JTG 2025 Poster Gallery
What advice did second-degree students have for prospective students on reducing the impact of part-time employment on their medical education?
Introduction:
Student finance provisions for the second degree can be complex, with some finance agencies having specific policies for graduate-entry students who have previously studied medicine or dentistry. Second-degree students may take up part time employment during their studies to maintain clinical skills or to allow for the financing of their course in addition to other living costs. Doctors and dentists have several employment options available to them although these may be during unsocial hours owing to the full-time nature of medicine and dentistry courses.
Methods:
This qualitative research study investigated the impact of employment on medical education during the second degree. In addition to educational impact, also explored were the reasons for taking on employment and what advice participants may have for prospective students on minimising impact. In total, 7 participants were interviewed over Microsoft Teams, following recruitment via a social media post. Those recruited were all dentistry-first and studied medicine as the second-degree. Participants were interviewed using a standardised interview schedule.
Results:
Participants reported both positive and negative impacts of work on medical education and the primary reason for working was financial. Positive impacts included maintenance and development of clinical skills, building of professional relationships and improved teaching skills. The predominant negative impact was that of tiredness, with additional negative impacts being loss of study time and poor academic performance.
Conclusion:
Second-degree students reported positive and negative impacts to their medical education as a result of part-time work during studies. Many expressed a desire for greater financial support during the second degree. Incidental findings also revealed other impacts to the student experience unrelated to medical education.
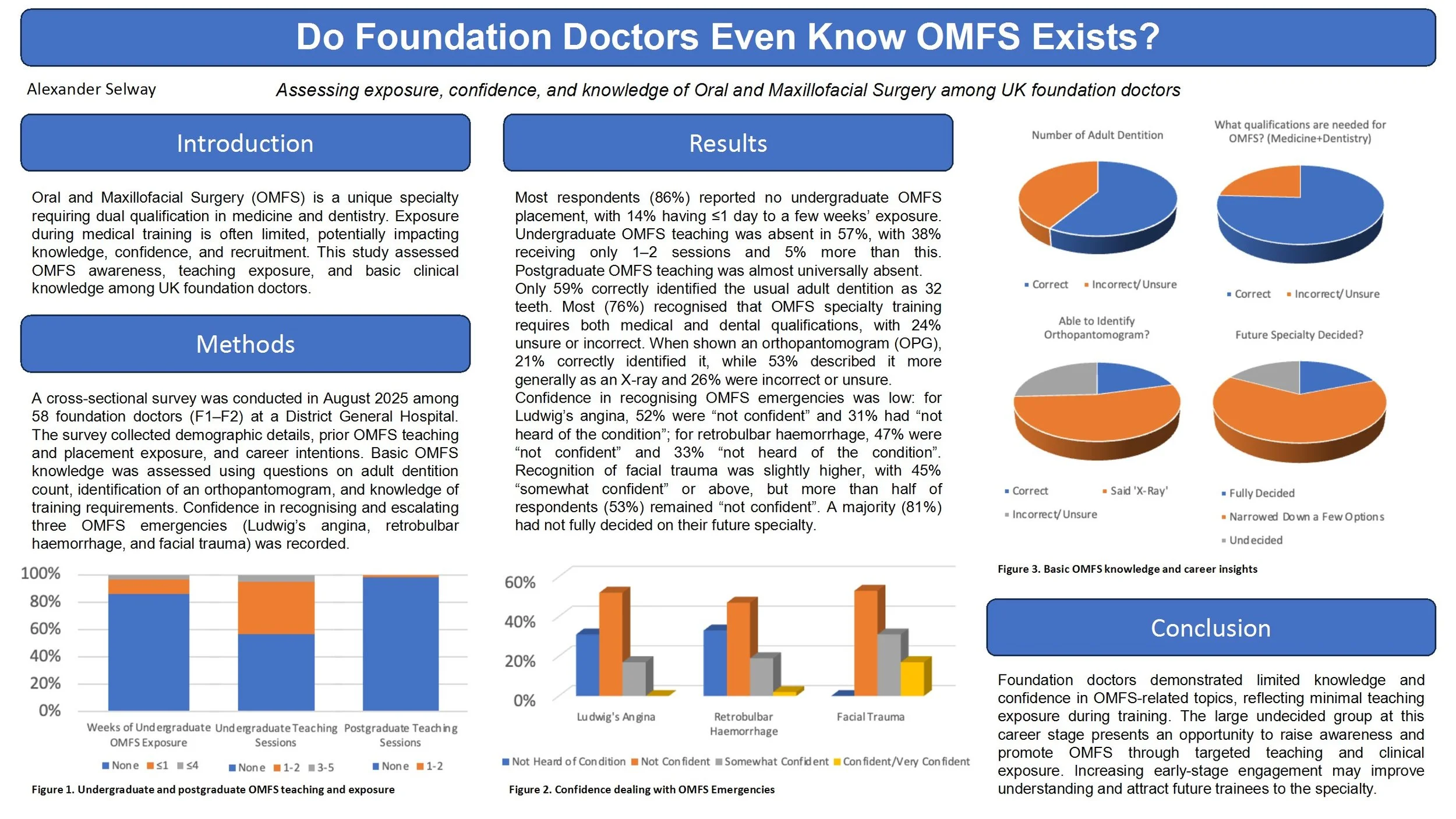
Do Foundation Doctors Even Know OMFS Exists? Assessing exposure, confidence, and knowledge of Oral and Maxillofacial Surgery among UK foundation doctors
