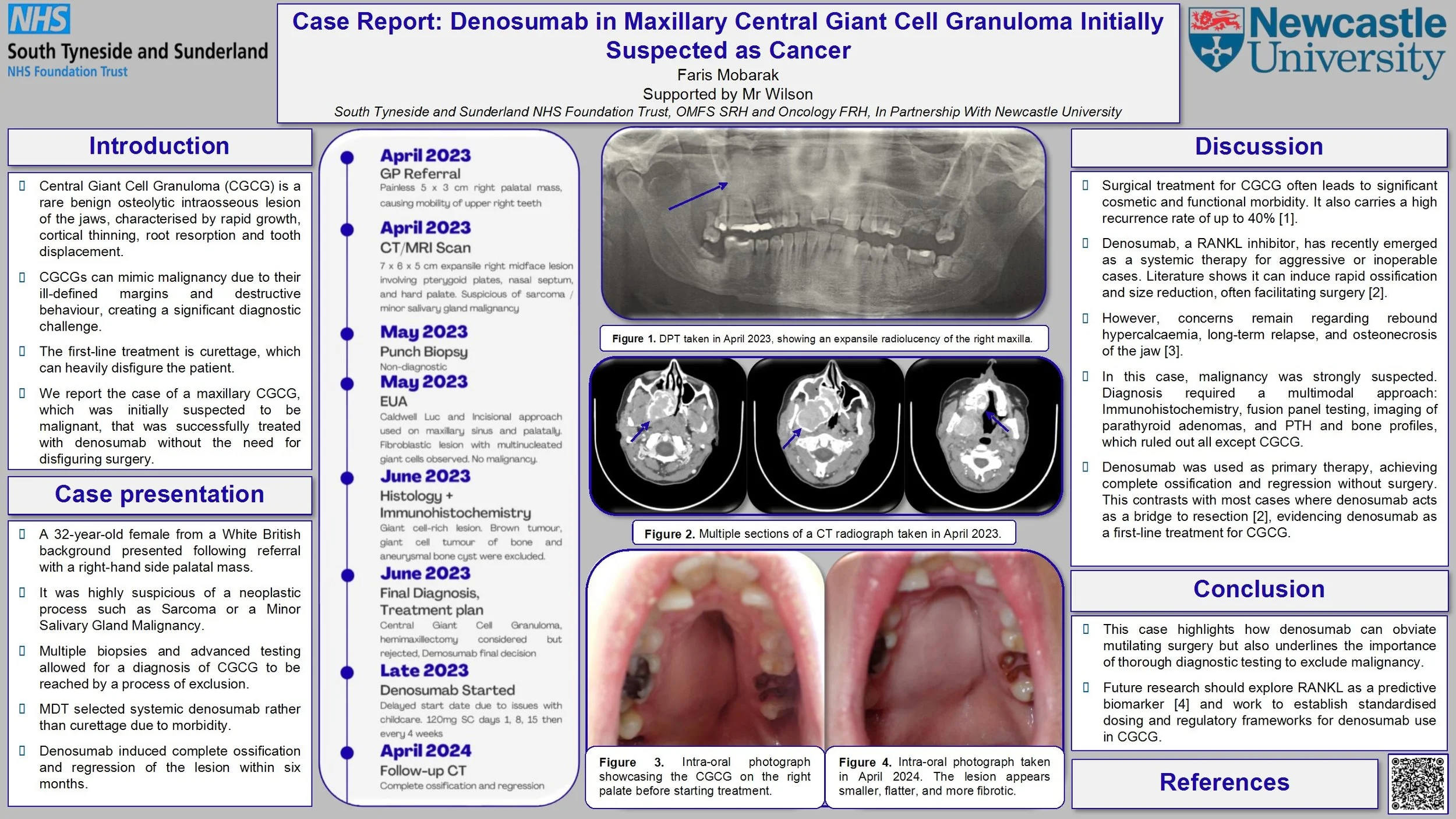
Case Report: Denosumab in Maxillary Central Giant Cell Granuloma Initially Suspected as Cancer
Introduction: Central Giant Cell Granuloma (CGCG) is a benign osteolytic lesion of the jaw that can present with aggressive radiographic features such as cortical thinning, root resorption, tooth displacement, and ill-defined margins that mimic malignancy and risk misdiagnosis. While surgical management remains the first-line therapy for CGCG, this case covers the use of denosumab, which successfully prompted ossification and lesion regression without the need for disfiguring surgery.
