JTG 2025 Poster Gallery
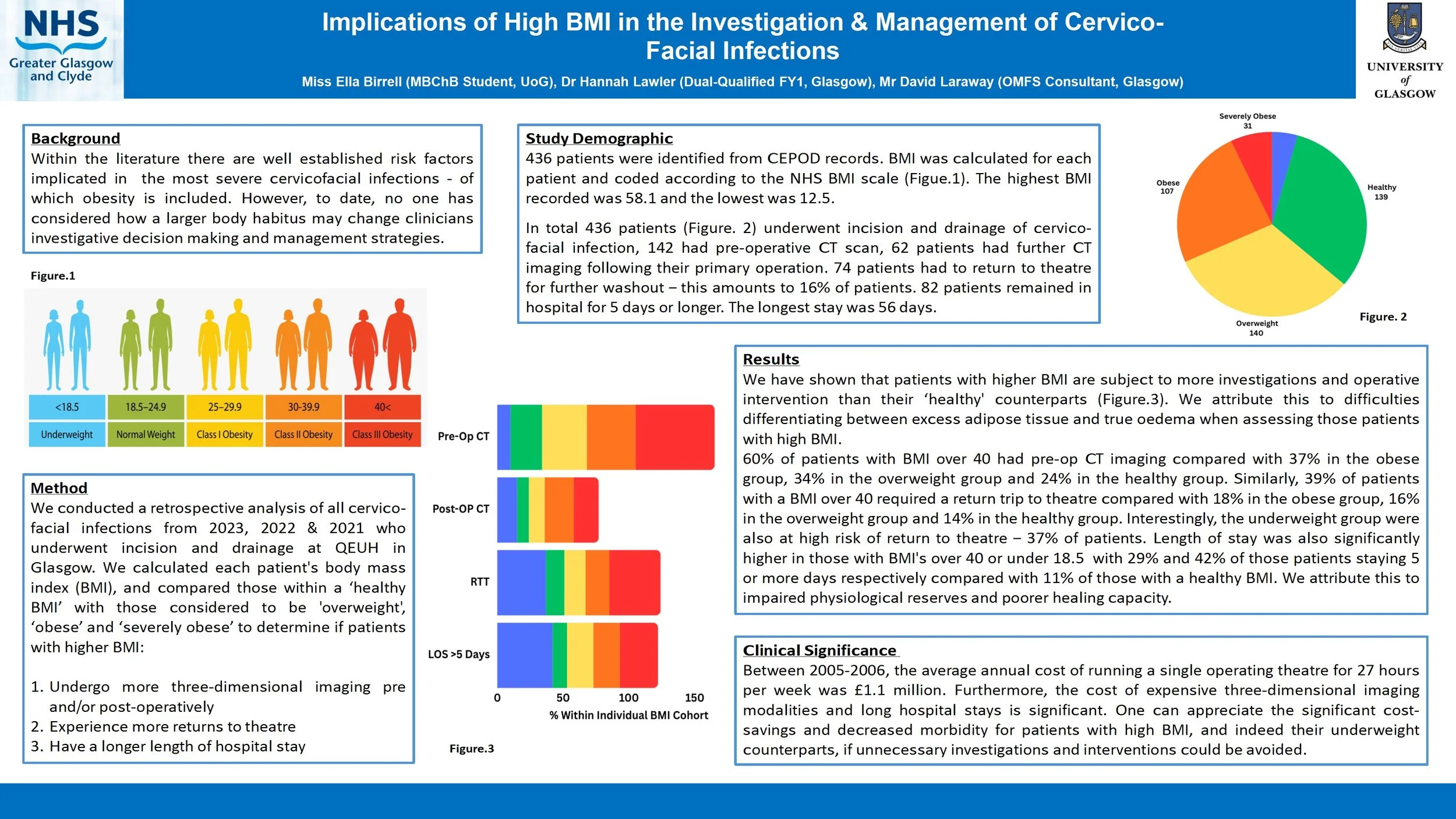
Implications of High BMI in the Investigation & Management of Cervico-Facial Infections
Introduction
Within the literature there are well established risk factors implicated in the most severe cervicofacial infections - of which obesity is included. However, to date, no one has considered how a larger body habitus may change clinicians investigative decision making and management strategies.
Method
We conducted a retrospective analysis of all cervico-facial infections over the last 6 years who underwent incision and drainage at QEUH in Glasgow. We calculated each patient's body mass index (BMI), and compared those within a ‘healthy BMI’ with those considered to be ‘obese’ and ‘morbidly obese’ to determine if patients with higher BMI:
Undergo more three-dimensional imaging pre/post-operatively
Experience more returns to theatre
Have a longer length of hospital stay
Are more likely to require a tracheostomy or intensive care stay
Results
We have shown that patients with higher BMI are subject to more investigations and operative intervention than their ‘healthy BMI’ counterparts. We attribute this to difficulties differentiating between excess adipose tissue and true oedema when assessing those patients with high BMI.
Conclusion
Between 2005-2006, the average annual cost of running a single operating theatre for 27 hours per week was £1.1 million. Furthermore, the cost of expensive three-dimensional imaging modalities and long hospital stays is significant. One can appreciate the significant cost-savings and decreased morbidity for patients with high BMI if unnecessary investigations and interventions could be avoided.
