JTG 2025 Poster Gallery
Dental abscess or something more?
Introduction:
Necrotising fasciitis is a rare, rapidly progressive soft tissue infection with high morbidity and mortality, often polymicrobial (Type I) and associated with immunocompromised states. Prompt recognition and aggressive surgical management are essential.
Case report:
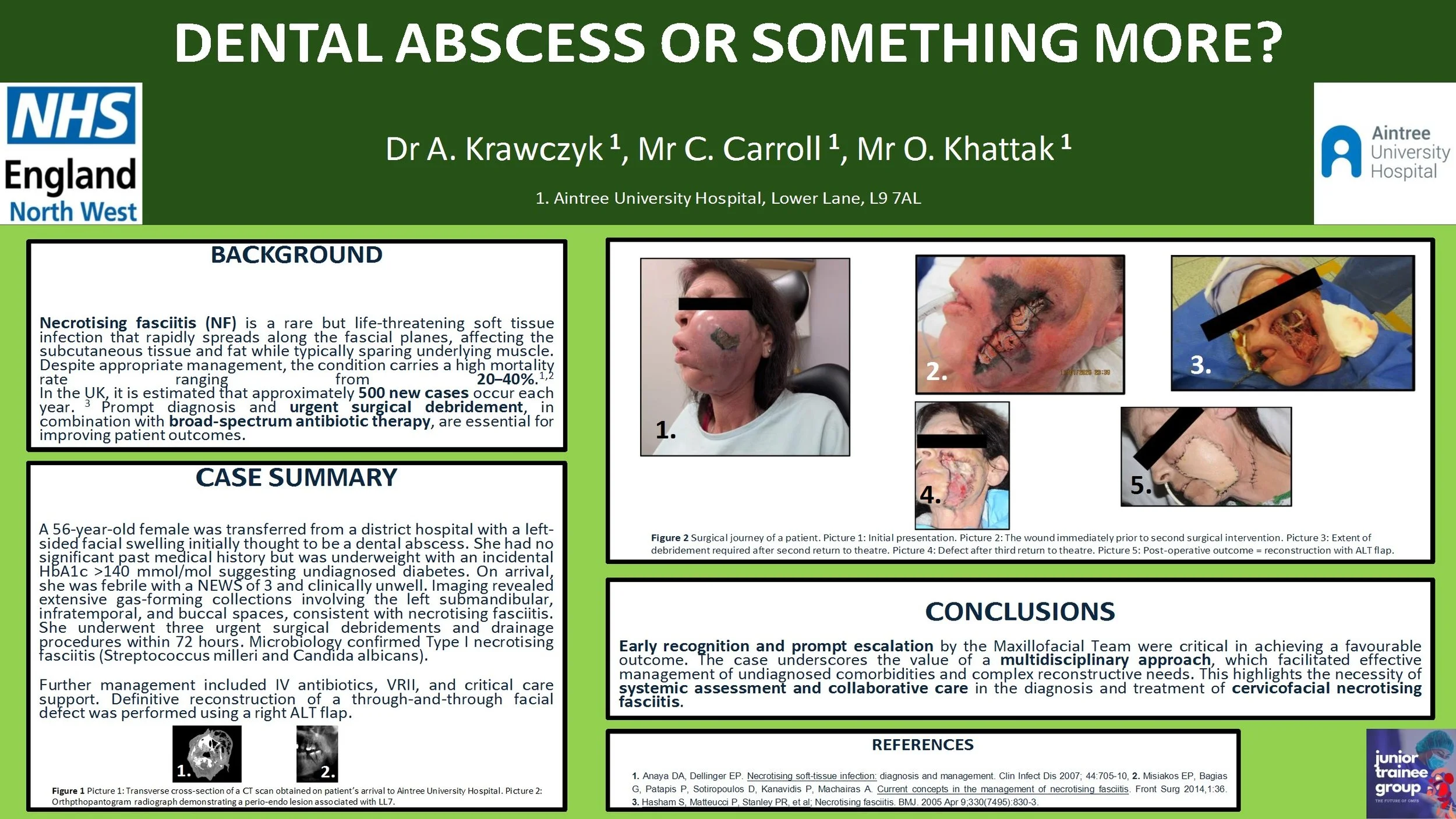
A 56-year-old female was transferred from a district hospital with a left-sided facial swelling initially thought to be a dental abscess. She had no significant past medical history but was underweight with an incidental HbA1c >140 mmol/mol suggesting undiagnosed diabetes. On arrival, she was febrile with a NEWS of 3 and clinical unwell. Imaging revealed extensive gas-forming collections involving the left submandibular, infratemporal, and buccal spaces, consistent with necrotising fasciitis. She underwent three urgent surgical debridements and drainage procedures within 72 hours. Microbiology confirmed Type I necrotising fasciitis (Streptococcus milleri and Candida albicans). Further management included intravenous antibiotics, variable rate insulin infusion, and critical care support. Definitive reconstruction of a through-and-through facial defect was performed using a right antero-lateral thigh free flap.
Discussion:
Early recognition and escalation by the on-call Maxillofacial team were key to successful outcomes. A multidisciplinary approach enabled management of complex comorbidities and reconstruction. This case highlights the importance of systemic evaluation and team-based care in managing cervicofacial necrotising fasciitis.