JTG 2025 Poster Gallery
A Quality Improvement Project to Improve Patient Aftercare Following Botulinum Toxin Injections for Temporomandibular Dysfunction
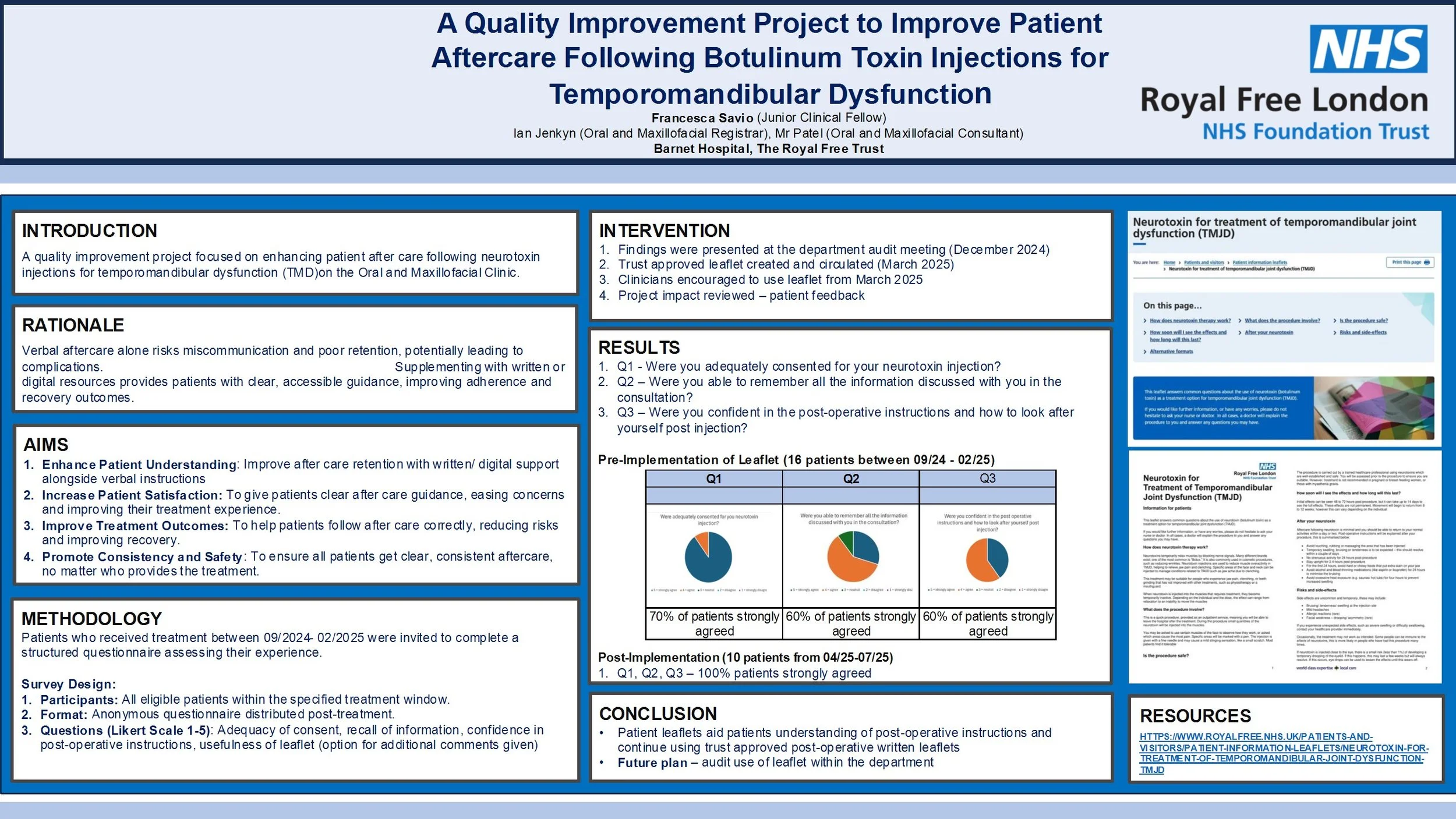
Introduction
Temporomandibular dysfunction (TMD) is increasingly managed with botulinum toxin injections. However, current practice at the Royal Free London NHS Foundation Trust involves providing only verbal aftercare instructions, which may be insufficient for optimal patient understanding and recovery. This quality improvement project aimed to enhance patient aftercare by introducing written resources to supplement verbal guidance.
Method
Two audit cycles were conducted. In Cycle 1 (Feb 2025), patients who received botulinum toxin injections for TMD between Sept 2024 and Feb 2025 were surveyed via telephone using a structured questionnaire. Questions assessed consent quality, recall of verbal instructions, confidence in post-operative care, and interest in written materials. Following Cycle 1, a trust-approved patient leaflet was introduced. Cycle 2 (June 2025) repeated the audit for patients treated after April 2025, evaluating the impact of the leaflet.
Results
Cycle 1 included 16 patients (14 female, 2 male; average age 45). Of the 10 respondents, 90% strongly agreed they were adequately consented, 60% agreed they remembered the verbal instructions, and 100% expressed interest in written aftercare materials. In Cycle 2, patients were surveyed post-leaflet implementation. All respondents (100%) found the written instructions useful and agreed they improved their confidence in post-treatment care.
Conclusion
The introduction of written aftercare materials significantly improved patient satisfaction and confidence in managing post- injections care for TMD. The audit supports continued use of written leaflets as standard practice and highlights the importance of multimodal communication in clinical care. Future audits will monitor long-term outcomes and adherence to aftercare protocols.
Re-audit of time to surgery for mandibular fractures following implementation of the Head and Neck Assessment Hub (HANAH)
Introduction
Recent studies have shown that delays in the treatment of mandibular fractures are not associated with adverse outcomes, and this has challenged the common practice of recommending treatment within 24 hours. However, the BAOMS Trauma Special Interest Group advocates early operation to facilitate prompt discharge. We aim to analyse the time from admission to operation of mandibular fractures and identify any reasons for delays.
Method
Retrospective data was collected from records of all admitted mandible fractures over a 3 month period between May and July in 2022, 2023 and 2025 from a major trauma hospital. Time from admission to operation was measured and compared to the standard that 100% of mandibular fractures will undergo open reduction and internal fixation (ORIF) within 48 hours of admission. Data collected also included: patient demographics, other injuries, theatre type, complications and discharge time.
Results
77% (10/13), 79% (15/19) and 76% (13/17) of mandible fractures underwent ORIF within 48 hours of admission over the same 3 month period in 2022, 2023 and 2025 respectively. The mean, median and range of time to undergo ORIF from admission for: 2022 was 36.5 hours, 27 hours, 11-100 hours respectively; 2023 was 40.4 hours, 19 hours, 0-282 hours respectively; 2025 was 26.7 hours, 19 hours, 5-63 hours respectively. There were 0, 4 and 6 post-operative complications over the 3 month period in 2022, 2023 and 2025 respectively.
Conclusion
The set standard was not met and the proportion of mandible fractures that underwent operation within 48 hours of admission over the years is consistently around 76-79%. Unlike previous years, 3 of the cases that underwent operation over 48 hours in 2025 had post-operative complications. We will continue to monitor to see if a dedicated trauma list would be indicated.