Introduction
Oral and Maxillofacial Surgery (OMFS) is a unique specialty requiring dual qualification in medicine and dentistry. Exposure during medical training is often limited, potentially impacting knowledge, confidence, and recruitment. This study assessed OMFS awareness, teaching exposure, and basic clinical knowledge among UK foundation doctors.
Methods
A cross-sectional survey was conducted in August 2025 among 58 foundation doctors (F1–F2) at a District General Hospital. The survey collected demographic details, prior OMFS teaching and placement exposure, and career intentions. Basic OMFS knowledge was assessed using questions on adult dentition count, identification of an orthopantomogram, and knowledge of training requirements. Confidence in recognising and escalating three OMFS emergencies (Ludwig’s angina, retrobulbar haemorrhage, and facial trauma) was recorded.
Results
Most respondents (86%) reported no undergraduate OMFS placement, with 14% having ≤1 day to a few weeks’ exposure. Undergraduate OMFS teaching was absent in 57%, with 38% receiving only 1–2 sessions and 5% more than this. Postgraduate OMFS teaching was almost universally absent. Only 59% correctly identified the usual adult dentition as 32 teeth. Most (76%) recognised that OMFS specialty training requires both medical and dental qualifications, with 24% unsure or incorrect. Confidence in recognising Ludwig’s angina was low, with 52% “not confident” and 31% “not heard of condition”. For retrobulbar haemorrhage, 47% “not confident” and 33% “not heard of condition”. Facial trauma recognition had slightly higher confidence (45% “somewhat confident” or above), but more than half of respondents (53%) remained “not confident”. A majority (81%) had not fully decided on their future specialty.
Conclusions
Foundation doctors demonstrated limited knowledge and confidence in OMFS-related topics, reflecting minimal teaching exposure during training. The large undecided group at this career stage presents an opportunity to raise awareness and promote OMFS through targeted teaching and clinical exposure. Increasing early-stage engagement may improve understanding and attract future trainees to the specialty.