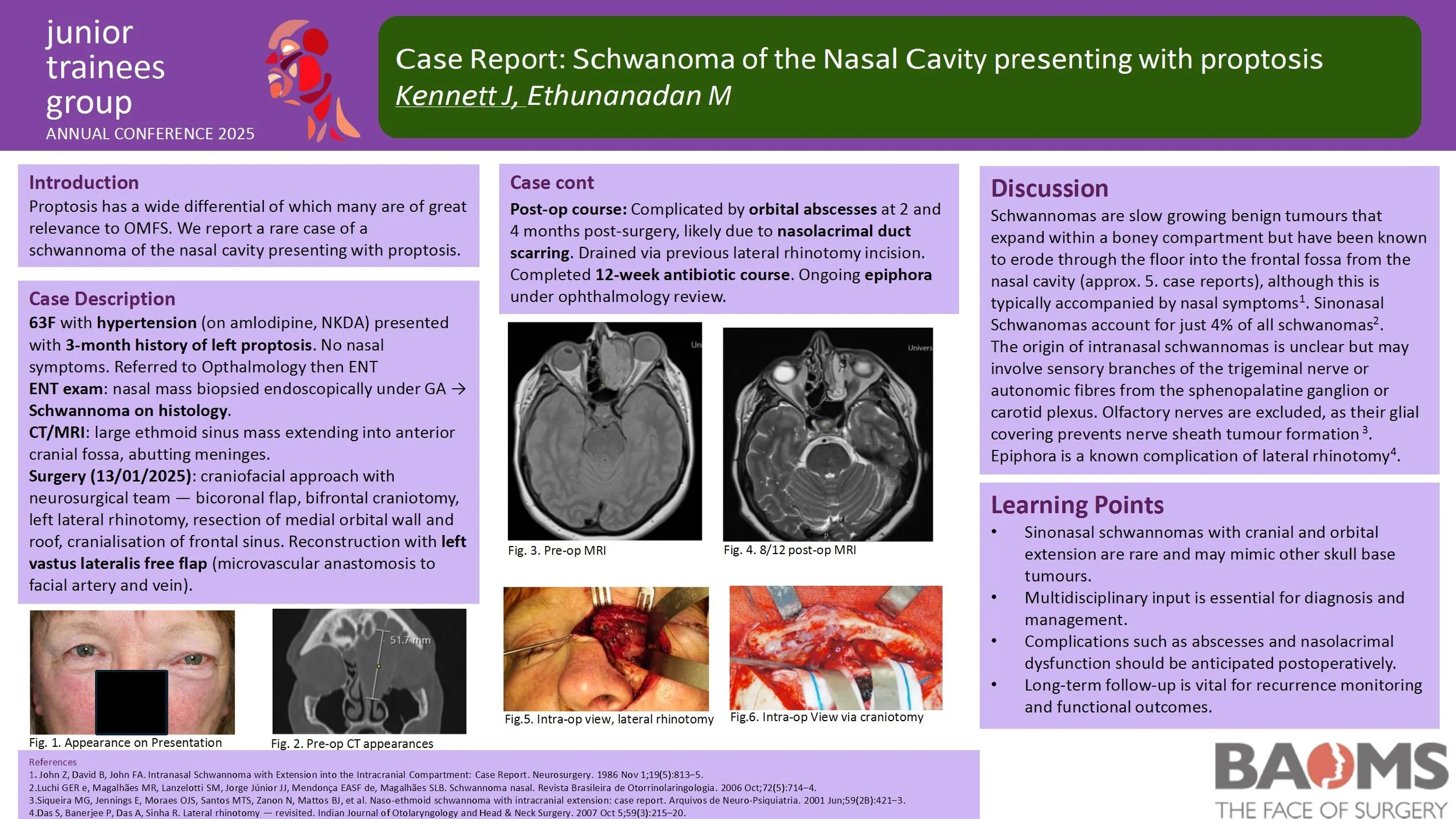
Case Report: Schwanoma of the Nasal Cavity presenting with proptosis
Introduction
Within the literature there are well established risk factors implicated in the most severe cervicofacial infections - of which obesity is included. However, to date, no one has considered how a larger body habitus may change clinicians investigative decision making and management strategies.
Method
We conducted a retrospective analysis of all cervico-facial infections over the last 6 years who underwent incision and drainage at QEUH in Glasgow. We calculated each patient's body mass index (BMI), and compared those within a ‘healthy BMI’ with those considered to be ‘obese’ and ‘morbidly obese’ to determine if patients with higher BMI:
Undergo more three-dimensional imaging pre/post-operatively
Experience more returns to theatre
Have a longer length of hospital stay
Are more likely to require a tracheostomy or intensive care stay
Results
We have shown that patients with higher BMI are subject to more investigations and operative intervention than their ‘healthy BMI’ counterparts. We attribute this to difficulties differentiating between excess adipose tissue and true oedema when assessing those patients with high BMI.
Conclusion
Between 2005-2006, the average annual cost of running a single operating theatre for 27 hours per week was £1.1 million. Furthermore, the cost of expensive three-dimensional imaging modalities and long hospital stays is significant. One can appreciate the significant cost-savings and decreased morbidity for patients with high BMI if unnecessary investigations and interventions could be avoided.
