JTG 2025 Poster Gallery
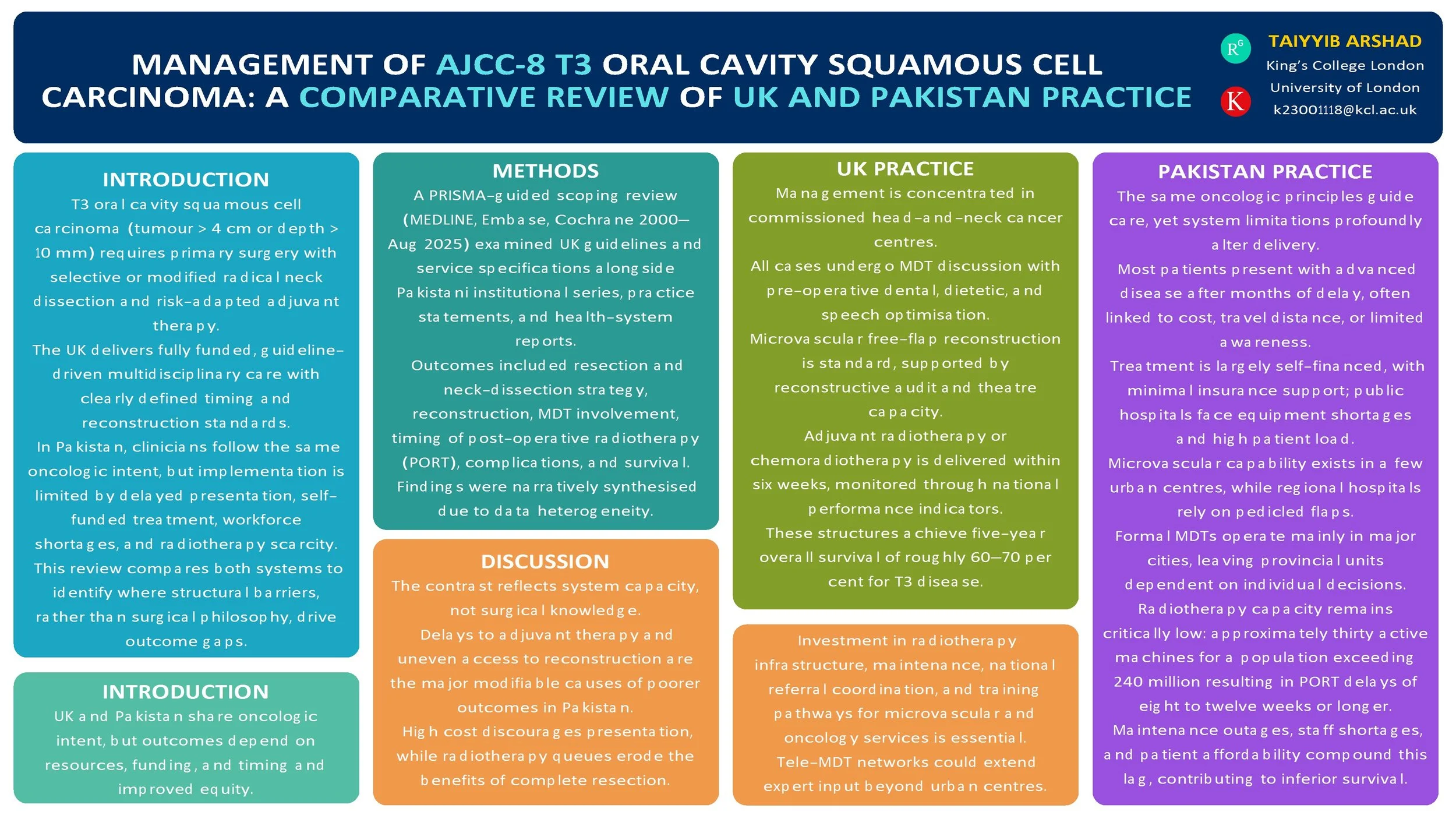
Management of AJCC-8 T3 Oral Cavity Squamous Cell Carcinoma: A Comparative Review of UK (NICE) and Pakistan Practices
Introduction
T3 oral cavity squamous cell carcinoma (OCSCC; AJCC-8: tumour > 4 cm or depth of invasion > 10 mm) is managed with primary surgery and risk-adapted adjuvant therapy. The UK delivers guideline-driven multidisciplinary care, while Pakistan applies the same oncologic principles within more heterogeneous resource settings. We compared published guidance and real-world practice to identify convergences, gaps, and opportunities for pathway improvement.
