JTG 2025 Poster Gallery
Jaw Dropping Brothers: Sibling Success with Distraction Osteogenesis in Pierre Robin Sequence
Reducing Delays to PEG Insertion in Postoperative Head and Neck Cancer Patients: A Quality Improvement Project
Introduction:
Patients undergoing major head and neck cancer surgery can experience postoperative dysphagia requiring percutaneous endoscopic gastrostomy (PEG) for nutrition. For those not pre-emptively fitted with PEGs, delays in post-operative PEG insertion can prolong hospitalisation, recovery, and initiation of adjuvant treatment. This quality improvement project aimed to quantify these delays, assess their impact, and implement interventions to streamline care.
Methods:
A retrospective review of all postoperative head and neck cancer patients admitted to a specialist ward, in a single centre, between January 2024, and June 2025, requiring inpatient PEG insertion was done. Data included demographics, surgical details, PEG indication, time from PEG request to insertion, and length of hospital stay. Financial impact was calculated using standard NHS bed day costs.
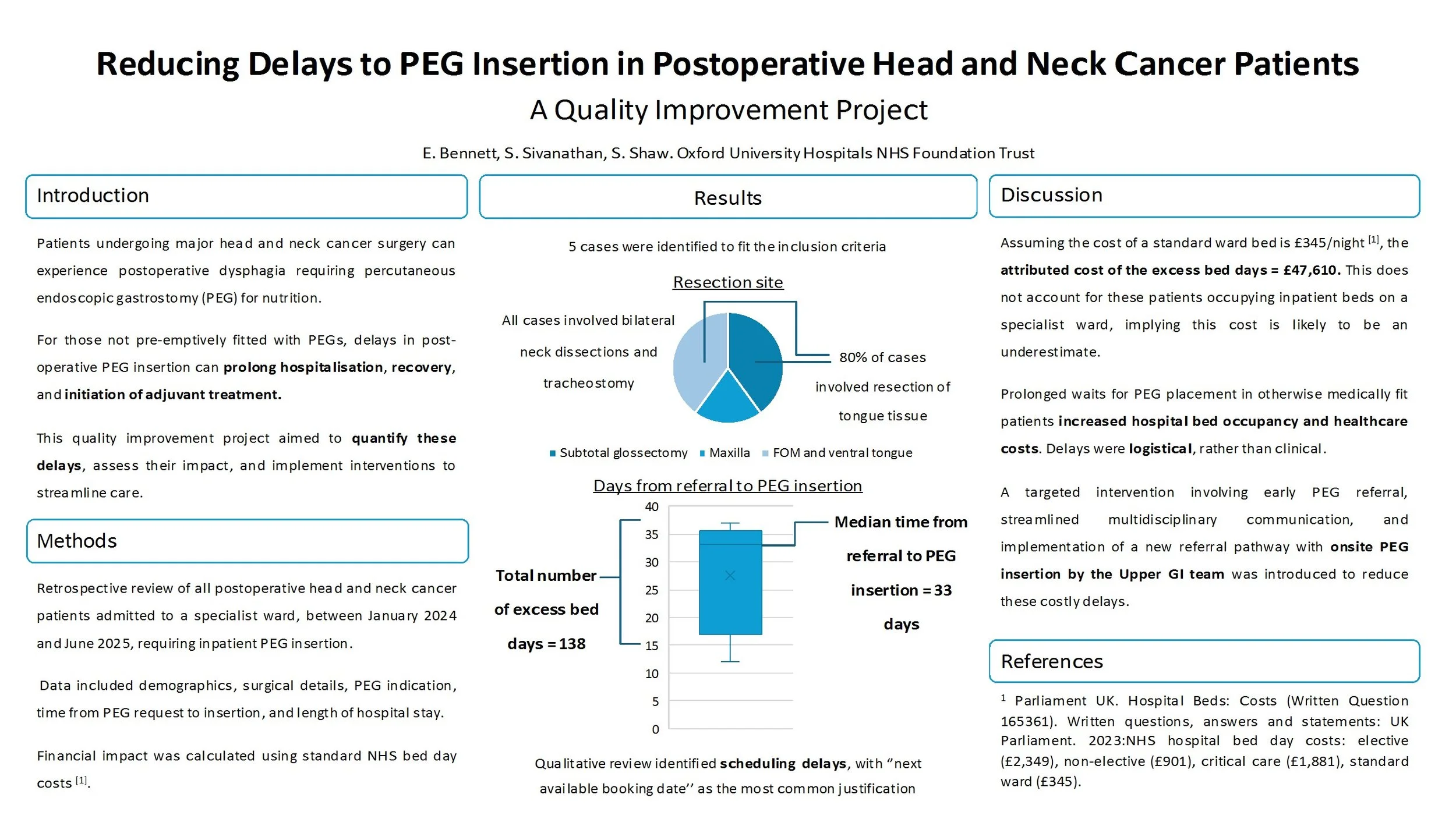
Results:
Five patients met inclusion criteria. All had extensive surgical procedures including bilateral neck dissections and tracheostomy. Median time from PEG request to insertion was 33 days (range: 12–37 days). Qualitative review revealed scheduling delays, with “next available booking date” as the most common justification. These delays accounted for 138 excess bed days, equating to an estimated cost of £47,610.
Discussion:
Prolonged waits for PEG placement in otherwise medically fit patients increased hospital bed occupancy and healthcare costs. Delays were logistical, rather than clinical. A targeted intervention involving early PEG referral, streamlined multidisciplinary communication, and onsite PEG insertion by the Upper GI team was introduced.
Conclusion:
Delayed PEG insertion in postoperative head and neck cancer patients leads to avoidable hospitalisation, financial burden, and may delay adjuvant treatment. Reasons for delay were specific to logistical factors within the unit. Results were presented and led to the implementation of an onsite referral pathway and improved interdepartmental coordination in order to offer a sustainable solution.
