JTG 2025 Poster Gallery
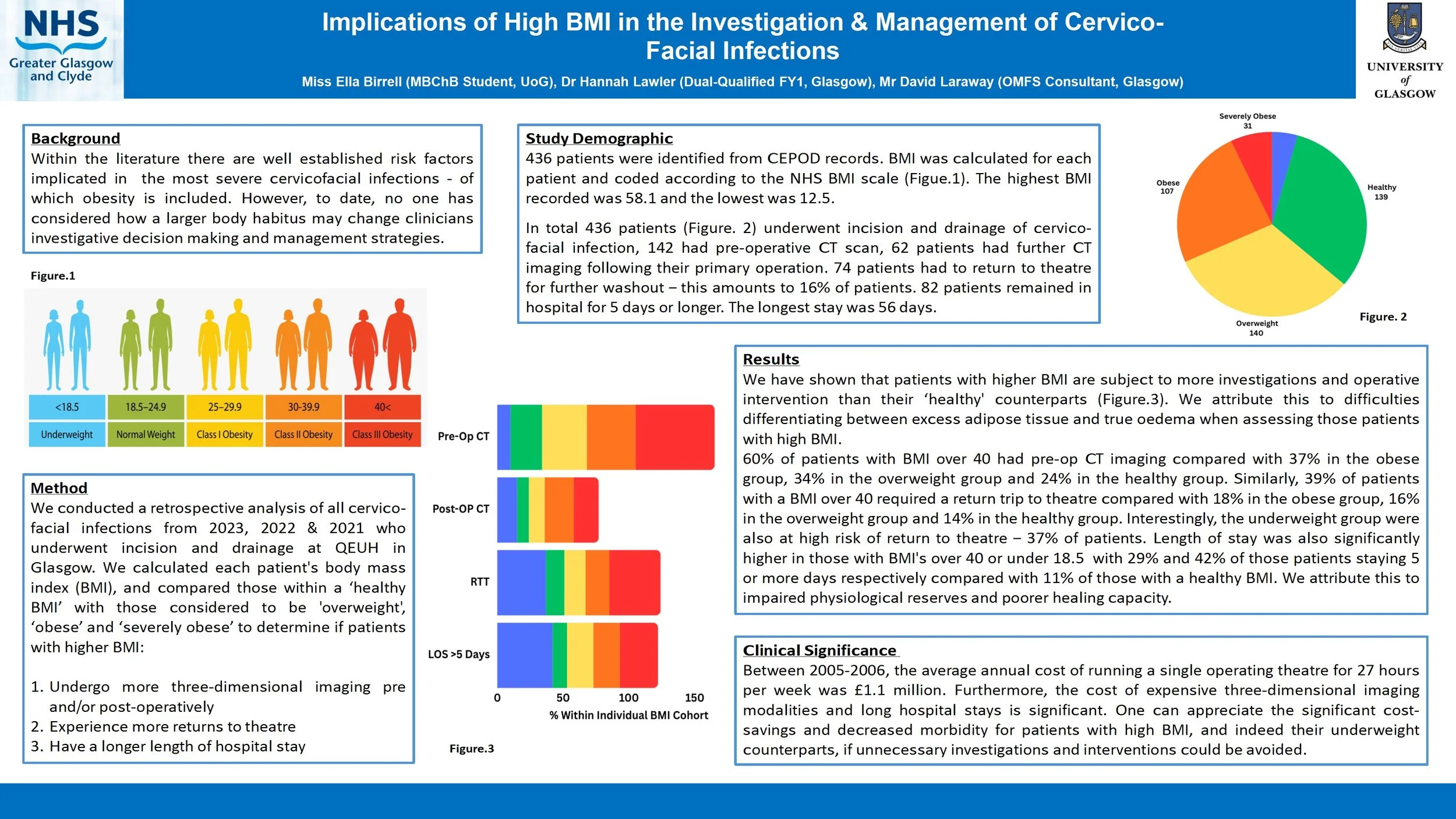
Implications of High BMI in the Investigation & Management of Cervico-Facial Infections
Introduction
Within the literature there are well established risk factors implicated in the most severe cervicofacial infections - of which obesity is included. However, to date, no one has considered how a larger body habitus may change clinicians investigative decision making and management strategies.