Method
PRISMA-guided scoping review (MEDLINE, Embase, Cochrane, and grey literature, 2000–Aug 2025). We included: (i) UK guidelines/standards for oral cavity cancer; (ii) Pakistan institutional series and practice statements for T3 OCSCC; (iii) health-system reports on multidisciplinary team (MDT) availability and radiotherapy capacity. Outcomes: resection and neck-dissection strategy, reconstruction modality, positive margins, time to post-operative radiotherapy (PORT), complications, recurrence, and survival. Data were charted narratively due to heterogeneity.
Results
UK sources consistently recommend upfront resection with appropriate ipsi/contralateral neck dissection, microvascular reconstruction when indicated, and adjuvant RT/CRT for adverse features, delivered through MDT pathways with staging, dental, and nutritional optimisation. Pakistan tertiary centres report adherence to core surgical principles with growing microvascular capability; regional flaps are used where resources are constrained. Across Pakistan reports, later stage at presentation is common; MDT access and radiotherapy capacity vary, contributing to PORT delays. Broader head-and-neck literature links delayed PORT (>6 weeks) with inferior outcomes. No head-to-head UK–Pakistan comparative cohort specific to T3 OCSCC outcomes was found.
Conclusion
Oncologic intent is aligned, but system-level factors—MDT coverage, reconstructive resources, and timely access to PORT—likely drive differences in delivered care and outcomes. Standardised, context-adapted pathways (routine MDT triage, clear neck algorithms, reconstruction choice matched to resources, and fast-tracked PORT) and a bi-national registry focused on T3 OCSCC are warranted to benchmark timing, treatment patterns, and outcomes.
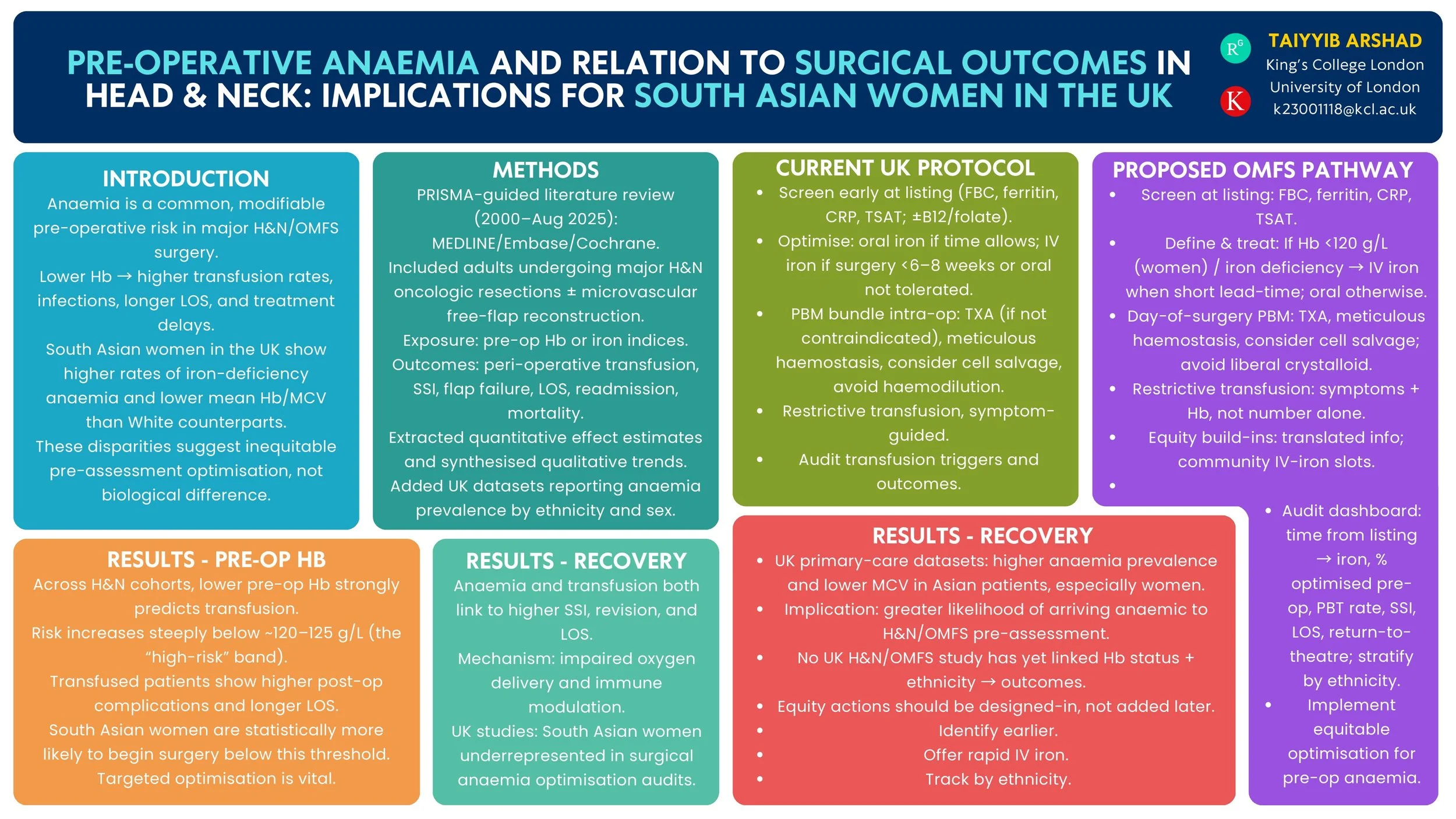
Pre-operative Anaemia and Surgical Outcomes in Head & Neck Surgery: Implications for South Asian Women in the UK
Introduction