Case Report: We report the unusual case of a 32-year-old Caucasian female who presented in April 2023 at an emergency dental appointment with a 5 x 3 cm firm, non-ulcerated right palatal mass and mobile upper right molars. CBCT and MRI demonstrated an ill-defined, expansile, vascular lesion of the right maxilla invading the sinus, nasal floor and pterygoid plates without orbital or intracranial extension. Deep biopsies were taken under GA via Caldwell-Luc and palatal incision. Histology reported a fibro-cellular stroma with numerous osteoclast-type giant cells. Giant cell tumour of bone, aneurysmal bone cyst and brown tumour were excluded by immunohistochemistry testing and blood tests. A multidisciplinary team (MDT) discussion confirmed the diagnosis of CGCG. Given the lesion’s size and location, systemic therapy with denosumab was initiated. Multiple CT scans indicated progressive ossification and reduction in lesion volume following administration of denosumab. At a 12-month follow-up after discontinuation of treatment, the lesion remained stable, with preserved dentition and no functional or aesthetic deficits.
Discussion: Our case illustrates the diagnostic dilemma in CGCG, necessitating deep surgical biopsy, comprehensive immunohistochemistry, and multidisciplinary team coordination to rule out malignancy. It also demonstrates denosumab as an effective, tissue-sparing alternative to the extensive resection typically carried out.
Re-audit of time to surgery for mandibular fractures following implementation of the Head and Neck Assessment Hub (HANAH)
Introduction
Recent studies have shown that delays in the treatment of mandibular fractures are not associated with adverse outcomes, and this has challenged the common practice of recommending treatment within 24 hours. However, the BAOMS Trauma Special Interest Group advocates early operation to facilitate prompt discharge. We aim to analyse the time from admission to operation of mandibular fractures and identify any reasons for delays.
Method
Retrospective data was collected from records of all admitted mandible fractures over a 3 month period between May and July in 2022, 2023 and 2025 from a major trauma hospital. Time from admission to operation was measured and compared to the standard that 100% of mandibular fractures will undergo open reduction and internal fixation (ORIF) within 48 hours of admission. Data collected also included: patient demographics, other injuries, theatre type, complications and discharge time.
Results
77% (10/13), 79% (15/19) and 76% (13/17) of mandible fractures underwent ORIF within 48 hours of admission over the same 3 month period in 2022, 2023 and 2025 respectively. The mean, median and range of time to undergo ORIF from admission for: 2022 was 36.5 hours, 27 hours, 11-100 hours respectively; 2023 was 40.4 hours, 19 hours, 0-282 hours respectively; 2025 was 26.7 hours, 19 hours, 5-63 hours respectively. There were 0, 4 and 6 post-operative complications over the 3 month period in 2022, 2023 and 2025 respectively.
Conclusion
The set standard was not met and the proportion of mandible fractures that underwent operation within 48 hours of admission over the years is consistently around 76-79%. Unlike previous years, 3 of the cases that underwent operation over 48 hours in 2025 had post-operative complications. We will continue to monitor to see if a dedicated trauma list would be indicated.