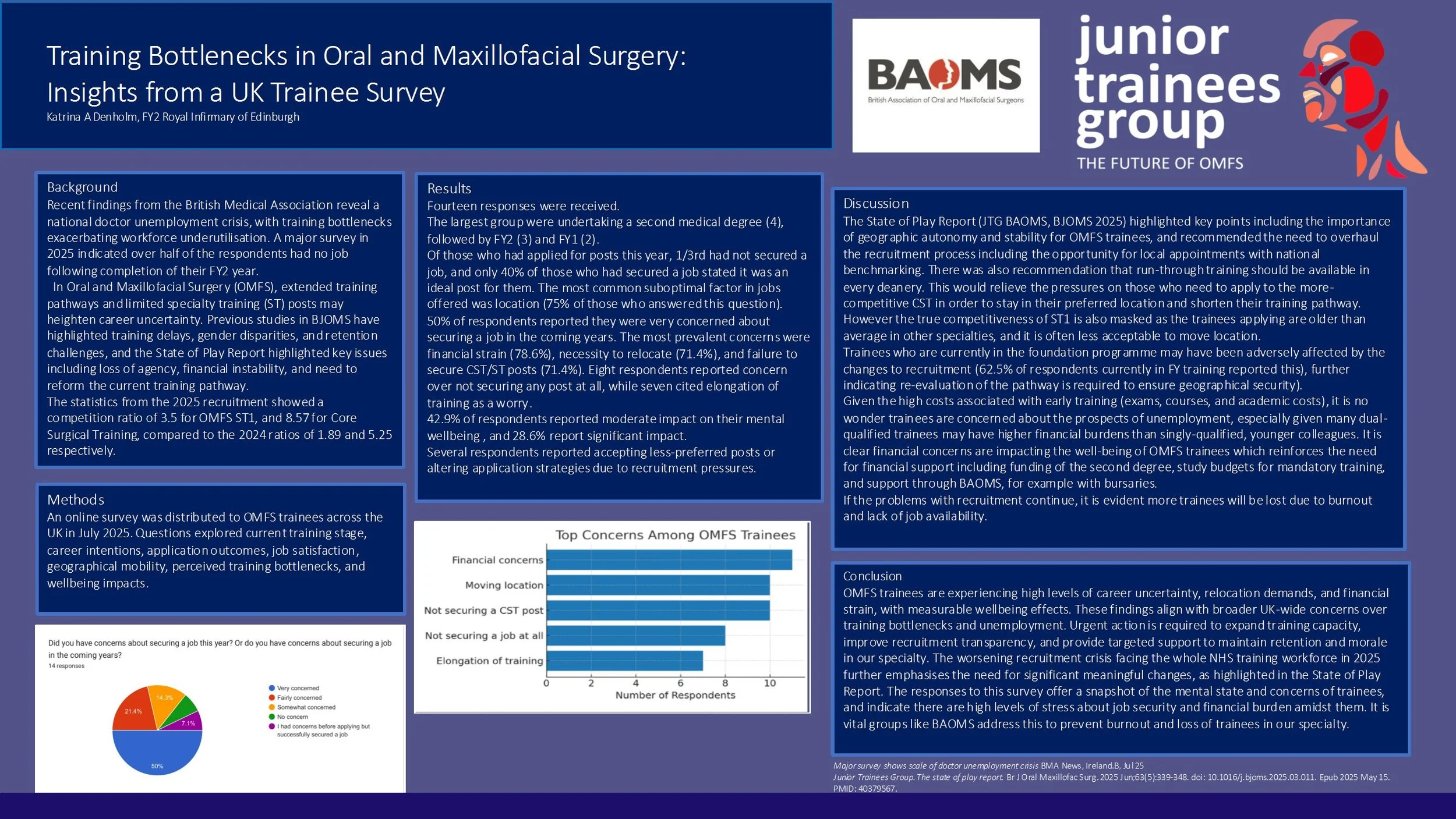
Training Bottlenecks in Oral and Maxillofacial Surgery: Insights from a UK Trainee Survey
Background
Recent findings from the British Medical Association reveal a national doctor unemployment crisis, with training bottlenecks exacerbating workforce underutilisation. In Oral and Maxillofacial Surgery (OMFS), extended training pathways and limited specialty training (ST) posts may heighten career uncertainty. Previous studies in BJOMS have highlighted training delays, gender disparities, and retention challenges, and the State of Play Report highlighted key issues including loss of agency, financial instability, and need to reform the current training pathway.
Methods
An online survey was distributed to OMFS trainees across the UK in July 2025. Questions explored current training stage, career intentions, application outcomes, job satisfaction, geographical mobility, perceived training bottlenecks, and wellbeing impacts.
Results
Fourteen responses were received. The largest group were undertaking a second medical degree, followed by FY2 and FY1. The most prevalent concerns were financial (78.6%), necessity to relocate (71.4%), and failure to secure CST posts (71.4%). Eight respondents feared not securing any post at all, while seven cited elongation of training as a worry. Wellbeing was moderately impacted in 42.9% and significantly impacted in 28.6%. Several respondents reported accepting less-preferred posts or altering application strategies due to recruitment pressures.
Conclusions
OMFS trainees are experiencing high levels of career uncertainty, relocation demands, and financial strain, with measurable wellbeing effects. These findings align with broader UK-wide concerns over training bottlenecks and underemployment. Urgent action is required to expand training capacity, improve recruitment transparency, and provide targeted support to maintain retention and morale in our speciality. The recruitment crisis facing the NHS workforce in 2025 further emphasises the need for significant meaningful changes highlighted by the State of Play Report.