JTG 2025 Poster Gallery
Orthognathic Surgery Outcomes: A Regional Unit’s BAOMS Audit Findings
Introduction
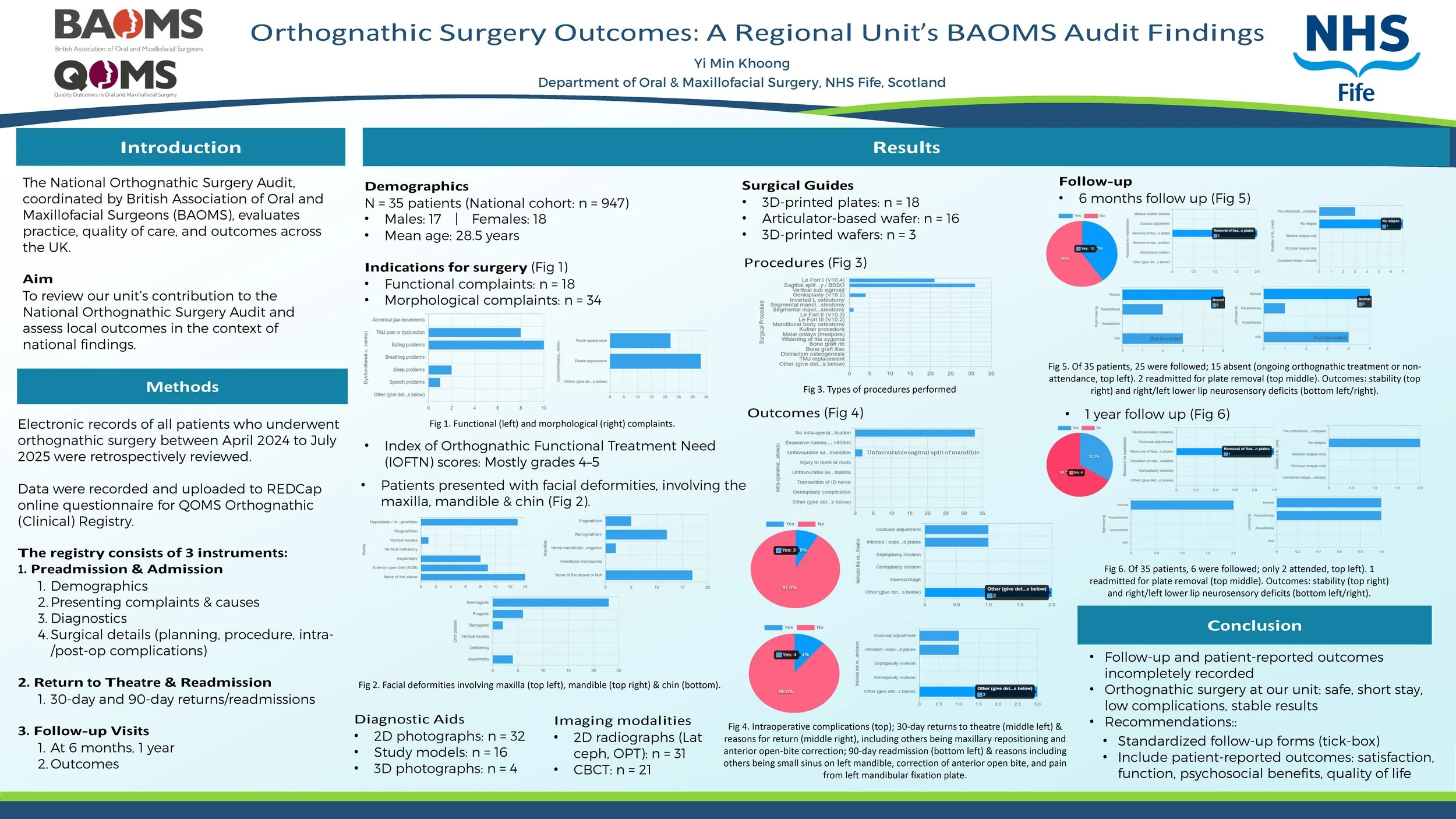
The National Orthognathic Surgery Audit conducted by British Association of Oral and Maxillofacial Surgeons (BAOMS) aims to assess practice, quality of care, and outcomes throughout the UK. This retrospective audit presents findings from a regional maxillofacial unit, which contributed 35 patients to the national cohort of 947 from April 2024 to July 2025.
Methods
A review was conducted of all patients who underwent orthognathic surgery at our unit during this period. Data was collected on demographics, presenting complaints, diagnoses, treatment plans, surgical procedures, and postoperative outcomes.
Result
The cohort included 17 males and 18 females, with a mean age of 28.53 years. Indications encompassed functional issues (e.g., masticatory difficulties, TMJ dysfunction), and morphological deformities (facial, dental appearance). IOFTN scores were predominantly 4–5, reflecting high need.
The majority underwent combined procedures, most commonly Le Fort I osteotomy and bilateral sagittal split osteotomy, with a smaller proportion receiving genioplasty. Planning methods included both traditional and digital approaches, ranging from standard articulator-based techniques and wafers to advanced 3D planning with 3D-printed wafers.
The median inpatient stay was 1 day (range 0–2), with 10 patients discharged within 24 hours. Intraoperative complications were uncommon, with 2 cases of unfavourable sagittal split of mandible. A minority (5 patients) returned to theatre within 90 days, primarily for fixation plate-related problems and occlusal adjustments.
At follow-up, outcomes were stable with minimal relapse rates and acceptable neurosensory deficit. One readmission occurred within 1 year for plate removal. Documentation of follow-up and patient-reported outcomes was inconsistent across cases.
Conclusion
Orthognathic surgery at our unit demonstrates safe practice, short inpatient stay, low complication rates, and stable results. Follow-up documentation could be improved using a standardized tick-box, and patient-reported outcomes (e.g., satisfaction, functional and psychosocial benefits, quality of life) should be incorporated to better capture treatment impact.