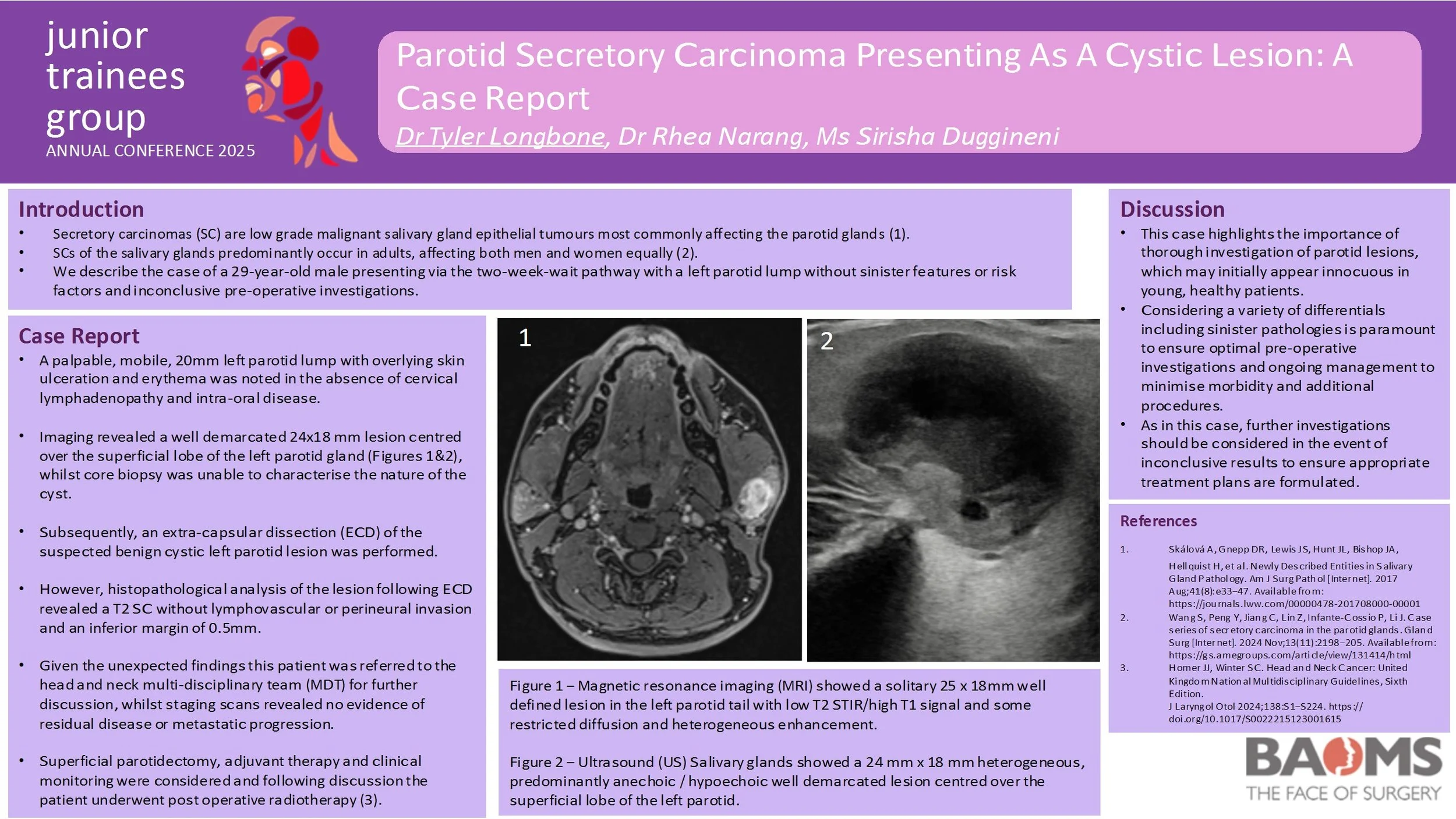
Parotid Secretory Carcinoma Presenting As A Cystic Lesion: A Case Report
Introduction:
Secretory carcinomas are low grade malignant tumours which most commonly affect the parotid glands. This report describes the case of a 29-year-old male presenting via the two-week-wait pathway with a left parotid lump without sinister features, risk factors and inconclusive pre-operative investigations. The option to pursue further lesion characterisation was discussed, however the patient elected to undergo treatment for the likely benign cystic lesion which was unexpectedly found to be a secretory carcinoma.
Case Report:
On review a palpable, mobile, 20mm left parotid lump with overlying skin ulceration and erythema was noted in the absence of cervical lymphadenopathy and intra-oral disease. Pre-operative imaging revealed a well demarcated 24x18 mm lesion centred over the superficial lobe of the left parotid gland, whilst core biopsy was unable to characterise the nature of the cyst. However, histopathological analysis of the left parotid lesion following extra-capsular dissection revealed a T2 secretory carcinoma without lymphovascular or perineural invasion and an inferior margin of 0.5mm. Subsequent staging scans did not demonstrate evidence of residual disease or metastatic progression.
This patient initially underwent extra-capsular dissection of the suspected benign cystic left parotid lesion. Given the unexpected histopathological findings this patient was referred to the head and neck multi-disciplinary team (MDT) for further discussion. Superficial parotidectomy, adjuvant therapy and clinical monitoring were considered and following discussion the patient underwent post operative radiotherapy.
Discussion:
This case highlights the importance of thorough investigation of parotid lesions, which may initially appear innocuous in young, healthy patients. Undoubtedly, considering a variety of differentials including sinister pathologies is paramount to ensure optimal pre-operative investigations and ongoing management to minimise morbidity and additional procedures.