Method
We conducted a retrospective analysis of all cervico-facial infections over the last 6 years who underwent incision and drainage at QEUH in Glasgow. We calculated each patient's body mass index (BMI), and compared those within a ‘healthy BMI’ with those considered to be ‘obese’ and ‘morbidly obese’ to determine if patients with higher BMI:
Undergo more three-dimensional imaging pre/post-operatively
Experience more returns to theatre
Have a longer length of hospital stay
Are more likely to require a tracheostomy or intensive care stay
Results
We have shown that patients with higher BMI are subject to more investigations and operative intervention than their ‘healthy BMI’ counterparts. We attribute this to difficulties differentiating between excess adipose tissue and true oedema when assessing those patients with high BMI.
Conclusion
Between 2005-2006, the average annual cost of running a single operating theatre for 27 hours per week was £1.1 million. Furthermore, the cost of expensive three-dimensional imaging modalities and long hospital stays is significant. One can appreciate the significant cost-savings and decreased morbidity for patients with high BMI if unnecessary investigations and interventions could be avoided.
Recurrent Upper Lip Cellulitis Due to MRSA : A Case Report
Abstract
Title: Recurrent Facial cellulitis due to MRSA : a case report.
Introduction
Cellulitis is a common bacterial skin infection that typically responds well to empirical antibiotic therapy. However, recurrent or non-responsive cases may signal underlying resistance, particularly due to community-acquired methicillin-resistant Staphylococcus aureus (MRSA). This report highlights the importance of microbiological diagnosis in guiding effective treatment.
Case Report
A 41-year-old male with a history of recurrent cellulitis presented with spreading erythema over the right perioral region following manipulation of a pimple. His general practitioner prescribed oral co-amoxiclav, but symptoms worsened, prompting hospital admission for intravenous flucloxacillin. The infection initially improved, but a small abscess developed and was surgically drained.
Ten days later, the patient reported significant improvement with only residual scarring. However, erythema recurred in the same area one week later. Oral metronidazole was initiated, resulting in partial improvement, but symptoms returned before the course was completed. Microbiological analysis of the drained abscess revealed MRSA, resistant to beta-lactam antibiotics and sensitive only to cotrimoxazole and vancomycin. The patient was transitioned to oral cotrimoxazole, leading to marked and sustained improvement at one-week follow-up.
Discussion
This case underscores the diagnostic challenges in managing recurrent cellulitis. Initial empirical therapy may be ineffective against resistant organisms such as MRSA, delaying recovery and increasing the risk of complications. Early microbiological sampling and sensitivity testing are essential in guiding targeted antibiotic therapy. Clinicians should maintain a high index of suspicion for MRSA in recurrent or non-responsive skin infections and consider culture-directed treatment to optimize outcomes and prevent recurrence.
Large language models in OMFS triage
Introduction:
Accurate triage of OMFS referrals is essential for appropriate care. However, increasing volume and often poor referral quality place strain on consultant time. Large language models (LLMs), such as GPT-3.5 and GPT-4, are emerging as potential decision-support tools. This project combined a scoping review and pilot study to evaluate the effectiveness of LLMs in OMFS referral triage compared to clinicians.
Method:
A scoping review was conducted using the PRISMA-ScR framework to identify literature on LLMs in triage, diagnosis, and referral optimisation. Findings informed a pilot study. Fifty synthetic referrals were constructed using anonymised real-patient case summaries. Original referrals lacked sufficient detail, so synthetic versions were designed to reflect plausible clinical scenarios with adequate information for assessment. Each referral was input into GPT-3.5 and GPT-4 using a standardised prompt requesting: (1) suggested investigations, (2) likely diagnosis, and (3) initial management. Outputs were compared to actual clinical decisions for those cases.
Results:
The review found limited but growing evidence for LLMs in referral triage, with sparse coverage in surgical specialties. In the pilot, GPT-4 showed better clinical alignment than GPT-3.5 across all domains. Both models produced more appropriate suggestions with structured information, but struggled with vague inputs, mirroring challenges in human triage.
Conclusion:
LLMs, particularly GPT-4, show promise as triage adjuncts in OMFS. While not a replacement for clinician judgement, they may help streamline decision-making when referral detail is sufficient. Further validation is needed before clinical implementation.