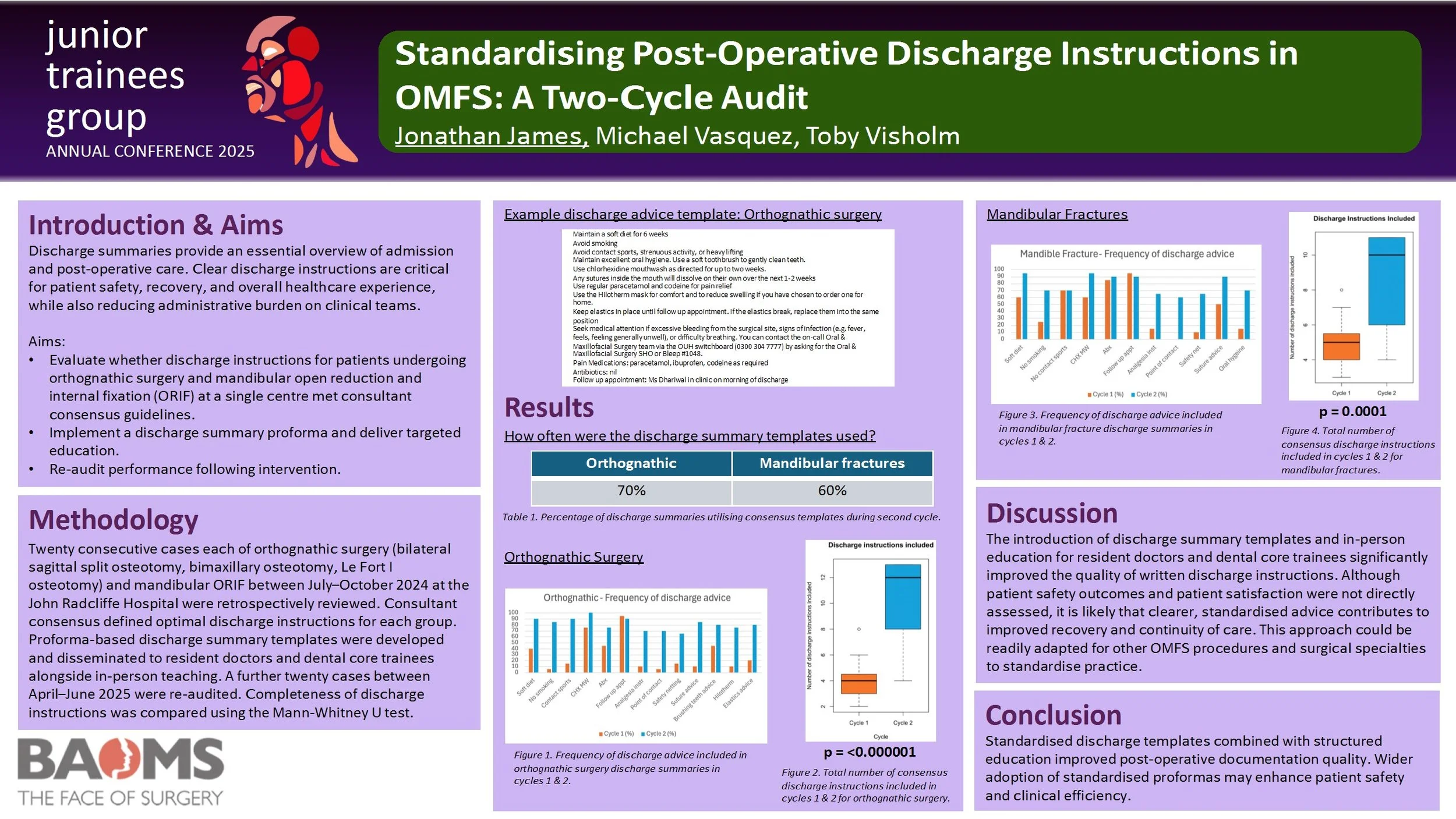
Standardising Post-Operative Discharge Instructions in OMFS: A Two-Cycle Audit
Introduction
Discharge summaries provide an essential overview of admission and post-operative care. Clear discharge instructions are critical for patient safety, recovery, and overall healthcare experience, while also reducing administrative burden on clinical teams.
Aims
1. To evaluate whether discharge instructions for patients undergoing orthognathic surgery and mandibular open reduction and internal fixation (ORIF) at a single centre met consultant consensus guidelines.
2. To implement a discharge summary proforma with targeted education.
3. To re-audit performance following intervention.
Methods
Twenty consecutive cases of orthognathic surgery (bilateral sagittal split osteotomy, bimaxillary osteotomy, Le Fort I osteotomy) and mandibular ORIF between July–October 2024 at the John Radcliffe Hospital were retrospectively reviewed. Consultant consensus defined optimal discharge instructions for each group. Proforma-based discharge summary templates were developed and disseminated to resident doctors and dental core trainees alongside in-person teaching. A further twenty cases between April–June 2025 were re-audited. Completeness of discharge instructions was compared using the Mann-Whitney U test.
Results
In the second cycle, templates were used in 70% of orthognathic cases and 60% of mandibular fracture cases. There was a significant improvement in the total number of relevant discharge instructions included for both orthognathic surgery (p = 0.0000006) and mandibular fractures (p = 0.0001).
Discussion
The introduction of discharge summary templates and in-person education for resident doctors and dental core trainees significantly improved the quality of written discharge instructions. Although patient safety outcomes and patient satisfaction were not directly assessed, it is likely that clearer, standardised advice contributes to improved recovery and continuity of care. This approach could be readily adapted for other OMFS procedures and surgical specialties to standardise practice.
Conclusion
Standardised discharge templates combined with structured education improved post-operative documentation quality. Wider adoption of standardised proformas may enhance patient safety and clinical efficiency.
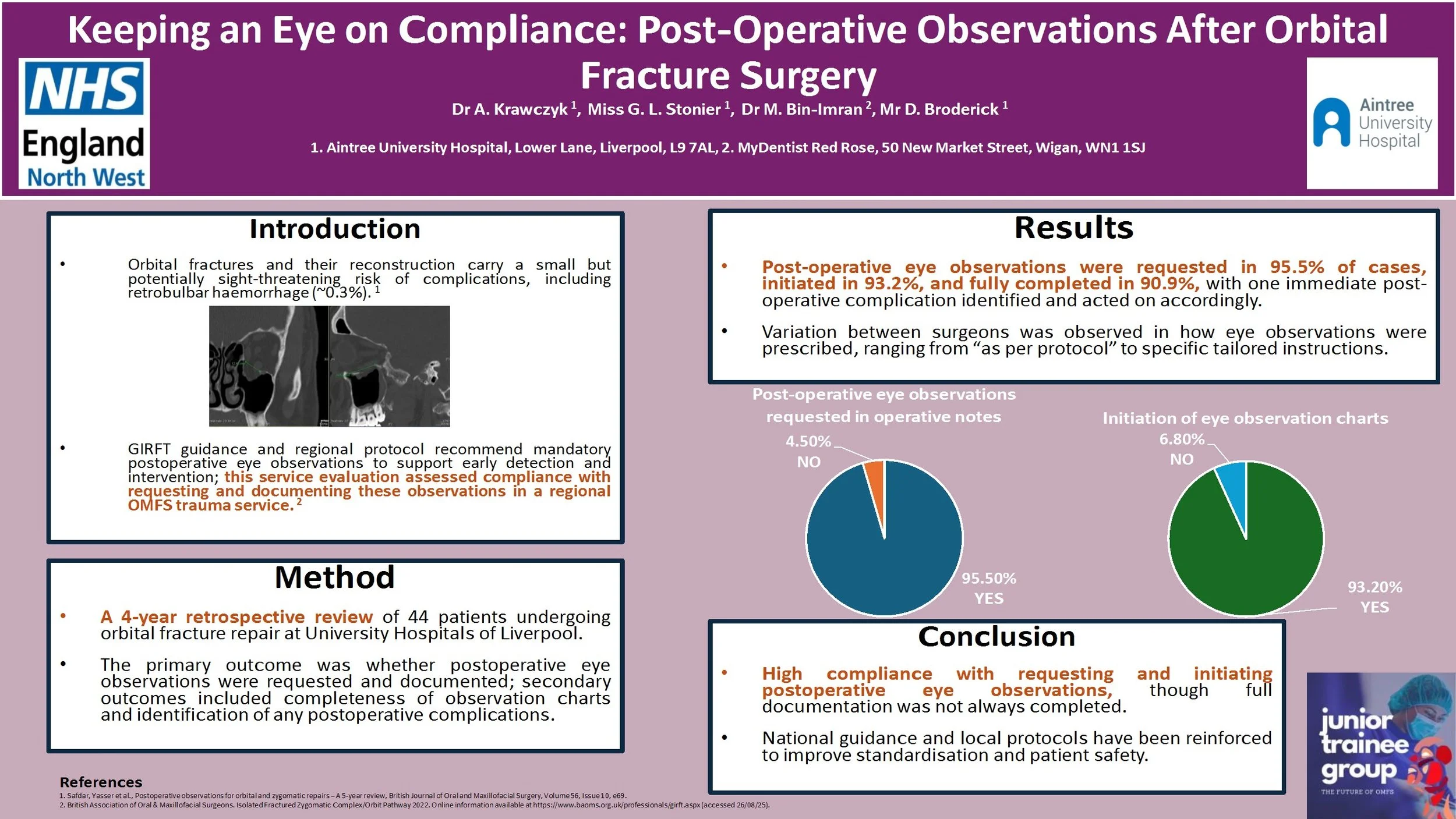
Keeping an Eye on Compliance: Post-Operative Observations After Orbital Fracture Surgery
Introduction:
Orbital fractures and the following reconstructive surgery carries a risk of sight-threatening complications, including retrobulbar haemorrhage (~0.3%).1 The Getting It Right First time (GIRFT) guidance2 and our regional protocol recommends mandatory postoperative eye observations to allow for early recognition and therefore intervention in case of developing sight‐threatening complications. This service evaluation assessed compliance of a regional Oral and Maxillofacial trauma service with requesting and documenting eye observations following orbital fracture surgery.
Method:
A retrospective review of 44 consecutive patients undergoing orbital fracture repair between 2020 and 2024 was conducted at University Hospitals of Liverpool Group. Information was recorded using an electronic data collection tool. The primary outcome was whether post-operative eye observations were requested and documented, with secondary outcomes including whether eye observation charts were completed fully and any complications identified.
Results:
Of the 44 patients, post-operative eye observations were requested in operative notes in 95.5% of cases. Majority (93.2%) of patients had eye observation charts initiated, with complete documentation recorded in 90.9%. One case displayed an immediate post-operative complication. Variation in practice between surgeons was noted, with some prescribing eye observations ‘as per protocol’ and others outlining specific recommendation.
Conclusion:
Compliance with requesting and initiating documentation of post-operative eye observations was high but full completion was inconsistent. National guidance and local protocol have been reinforced to optimise patient safety.
References:
1. Safdar, Yasser et al., Postoperative observations for orbital and zygomatic repairs – A 5-year review, British Journal of Oral and Maxillofacial Surgery, Volume 56, Issue 10, e69.
2. British Association of Oral & Maxillofacial Surgeons. Isolated Fractured Zygomatic Complex/Orbit Pathway, 2022. Online information available at https://www.baoms.org.uk/professionals/girft.aspx (accessed 26/08/25).
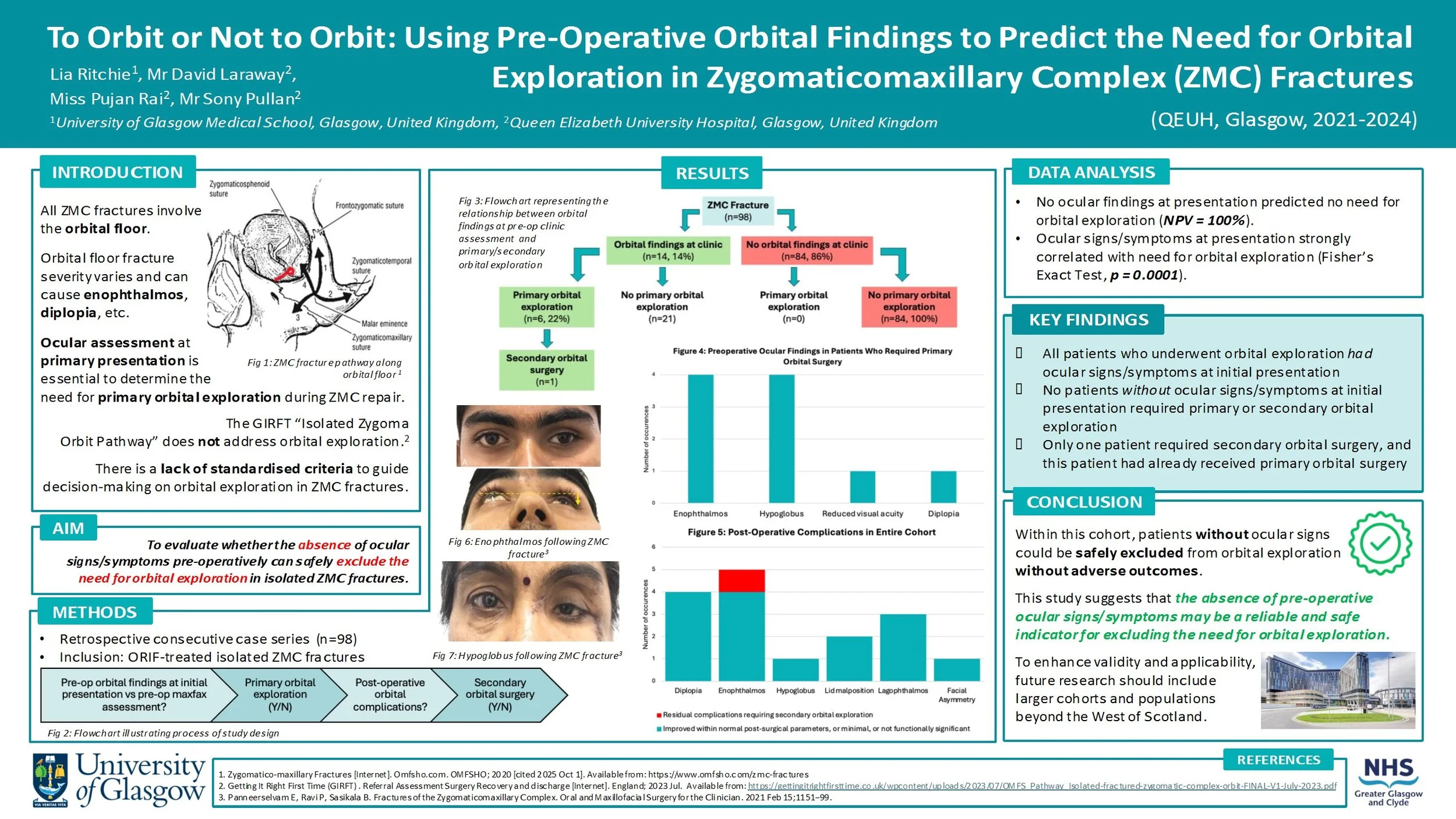
To Orbit or Not to Orbit: Using Pre-Operative Orbital Findings to Predict the Need for Orbital Exploration in Zygomaticomaxillary Complex (ZMC) Fractures
Introduction:
All ZMC fractures involve orbital fractures, with orbital floor fracture severity varying depending on the mechanism and energy of injury. Disruption of the orbital floor changes the orbital volume, increasing the risk of ocular signs/symptoms (e.g. enophthalmos, diplopia). This must be assessed at primary presentation to decide if primary orbital surgery should be performed alongside ZMC repair.
There is currently no standardised set of criteria to guide the decision-making process for orbital exploration in ZMC fractures. This study will evaluate whether the absence of ocular signs/symptoms pre-operatively can safely exclude the need for orbital exploration.
Method:
Data was retrospectively collected from a consecutive series of 98 patients who had ZMC fractures requiring ORIF intervention at the QEUH between 2021-2024. The presence/absence of ocular signs/symptoms at initial assessment was recorded. The cohort was then assessed to determine which patients underwent primary orbital exploration. Post-operative outcomes were reviewed, including whether any patients subsequently required secondary orbital surgery.
Results:
27 patients (28%) presented with ocular signs/symptoms, 6 of them underwent primary orbital surgery. Among the 71 patients (72%) who had no ocular findings at initial presentation, none required orbital surgery. Only 1 patient in the cohort required secondary orbital surgery, and this patient had also undergone primary orbital surgery.
Conclusion:
The absence of pre-operative ocular signs/symptoms may be a reliable indicator for excluding the need for orbital exploration. No patients who did not receive primary orbital exploration needed secondary orbital exploration, proving there were no late ocular complications from this approach.