Orbital Roof Reconstruction Utilizing Inverted Orbital Floor Plates - A Case-Based Technical Note
Background: Orbital roof fractures are rare [1] but significant injuries resulting from high-energy trauma, often alongside complex maxillofacial injuries [2,3]. Surgical repair is indicated for displaced fractures with neurological or ophthalmic compromise [4]. Traditional reconstruction with titanium mesh presents challenges such as insufficient rigidity, sharp edges, implant extrusion risk, and difficulty of removal if infected. As such, we propose using pre-shaped orbital floor plates, inverted for orbital roof reconstruction, offering improved structural support and a more ergonomic surgical experience.
Methods: Retrospective case series (n=4) of patients undergoing surgical repair for orbital roof fractures. A bicoronal and pericranial flap was raised, followed by hemifrontal craniotomy. Orbital roof defects were visualised, dural tears repaired, and reconstruction performed using inverted orbital floor plates secured with screws. A pericranial flap covered the repair, and the bone flap was re-fixed with low-profile plating. Postoperative outcomes were assessed.
Results: All cases achieved correct orbital roof alignment and restoration of orbital volume. No implant-related infections were found. Progressive recovery or complete resolution of ocular symptoms was observed, even in severe trauma patients.
Discussion: This case series demonstrates the feasibility, safety, and structural adequacy of using inverted orbital floor plates for orbital roof reconstruction. This alternative offers greater rigidity, easier handling, anatomical contour matching and immediate availability in trauma settings, with good outcomes even in severe trauma. Study limitations include small sample size due to the rarity of the fracture, heterogeneous trauma profiles, and limited long-term follow-up. Therefore, further studies are needed to confirm long-term outcomes.
The use of dermal matrices in the reconstruction of defects following the resection of oral potentially malignant disorders: a scoping review
Introduction:
Dysplasia and oral potentially malignant disorders (OPMDs) of the oral cavity often require surgical resection to prevent malignant transformation. These lesions are frequently left to heal by secondary intention, exposing patients to discomfort and an increased risk of post-operative infection. Dermal matrices offer a promising reconstructive alternative, providing biocompatibility and favourable healing outcomes. However, their clinical use in this specific context has not yet been comprehensively reviewed. This scoping review aims to systematically map and critically appraise the current evidence on the use of dermal matrices in reconstructive surgery following resection of dysplastic lesions and OPMDs of the oral cavity, and to identify current evidence, innovation, and gaps in knowledge.
Methods:
A scoping review was conducted following the PRISMA-ScR guidelines. The electronic databases PubMed, Scopus and Medline were searched without date restrictions. Grey literature was also explored via Google Scholar. Two reviewers independently screened the articles, with discrepancies resolved by a third reviewer. Data were extracted on factors such as study design, type of dermal matrix used, surgical outcomes and disease recurrence.
Results:
From an initial yield of 6229 titles, 25 studies met the inclusion criteria. These involved various dermal matrix types, including acellular human dermal matrices and bovine-derived collagen scaffolds. Most studies reported satisfactory integration and minimal complications. However, heterogeneity in study design, outcome measures, and follow-up limited direct comparisons. Few studies specifically addressed long-term recurrence or malignant transformation post-reconstruction.
Conclusion:
Dermal matrices may represent a viable and increasingly utilised option for reconstructing defects following the resection of dysplasia and OPMDs of the oral cavity. While this review highlights early successes, it also underscores key limitations in the existing literature and calls for targeted research to validate dermal matrices as a standard reconstructive strategy in oral oncology.