Case Report: Reconstruction of Labial Commissure, Lip and Buccal Mucosa following Resection of Recurrent Squamous Cell Carcinoma in a Previously Irradiated Field
Background: 70-year-old female previously treated for Squamous Cell Carcinoma (SCC) of the right mandible and right labial commissure represents with a non-healing ulcer on the right labial mucosa extending to the maxillary alveolus. Reconstruction following resection of the SCC poses a significant challenge due to previous radiotherapy associated with treatment of the SCC on the right labial commissure, a field needed in reconstruction of the resected site. The aim of the patient’s treatment being tumour resection, restoration of function and a level of aesthetic restoration.
Methods: Careful consideration of reconstructive flap in this case was needed due to the compromised vascularity of the previously irradiated tissue. A modified Karapandzic flap along with a V-Y flap and placement of Integra intraorally was the treatment modality of choice, conserving nerves, enhancing blood supply as well as providing adequate adaptation and functional restoration.
Results: The selected flaps provided majority stable wound healing, restored oral competence, and preserved speech and oral intake. The patient recovered without major complications.
Conclusion: Oral commissure reconstruction in previously irradiated patients requires meticulous flap selection to optimise vascularity and function. A tailored approach is essential to achieving functional and aesthetic outcomes while satisfying the primary objective of complete tumour excision.
An incidental finding of a Complex Odontoma – A reminder regarding the importance of routine investigations
An incidental finding of a Complex Odontoma – A reminder regarding the importance of routine investigations
Maria-Alexandra Barbu1, Cristina Frezzini1, Iain Varley1
1-Department of Oral and Maxillofacial Surgery Department
Sheffield Teaching Hospitals NHS Foundation Trust
Abstract
Introduction:
Complex odontomas are rare odontogenic tumors composed of a disorganized mass of dental tissues, typically detected during routine radiographic examinations. They represent a developmental anomaly rather than a true neoplasm and are most often diagnosed in the first two decades of life. Although usually asymptomatic, complex odontomas may impede eruption of permanent teeth or alter the normal development of adjacent anatomical structures, warranting early recognition and appropriate management.
Case report:
We report the case of an 11-year-old fit and well female who presented with a complex odontoma of the LR7 region. This was an incidental finding following imaging taken for orthodontic treatment purposes.
We describe the investigation, diagnosis and management of this child’s condition.
Discussion:
This case highlights the incidental detection of a complex odontoma during orthodontic evaluation and underlines the potential implications for tooth eruption and mandibular growth. Multidisciplinary input involving orthodontics and oral and maxillofacial surgery is crucial for establishing an appropriate management plan, balancing surgical intervention with preservation of developing teeth and the inferior alveolar nerve. Early diagnosis allows timely intervention, preventing complications such as impaction, malocclusion, or pathological fracture. Recognition of odontomas as incidental findings on panoramic radiographs emphasizes their significance in orthodontic and pediatric dental practice.
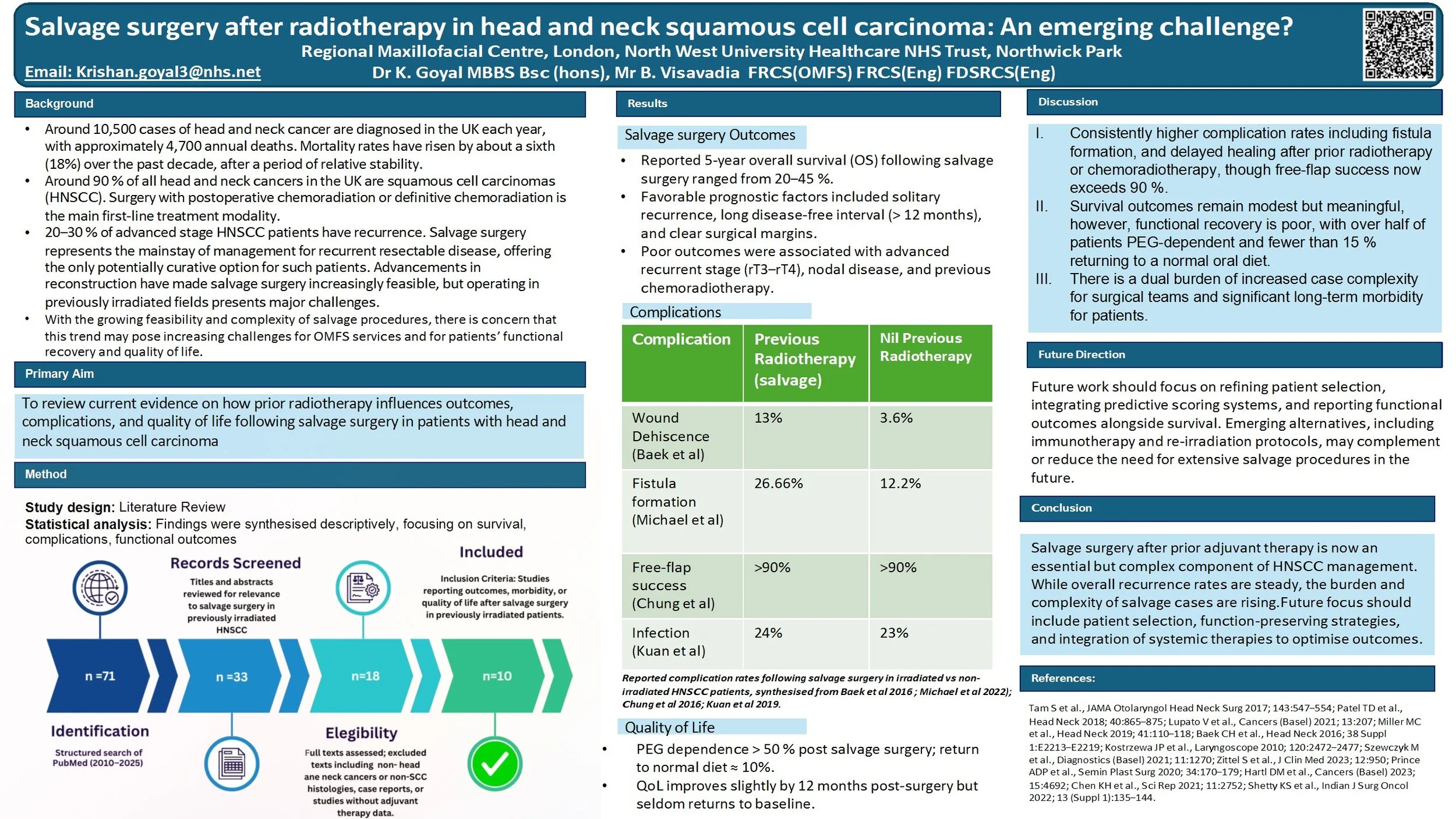
Salvage surgery after radiotherapy in head and neck squamous cell carcinoma: An emerging challenge?
Head and neck squamous cell carcinoma (HNSCC) is often treated with surgery followed by adjuvant radiotherapy or chemoradiotherapy in high-risk cases. While radiotherapy improves initial control, up to 20–30% of patients still develop recurrence. For many, salvage surgery is the only potentially curative option. Advances in microvascular reconstruction now make salvage more feasible, but operating in irradiated tissues carries higher risks and often leaves patients with significant functional difficulties.
Aim:
To review current evidence on how prior radiotherapy influences outcomes and complications of salvage surgery in HNSCC, and to consider the implications for both patients and clinical teams.
Findings:
Five-year overall survival after salvage typically ranges from 20–45%, with the best outcomes seen in solitary, late recurrences. Prognosis is worse with short disease-free intervals, nodal recurrence, or previous adjuvant treatment. Surgery in irradiated fields is associated with greater rates of wound breakdown, fistula and reconstructive failure, though flap survival exceeds 90% in experienced centres. Functionally, many patients remain gastrostomy-dependent and return to a normal diet is rare. Only about one-third of patients with recurrence are suitable candidates for salvage, but the overall number of operations is increasing due to rising cancer incidence, longer survivorship, and wider surgical feasibility.
Discussion:
For patients, salvage after radiotherapy offers a chance of cure but at the cost of higher morbidity and quality-of-life compromise. For clinical teams, these operations are complex, resource-intensive and require multidisciplinary planning.
Conclusion:
Salvage surgery in previously irradiated HNSCC provides hope for selected patients, but remains a demanding intervention with significant risks and functional consequences. Future strategies, including better patient selection, quality-of-life research, and novel systemic options such as immunotherapy, are needed to refine care.