Re-audit of time to surgery for mandibular fractures following implementation of the Head and Neck Assessment Hub (HANAH)
Introduction
Recent studies have shown that delays in the treatment of mandibular fractures are not associated with adverse outcomes, and this has challenged the common practice of recommending treatment within 24 hours. However, the BAOMS Trauma Special Interest Group advocates early operation to facilitate prompt discharge. We aim to analyse the time from admission to operation of mandibular fractures and identify any reasons for delays.
Method
Retrospective data was collected from records of all admitted mandible fractures over a 3 month period between May and July in 2022, 2023 and 2025 from a major trauma hospital. Time from admission to operation was measured and compared to the standard that 100% of mandibular fractures will undergo open reduction and internal fixation (ORIF) within 48 hours of admission. Data collected also included: patient demographics, other injuries, theatre type, complications and discharge time.
Results
77% (10/13), 79% (15/19) and 76% (13/17) of mandible fractures underwent ORIF within 48 hours of admission over the same 3 month period in 2022, 2023 and 2025 respectively. The mean, median and range of time to undergo ORIF from admission for: 2022 was 36.5 hours, 27 hours, 11-100 hours respectively; 2023 was 40.4 hours, 19 hours, 0-282 hours respectively; 2025 was 26.7 hours, 19 hours, 5-63 hours respectively. There were 0, 4 and 6 post-operative complications over the 3 month period in 2022, 2023 and 2025 respectively.
Conclusion
The set standard was not met and the proportion of mandible fractures that underwent operation within 48 hours of admission over the years is consistently around 76-79%. Unlike previous years, 3 of the cases that underwent operation over 48 hours in 2025 had post-operative complications. We will continue to monitor to see if a dedicated trauma list would be indicated.
Orbital Roof Reconstruction Utilizing Inverted Orbital Floor Plates - A Case-Based Technical Note
Background: Orbital roof fractures are rare [1] but significant injuries resulting from high-energy trauma, often alongside complex maxillofacial injuries [2,3]. Surgical repair is indicated for displaced fractures with neurological or ophthalmic compromise [4]. Traditional reconstruction with titanium mesh presents challenges such as insufficient rigidity, sharp edges, implant extrusion risk, and difficulty of removal if infected. As such, we propose using pre-shaped orbital floor plates, inverted for orbital roof reconstruction, offering improved structural support and a more ergonomic surgical experience.
Methods: Retrospective case series (n=4) of patients undergoing surgical repair for orbital roof fractures. A bicoronal and pericranial flap was raised, followed by hemifrontal craniotomy. Orbital roof defects were visualised, dural tears repaired, and reconstruction performed using inverted orbital floor plates secured with screws. A pericranial flap covered the repair, and the bone flap was re-fixed with low-profile plating. Postoperative outcomes were assessed.