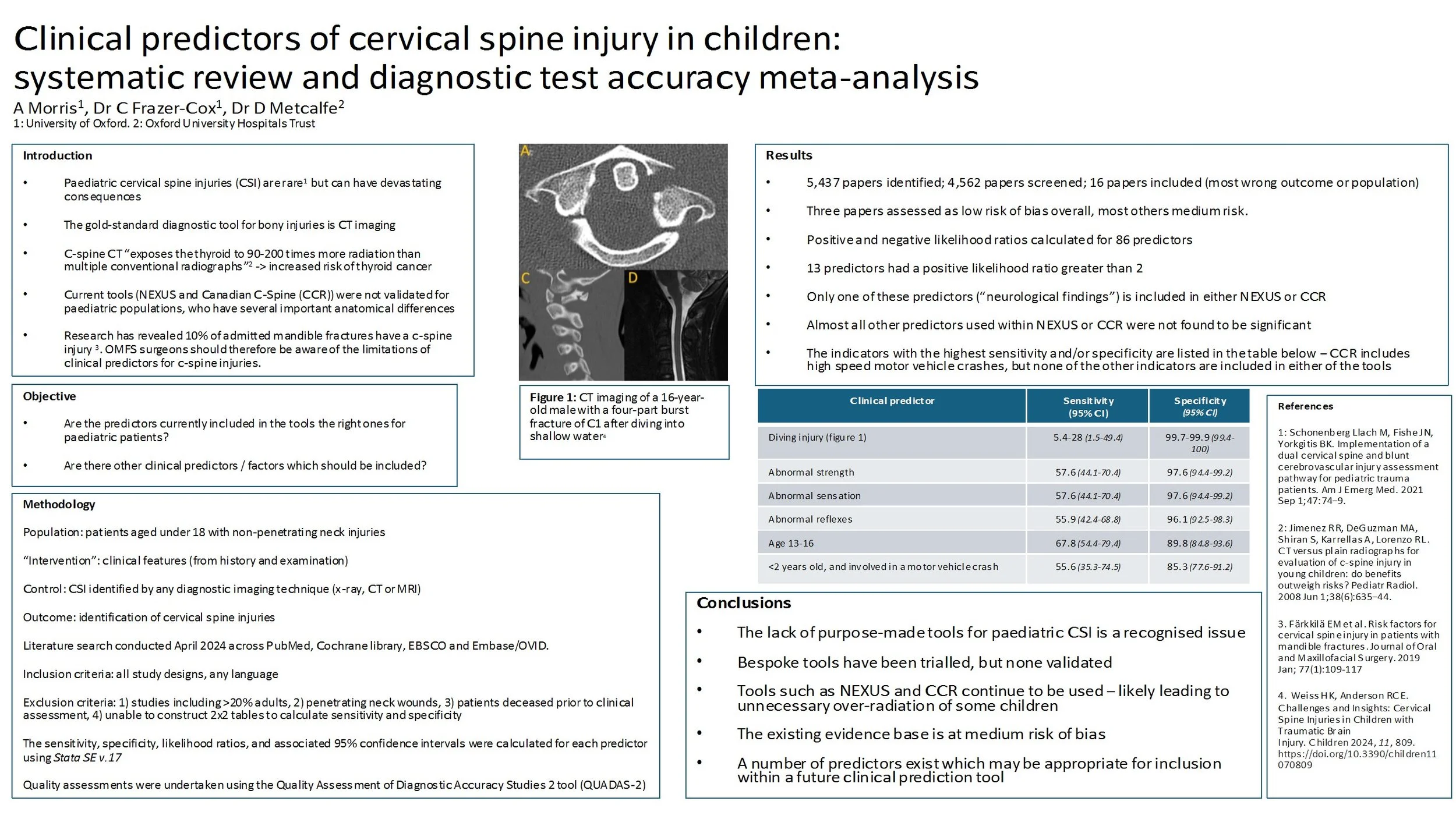
Clinical predictors of cervical spine injury in children: systematic review and diagnostic test accuracy meta-analysis
Introduction: Clinical decision rules for identifying which cervical spine injuries (CSI) require diagnostic radiography were validated in adult populations, whose necks are anatomically very different to those of children. Their accuracy in children is unclear. This review sought to identify clinical predictors of non-penetrating CSI in children and propose candidates for a modified decision tool.
Method: A systematic review and meta-analysis of diagnostic test accuracy studies that evaluated the ability of clinical features to identify CSI in patients younger than 18 years old. The search was conducted on 18 April 2024. Language limits were not applied. All traumatic, non-penetrating neck injuries were included, except where patients died due to their injuries prior to clinical assessment. The sensitivity, specificity, likelihood ratios, and associated 95% confidence intervals were reported for each predictor. Data reported by three studies was pooled using univariate random effects models, and those with four or more studies used multi-level mixed effects logistic regression models. Quality assessments were undertaken using the Quality Assessment of Diagnostic Accuracy Studies 2 tool.
Results: 16 studies reported on 9926 CSI. The most important potential source of bias was unclear/inconsistent utilisation of reference standard tools during patient assessment. The most useful clinical predictors were abnormal strength, sensation or reflexes, and age 13-16. The most important mechanisms of injury were diving, children under 2 years old involved in a motor vehicle crash, and firearms.