Pre-operative anaemia is a modifiable risk factor that increases complications after head & neck (H&N) surgery. UK primary-care data show a higher burden of anaemia among women of Asian heritage than White women. We reviewed the evidence on pre-operative anaemia and H&N/OMFS surgical outcomes and summarised UK epidemiology by ethnicity to inform equity-focused peri-operative pathways.
Method
PRISMA-guided review (MEDLINE/Embase/Cochrane, 2000–Aug 2025). Inclusion: studies of H&N/OMFS surgery reporting pre-operative haemoglobin/iron indices vs peri-operative outcomes (transfusion, surgical-site infection, return to theatre, flap failure, length of stay, readmission, mortality, oncological endpoints). We additionally summarised UK population/primary-care studies reporting anaemia prevalence in women by ethnicity and current UK peri-operative anaemia guidance.
Results
Across H&N cohorts and syntheses, lower pre-operative haemoglobin independently associates with higher peri-operative transfusion and adverse outcomes; a high-risk transfusion threshold is consistently observed around ~120 g/L. UK guidance recommends routine pre-operative screening and optimisation (including intravenous iron) for major surgery. UK primary-care datasets demonstrate higher anaemia prevalence and lower mean haemoglobin/MCV among Asian compared with White patients, indicating that women of South Asian heritage are more likely to present anaemic before surgery. No UK H&N/OMFS study has yet quantified outcome differences by both anaemia status and ethnicity.
Conclusion
Robust evidence links pre-operative anaemia with worse H&N surgical outcomes, and UK datasets show higher anaemia prevalence in Asian women. These findings support a standardised OMFS/H&N anaemia optimisation pathway—early case-finding, iron studies, rapid IV iron, and transfusion-sparing strategies—with particular attention to access and uptake among South Asian women. Future UK multicentre analyses should test whether ethnicity modifies anaemia-related surgical risk and evaluate pathway impact on complications and treatment delays.