Results: All cases achieved correct orbital roof alignment and restoration of orbital volume. No implant-related infections were found. Progressive recovery or complete resolution of ocular symptoms was observed, even in severe trauma patients.
Discussion: This case series demonstrates the feasibility, safety, and structural adequacy of using inverted orbital floor plates for orbital roof reconstruction. This alternative offers greater rigidity, easier handling, anatomical contour matching and immediate availability in trauma settings, with good outcomes even in severe trauma. Study limitations include small sample size due to the rarity of the fracture, heterogeneous trauma profiles, and limited long-term follow-up. Therefore, further studies are needed to confirm long-term outcomes.
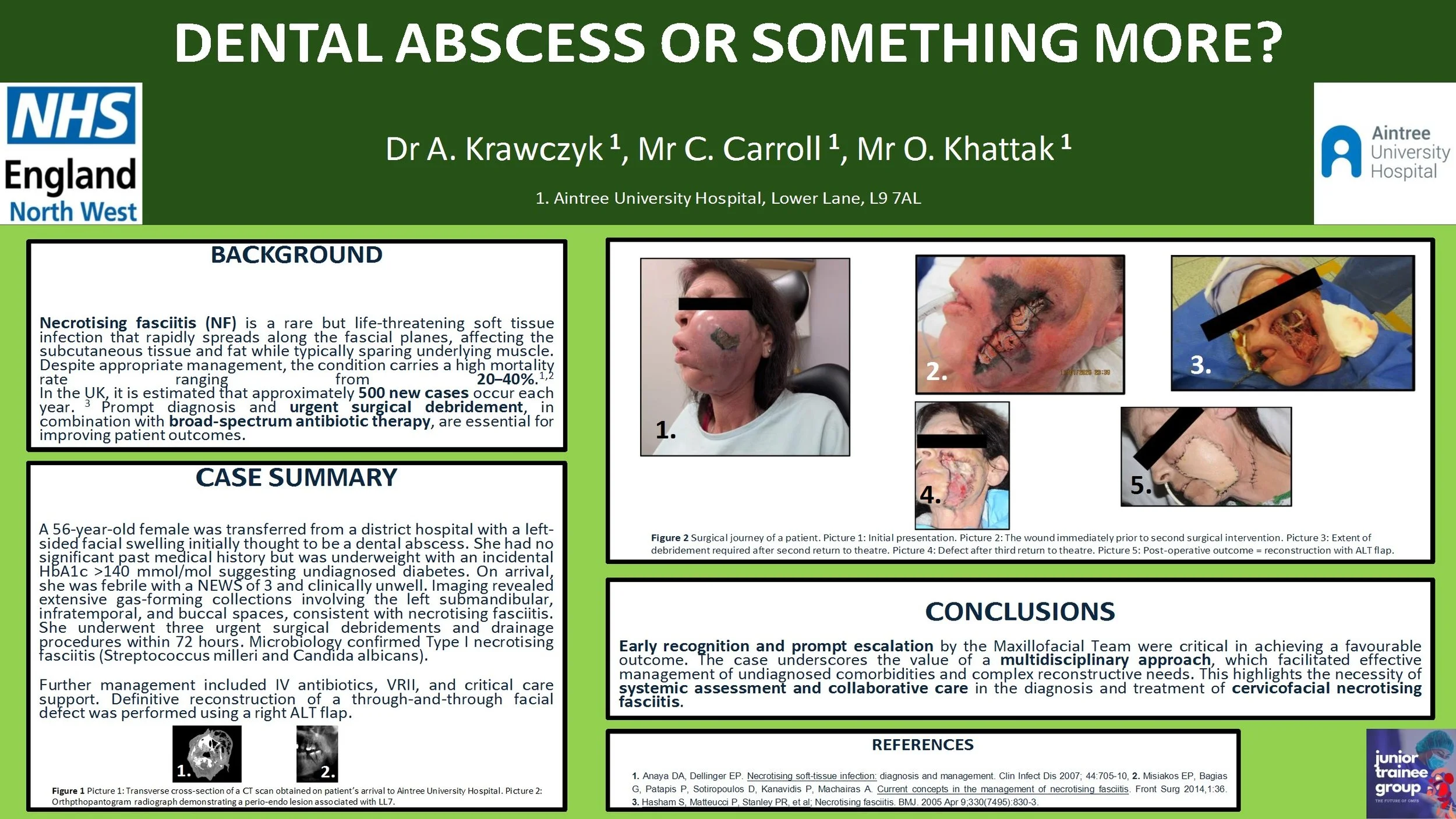
Dental abscess or something more?
Introduction:
Necrotising fasciitis is a rare, rapidly progressive soft tissue infection with high morbidity and mortality, often polymicrobial (Type I) and associated with immunocompromised states. Prompt recognition and aggressive surgical management are essential.
Case report:
A 56-year-old female was transferred from a district hospital with a left-sided facial swelling initially thought to be a dental abscess. She had no significant past medical history but was underweight with an incidental HbA1c >140 mmol/mol suggesting undiagnosed diabetes. On arrival, she was febrile with a NEWS of 3 and clinical unwell. Imaging revealed extensive gas-forming collections involving the left submandibular, infratemporal, and buccal spaces, consistent with necrotising fasciitis. She underwent three urgent surgical debridements and drainage procedures within 72 hours. Microbiology confirmed Type I necrotising fasciitis (Streptococcus milleri and Candida albicans). Further management included intravenous antibiotics, variable rate insulin infusion, and critical care support. Definitive reconstruction of a through-and-through facial defect was performed using a right antero-lateral thigh free flap.
Discussion:
Early recognition and escalation by the on-call Maxillofacial team were key to successful outcomes. A multidisciplinary approach enabled management of complex comorbidities and reconstruction. This case highlights the importance of systemic evaluation and team-based care in managing cervicofacial necrotising fasciitis.