Reducing Delays to PEG Insertion in Postoperative Head and Neck Cancer Patients - A Quality Improvement Project
Reducing Delays to PEG Insertion in Postoperative Head and Neck Cancer Patients: A Quality Improvement Project
Introduction:
Patients undergoing major head and neck cancer surgery can experience postoperative dysphagia requiring percutaneous endoscopic gastrostomy (PEG) for nutrition. For those not pre-emptively fitted with PEGs, delays in post-operative PEG insertion can prolong hospitalisation, recovery, and initiation of adjuvant treatment. This quality improvement project aimed to quantify these delays, assess their impact, and implement interventions to streamline care.
Methods:
A retrospective review of all postoperative head and neck cancer patients admitted to a specialist ward, in a single centre, between January 2024, and June 2025, requiring inpatient PEG insertion was done. Data included demographics, surgical details, PEG indication, time from PEG request to insertion, and length of hospital stay. Financial impact was calculated using standard NHS bed day costs.
Results:
Five patients met inclusion criteria. All had extensive surgical procedures including bilateral neck dissections and tracheostomy. Median time from PEG request to insertion was 33 days (range: 12–37 days). Qualitative review revealed scheduling delays, with “next available booking date” as the most common justification. These delays accounted for 138 excess bed days, equating to an estimated cost of £47,610.
Discussion:
Prolonged waits for PEG placement in otherwise medically fit patients increased hospital bed occupancy and healthcare costs. Delays were logistical, rather than clinical. A targeted intervention involving early PEG referral, streamlined multidisciplinary communication, and onsite PEG insertion by the Upper GI team was introduced.
Conclusion:
Delayed PEG insertion in postoperative head and neck cancer patients leads to avoidable hospitalisation, financial burden, and may delay adjuvant treatment. Reasons for delay were specific to logistical factors within the unit. Results were presented and led to the implementation of an onsite referral pathway and improved interdepartmental coordination in order to offer a sustainable solution.