Cross Covering ENT As An OMFS SHO
Author - Imran Aziz
“Hello, just answering the ENT bleep.. this is the sleep-deprived dentist speaking - how can I help.”
Most reading this will have experienced feeling out of your depth as dentists new to working in OMFS. Toss in ENT cross-cover and it’s a whole other story. The reality being that regularly overnight, I am said SHO answering every bleep about bleeding, blocked airways and small children who have inhaled bits of plastic shaped like cartoon cats.
For the last four years at Sunderland Royal I’ve worked in maxillofacial surgery. This unfortunately means looking after an additional 10-15 (often quite unwell) ENT inpatients, A&E majors and minors, paediatrics and referrals from the neighbouring units. Fortunately with a very supportive bunch of ENT seniors never more than 40 minutes away.
Alongside our usual maxillofacial surgery duties, most nights follow roughly the same script. The bulk of my work falling into a few familiar buckets.
Bleeding
Epistaxis ranging from the mild ooze to those anticoagulated with bilateral nasal packs yet still gushing. Bleeding tracheostomy sites. And the cold dread of a post‑tonsillectomy bleed who vomits up their circulating volume in front of you.
Airway
From quinsy’s to blocked tracheostomies. Or the epiglottitis which has everyone quietly asking the same question - “how long before this gets bad?”.
Infection and other complications
Tonsilitis, mastoiditis, necrotising otitis externa, periorbital cellulitis, angry post‑op necks, developmental defects and pinna or septal haematomas that arrive just as you dip your complimentary NHS custard cream into a brew.
Kids and foreign bodies
Be it button batteries, magnets, beads or Lego heads evading the mothers kiss whilst nestled in a tiny nostril, ear canal or throat. These can present as real emergencies and require a degree of skill to manage appropriately.
In the beginning, most situations came with a reflexive phone call to the ENT registrar. A few months in and a fair amount of night‑time corridor teaching, that all changed. You learn quickly what you can handle and what absolutely must trigger your “phone a friend” reflex.
On occasion a late running endocrine case may leave you having to chase a patients PTH bloods – most trusts have excellent flow charts to help you puzzle your way through this.
The Hello Kitty GA that wasn’t
One memorable call 2 months in was my first paediatric foreign body. An unfortunate right nostril now home to a rubber Hello Kitty. Lodged just far enough back to be a risk but just close enough to make a trip to theatre feel like overkill.
The scene: 2am in Paeds ED. Arriving to an extremely unimpressed three‑year‑old, an exhausted nurse, a panicked mum holding it together, and me. Armed with a pair of crocs, a pen torch placed strategically between my teeth and a pair of those nasal speculums everyone forget the name of. With some calm chat, gentle manoeuvring and a lot of snot later, the foreign body was secured. No GA, some drama, a surprisingly chilled child and one very relieved mum.
What I learned: managing paediatric foreign bodies are as much about managing parents and expectations as they are about technique. A steady voice and a plan will often do more good than yanking aimlessly.
A 3am FNE jumpscare
Then there are the quieter moments that stay with you for different reasons. Late into another shift, I took a call from an ED registrar “Re-presentation with food bolus, dysphagia, buscopan hasn’t helped, she’s been here 6 hours could you cast an eye?” The patient a young lady - stable, chatting, just “quite uncomfortable”. A dash of lidocaine spray and out comes the scope. On paper, this was a quick win, scope, call the gastro consultant, organise endoscopy for the next day, more buscopan and bed.
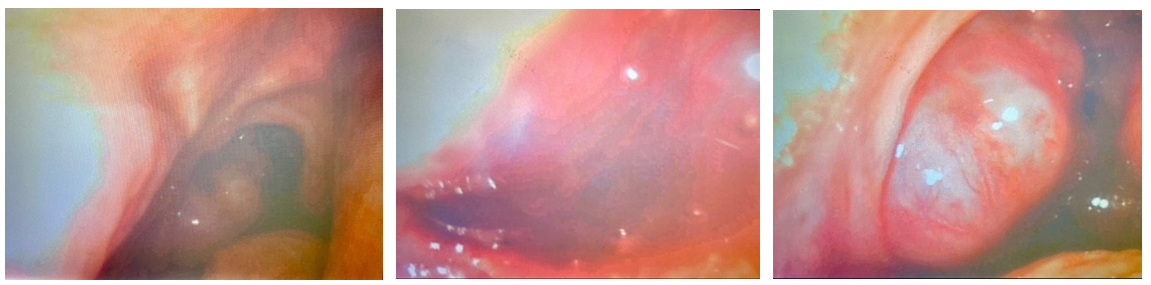
There I was admiring some nasal turbinates, when, instead of a neat little bolus something strange catches my eye. Once the saliva had cleared a large mass was revealed in the pharynx. The kind of pathology you expect to see in clinic or on an MDT list, not ED in the middle of the night with you as the first doc to spot it.
That night I realised cross‑cover isn’t just all feeling sorry for patients whilst inflating that second rapid rhino. It could be catching something capable of changing a patient’s entire trajectory, and doing so whilst there isn’t a consultant standing at your shoulder.
The Stridulous alarm clock
Nothing quite rubs the sleep from your eyes like waking to a bleep with audible stridor in the back-ground.
Those are the moments when friends in high places matter. Early calls to anaesthetics, ICU, seniors and experienced nurses are the difference between a slick, well‑run airway emergency and a slow‑motion car crash. Getting to know them by daylight makes the 4am call much easier. It’s surprisingly calmer scoping a narrowing airway when the anaesthetics reg is on hand. Also a big plus knowing your second-on is awake, putting on his trousers and driving as fast as he legally can to help you out.
What Max-Fax brings to ENT nights
Cross‑covering ENT was initially daunting but truly has been a crash‑course in areas of medicine that really matter when the sun goes down.
Our undergraduate training and practical understanding of head and neck anatomy sets us apart from some medically qualified colleagues. Being independent practitioners experienced in delivering painless local anaesthetic, and dealing with suctions‑that‑won’t‑suck puts us in good stead when faced with most situations A&E throw at you.
The other big lesson. You learn quickly to tolerate being out of your comfort zone and how to ask for help appropriately.
Survival tips for the accidental ENT SHO
If you find yourself in a similar role, these are my top tips.
Never be embarrassed to admit early doors you haven’t seen something before. Seniors far prefer an honest “talk me through this” at midnight to a panicked muddle at 3am.
Practice fibre‑nasendoscopy in hours with someone competent beside you; it’s a different experience when the corridor is quiet and nobody is desaturating.
Make anaesthetics and ICU your friends long before you need them. They are your safety net when help is speeding down the motorway.
Download and use the ENTSHO app. It is the unofficial co‑pilot for every new ENT SHO (and for the MaxFax SHO masquerading as one).
Trust your skillset. As dentists and OMFS trainees, you are often several steps ahead of inexperienced F2’s who rarely look inside of mouths, let alone stuck needles in there.
True, there may be more medical headaches but they soon become the Med Reg’s headache. The depth of experience you gain in airway management, acute head and neck pathology and teamworking is, frankly, gold. I would encourage anyone to give it a go.
If I ever go on to receive a Pulitzer prize for this piece of literary genius.. The following apps will receive special mention in my acceptance speech for getting me through.