Conclusion: The existing evidence base is at moderate risk of bias. Predictors in existing clinical rules, validated in adults (e.g. NEXUS and CCR), often do not include good diagnostic characteristics for children. It is therefore possible that these rules do not perform as effectively in paediatric populations as in adults. A number of predictors exist that are potential candidates for inclusion within a future clinical prediction rule for paediatric CSI.
Connecting Patients and Providers: A Quality Improvement Initiative in Head and Neck Cancer Care
Introduction
Patients with head and neck cancer are often treated across multiple hospitals, leading to confusion about appointments, treatment stages, and who to contact. This quality improvement project aimed to improve communication by introducing a clear, unified leaflet outlining the full treatment pathway. The project involved trusts in London and Essex, with UCLH as the central site for surgery.
Methodology
The leaflet was co-developed with input from consultants, clinical nurse specialists, and admin staff from UCLH, Queen’s, and the Royal London Hospital. It explained each step of the patient journey from diagnosis to surgery and follow-up and was translated into several languages to reflect local populations. Patients received the leaflet at pre-assessment and were asked to complete a six-question survey before and an eight-question survey after reading it.
Results
Survey results were on a scale from 1-5 and displayed marked improvements. Familiarity with the care process rose from an average of 2.3 to 4.2. Confidence in navigating appointments and services improved from 2.1 to 4.1. Understanding of treatment stages increased from 2.4 to 4.3. Clarity around locations and contact points also improved. More than 90% of patients rated the leaflet as clear and helpful. At £50 per 1000 copies, the leaflet was low-cost. Challenges included translation funding, legal permissions, and coordination between sites, though these were manageable.
Conclusion