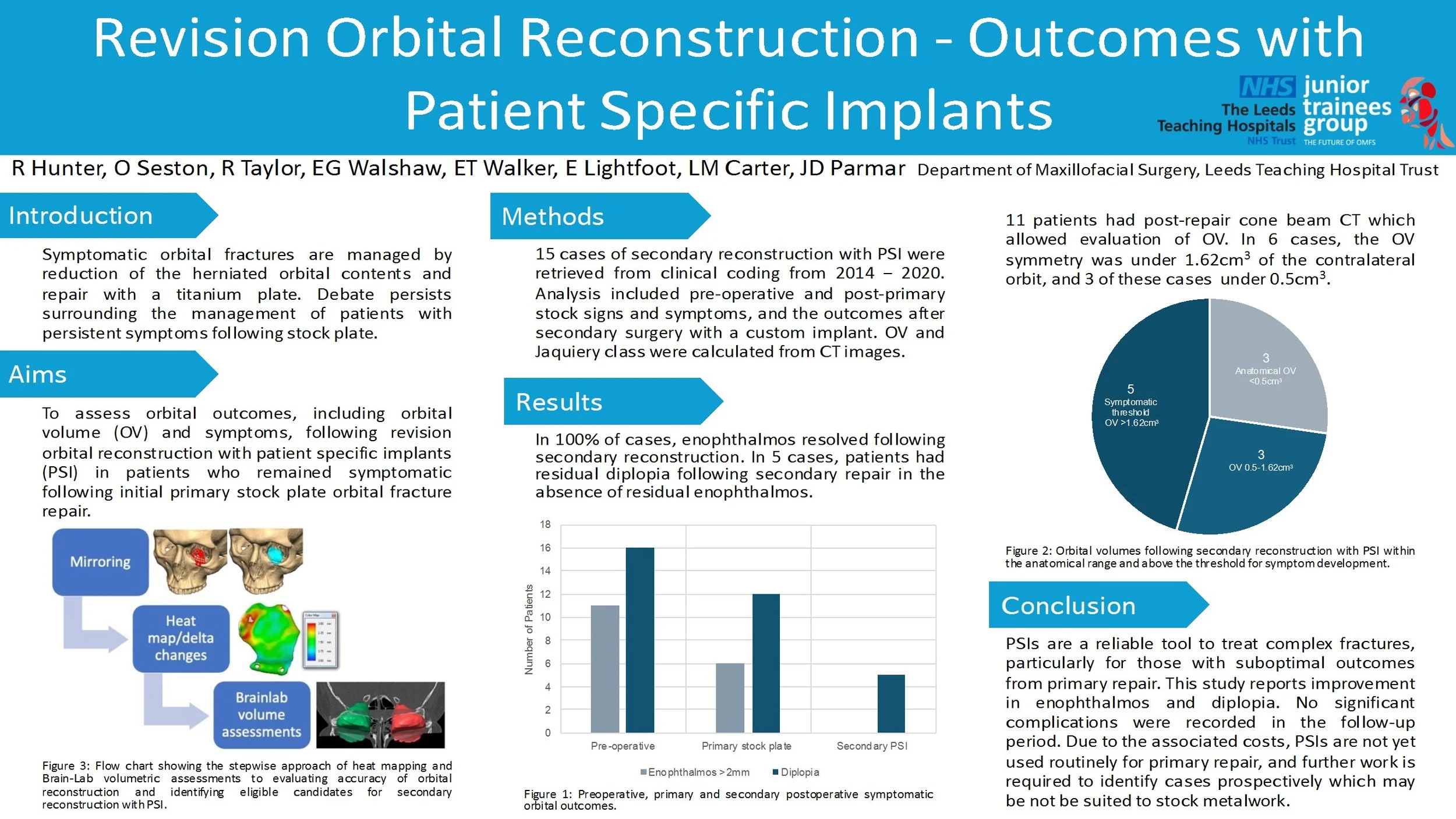
Revision Orbital Reconstruction - Outcomes with Patient Specific Implants
Introduction/Aims
The mainstay of treatment of symptomatic orbital fractures remains the reduction of herniated orbital contents and repair with a titanium plate. The management of patients who have had a stock plate with persistent symptoms is subject to debate. In this study, 15 patients underwent a novel analysis of orbital volumes (OV) and symptom assessment, prior to revision surgery with a patient specific implant (PSI).
Materials and Methods
Relevant cases were retrieved from clinical coding, operated between 2014 - 2020. After excluding 4 cases, 15 cases of revision reconstruction with PSI were analysed in detail, including pre-operative and post-primary-op signs and symptoms, and the outcomes after revision surgery with a custom implant. OV and Jaquiery class were calculated from CT images.
Results/Statistics
In 100% of cases, exophthalmos and hypoglobus resolved following revision reconstruction. In 5 cases, patients had residual diplopia following revision repair in the absence of residual exophthalmos or hypoglobus. 11 patients had post-repair cone beam CT which allowed evaluation of OV. In 6 cases, the OV symmetry was under 1.62cm3 of the contralateral orbit, and 3 of these cases under 0.5cm3.
Conclusions/Clinical Relevance
PSIs are a reliable tool to treat complex fractures, particularly for those with suboptimal outcomes from primary repair. This study reports good outcomes in terms of enophthalmos and hypoglobus with no significant complications in the followup period. Due to the associated costs, PSIs are not yet used routinely for primary repair, and further work is required to identify cases prospectively which may be not be suited to stock metalwork.
Reconstruction of Multifocal Comminuted Facial Fractures Caused by a Horse Kick
Introduction
Naso-orbital-ethmoidal (NOE) fractures are uncommon, complex facial fractures that
are often sustained following higher energy injury mechanisms. Common
mechanisms include road traffic accidents, sports injuries and horse kicks.
Anatomically, the NOE complex lies close to key facial structures including the orbits
and the anterior cranial fossa so damage to this complex can result in damage to
nearby structures. This can result in serious complications such as changes to vision
and intercranial infections.
Case Report
This case presents a 19-year-old patient who presented to the emergency
department following a horse kick to the face. Initial examinations revealed proptosis
and increased intercanthal distance. Imaging showed us that there were multifocal
comminuted fractures that involved the NOE complex, anterior cranial fossa, the
orbits, a retro-orbital haematoma, a small subdural haemorrhage and a small,
depressed skull fracture. The NOE fracture was determined to be a type 2 fracture
according to the Markowitz and Manson classification. Despite the severity of the
injuries, the patient remained GCS 15 throughout their care. For repair, an open
reduction and internal fixation using a coronal flap with cranialisation of the frontal
sinus was carried out.