This QIP offers a simple, scalable solution to a common communication gap in cancer care. By creating a multilingual, patient-friendly resource in both print and digital formats, the project has improved patient understanding and pathway navigation. Future work will assess long-term effects on patient satisfaction and whether the approach can be expanded to other specialties.
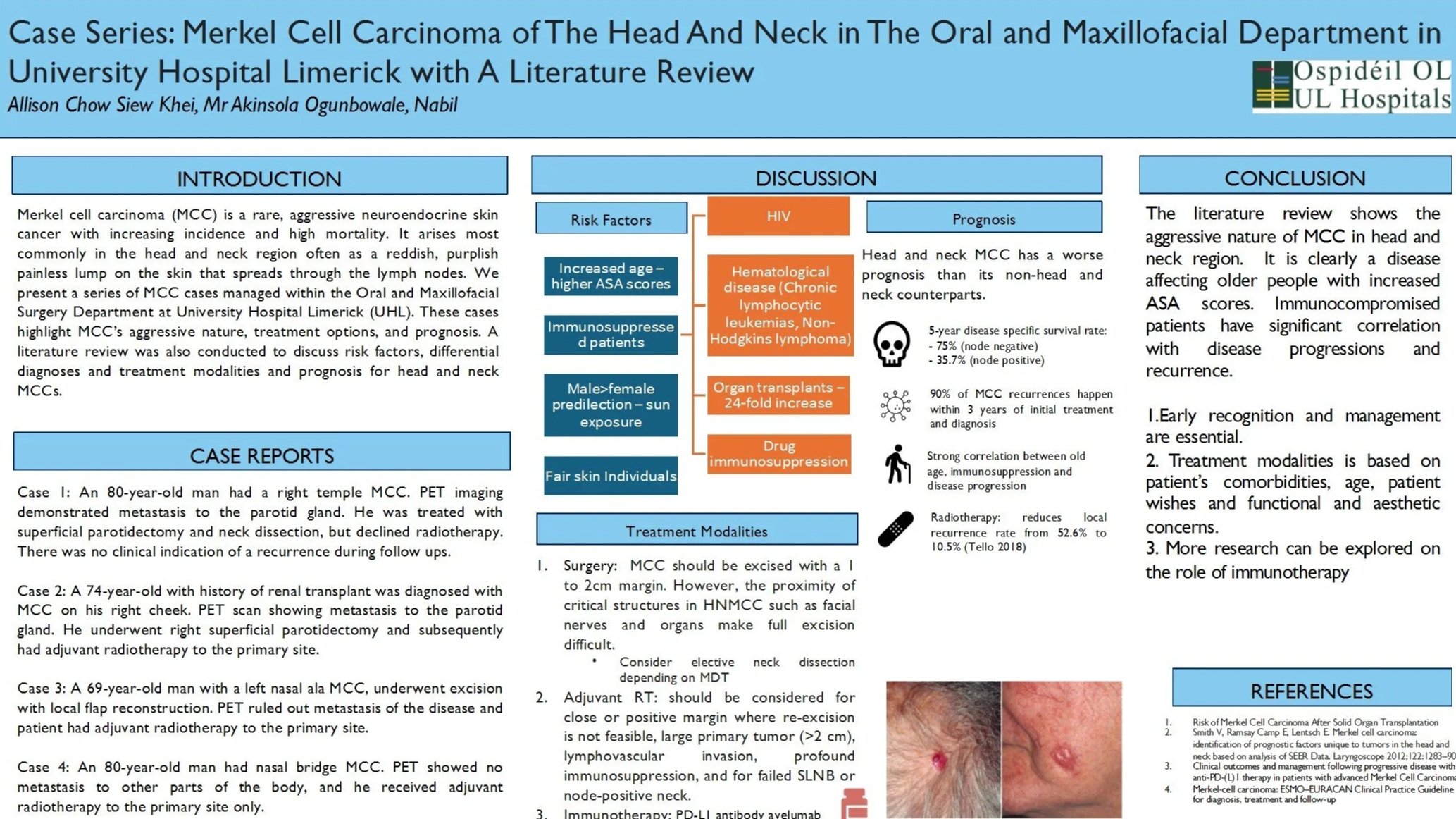
Case Series: Merkel Cell Carcinoma of The Head And Neck in The Oral and Maxillofacial Department in University Hospital Limerick with A Literature Review
Introduction
Merkel cell carcinoma (MCC) is a rare, aggressive neuroendocrine skin cancer with increasing incidence and high mortality. Early recognition and management are essential. We present a series of MCC cases managed within the Oral and Maxillofacial Surgery Department at University Hospitals Limerick (UHL). These cases highlight MMC’s aggressive nature, treatment options, and prognosis.
Case Reports
Case 1: A 74-year-old man diagnosed with right cheek MCC with metastatic to the parotid gland. He underwent right superficial parotidectomy followed by chemo-radiotherapy.
Case 2: An 80-year-old man had a right temple MCC. PET imaging demonstrated metastasis to parotid. He was treated with superficial parotidectomy and neck dissection, but declined radiotherapy.
Case 3: A 69-year-old man with an left nasal ala MCC, underwent excision with local flap reconstruction. PET ruled out metastasis of the disease and he received adjuvant radiotherapy to the primary site.
Case 4: An 80-year-old man had an nasal bridge MCC. PET showed no metastasis, and he received adjuvant radiotherapy to the primary site only.
Discussion
MCC is an uncommon but highly aggressive cutaneous malignancy, most often arising on the head and neck. Risk factors include immunosuppression, with solid organ recipients carrying a 24-fold increased risk. Surgery is the mainstay of treatment, usually followed by adjuvant radiotherapy. Chemotherapy is reserved for advanced disease, while immunotherapy is an emerging and promising option.
Conclusion
MCC is rarely suspected clinically but is rapidly becoming more common. Imaging, particularly PET, should be considered where clinically indicated. Management typically involves surgery with adjuvant radiotherapy; chemotherapy and immunotherapy may be considered in metastatic or recurrent disease. Further studies surrounding knowledge of disease progression and management, should be carried out
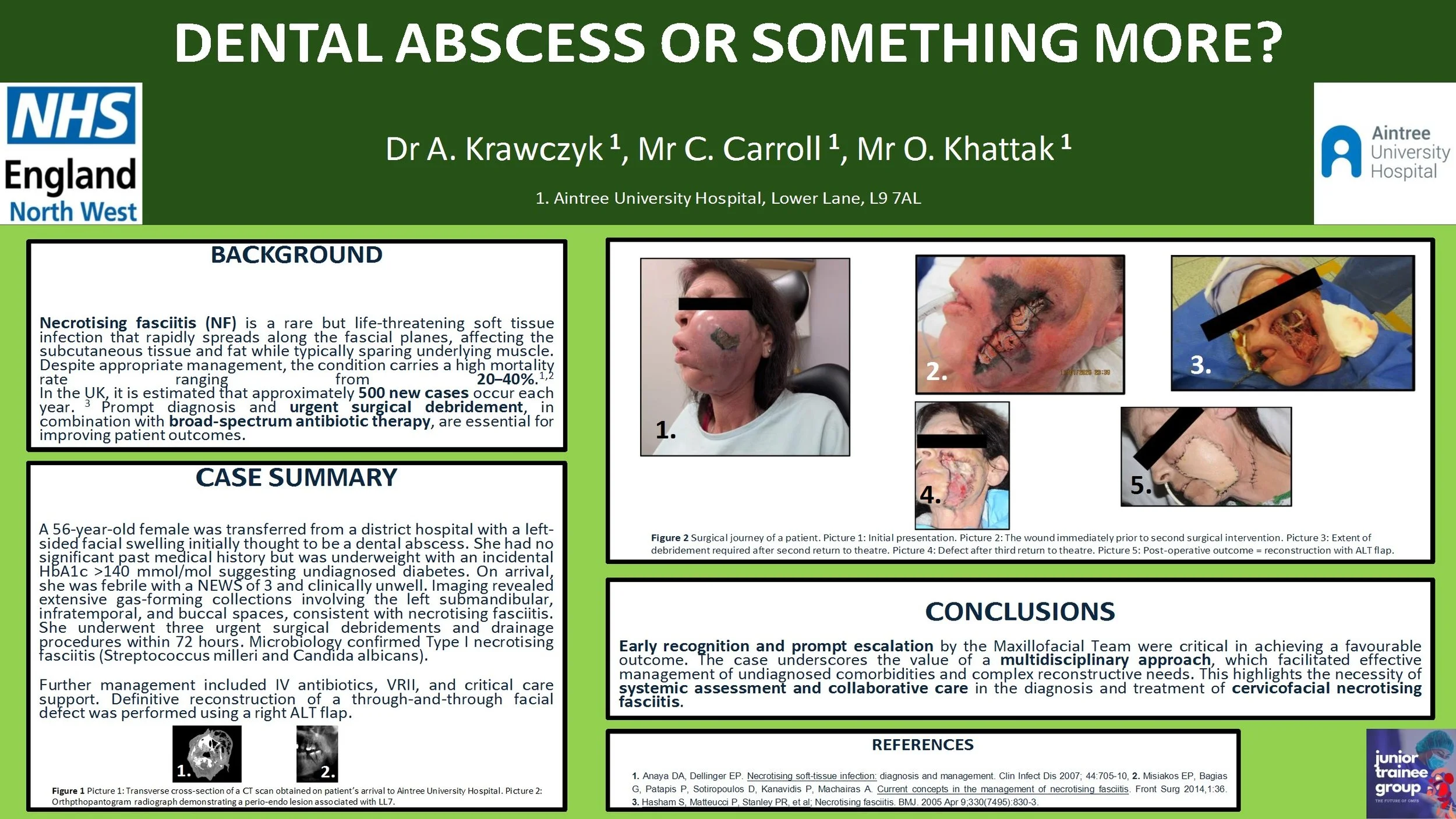
Dental abscess or something more?
Introduction:
Necrotising fasciitis is a rare, rapidly progressive soft tissue infection with high morbidity and mortality, often polymicrobial (Type I) and associated with immunocompromised states. Prompt recognition and aggressive surgical management are essential.
Case report:
A 56-year-old female was transferred from a district hospital with a left-sided facial swelling initially thought to be a dental abscess. She had no significant past medical history but was underweight with an incidental HbA1c >140 mmol/mol suggesting undiagnosed diabetes. On arrival, she was febrile with a NEWS of 3 and clinical unwell. Imaging revealed extensive gas-forming collections involving the left submandibular, infratemporal, and buccal spaces, consistent with necrotising fasciitis. She underwent three urgent surgical debridements and drainage procedures within 72 hours. Microbiology confirmed Type I necrotising fasciitis (Streptococcus milleri and Candida albicans). Further management included intravenous antibiotics, variable rate insulin infusion, and critical care support. Definitive reconstruction of a through-and-through facial defect was performed using a right antero-lateral thigh free flap.
Discussion:
Early recognition and escalation by the on-call Maxillofacial team were key to successful outcomes. A multidisciplinary approach enabled management of complex comorbidities and reconstruction. This case highlights the importance of systemic evaluation and team-based care in managing cervicofacial necrotising fasciitis.