Discussion
This case discusses the importance of early recognition and multidisciplinary
management of NOE fractures. Appropriate surgical intervention based on the
Markowitz and Manson classification is important in reducing complications such as
meningitis, facial deformities and ocular changes. Management of NOE fractures is
also important in order to achieve a good aesthetic outcome for the patient.
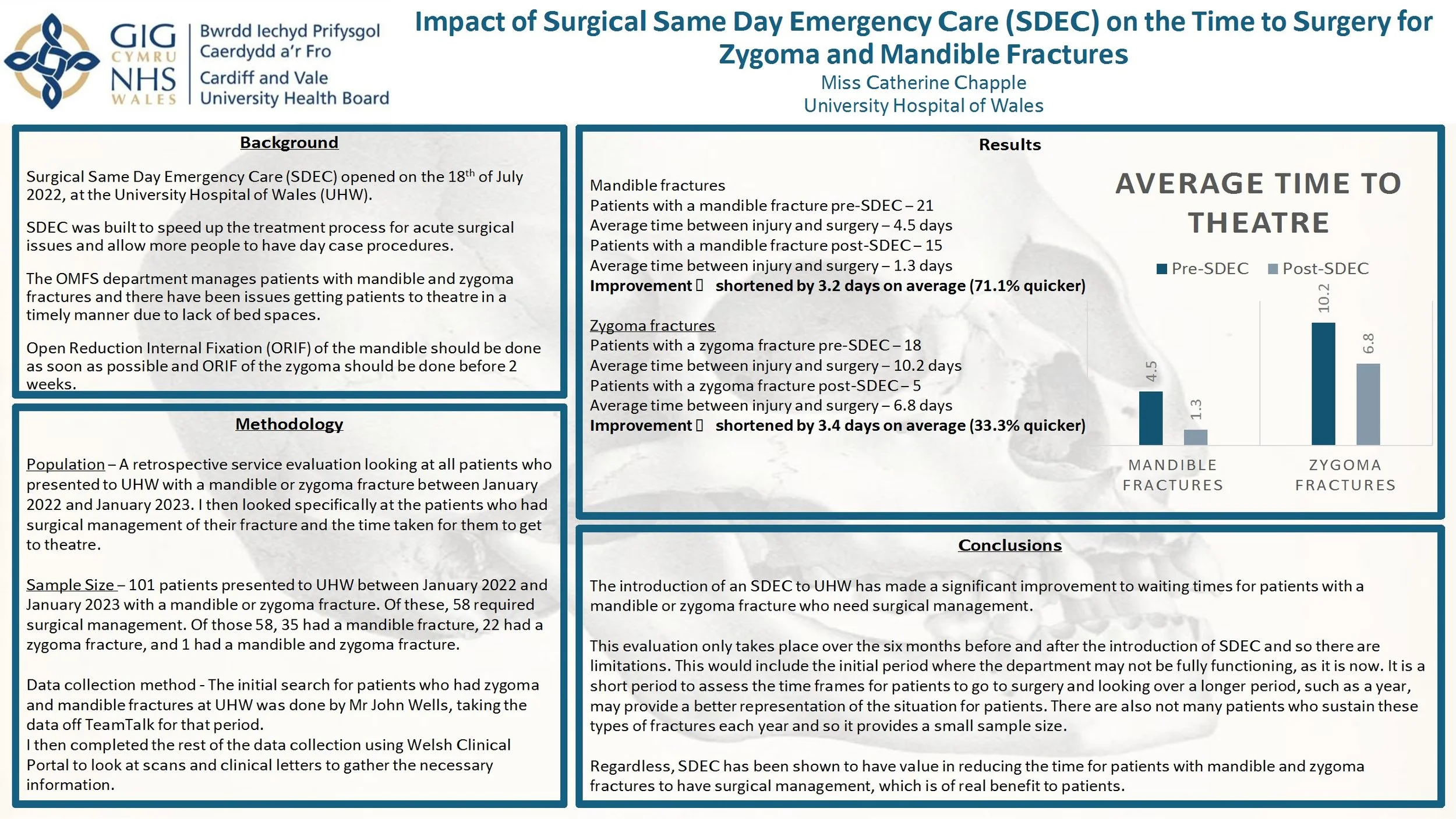
Impact of Surgical Same Day Emergency Care (SDEC) on the Time to Surgery for Zygoma and Mandible Fractures
Introduction: Surgical Same Day Emergency Care (SDEC) opened on July 18th 2022 at the University Hospital of Wales (UHW). It aimed to accelerate the treatment process for acute surgical procedures and allow more day case procedures. The OMFS department manages patients with mandible and zygoma fractures and there were delays to surgical management due to lack of bed spaces. Open reduction internal fixation (ORIF) of the mandible should be done as soon as possible and ORIF of the zygoma should be done before 2 weeks. This service evaluation investigates whether the opening of SDEC had an impact on the waiting times for patients with mandible and zygoma fractures to have surgery.
Method: This is a retrospective service evaluation looking at all patients who presented to UHW with a mandible or zygoma fracture between January 2022 and 2023. I looked specifically at patients who had surgical management. The initial search for patients was done by taking data from TeamTalk and the rest of the data collection was from Welsh Clinical Portal.
Results: 101 patients presented to UHW between January 2022 and 2023 with a mandible or zygoma fracture. Of these, 58 required surgical management. Patients with a mandible fracture had their surgery 3.2 days earlier on average and patients with a zygoma fracture had their surgery 3.4 days earlier on average, after the implementation of SDEC.
Conclusion: The introduction of SDEC to UHW has made a significant improvement to waiting times for patients with mandible or zygoma fractures who need surgical management. However, this evaluation only looks at the management of patients 6 months before and after the implementation of SDEC and it is important to investigate over a longer period. Regardless, SDEC has been shown to have value in reducing the time taken to achieve surgical management.