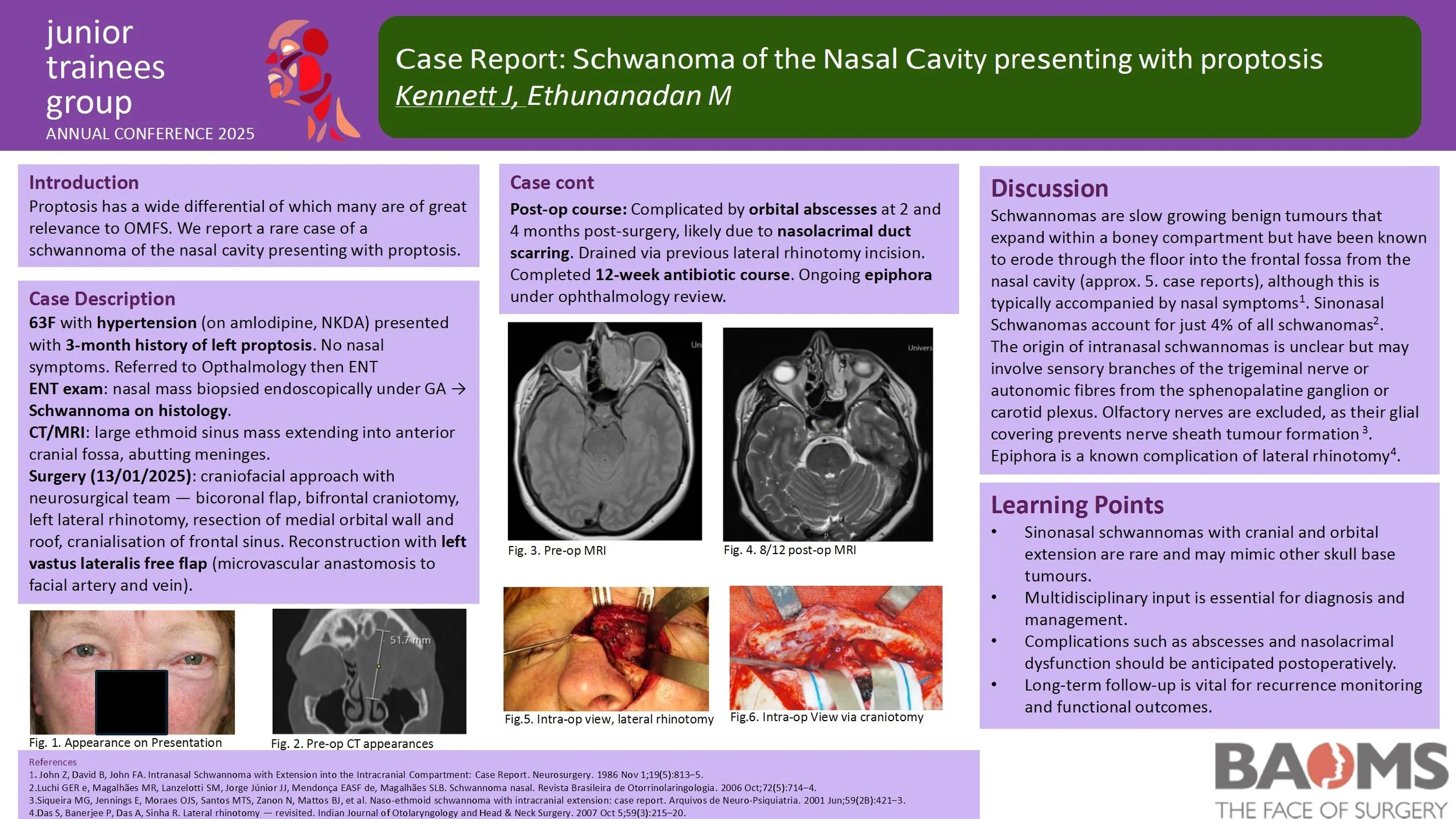
Case Report: Schwanoma of the Nasal Cavity presenting with proptosis
Introduction
Within the literature there are well established risk factors implicated in the most severe cervicofacial infections - of which obesity is included. However, to date, no one has considered how a larger body habitus may change clinicians investigative decision making and management strategies.
Method
We conducted a retrospective analysis of all cervico-facial infections over the last 6 years who underwent incision and drainage at QEUH in Glasgow. We calculated each patient's body mass index (BMI), and compared those within a ‘healthy BMI’ with those considered to be ‘obese’ and ‘morbidly obese’ to determine if patients with higher BMI:
Undergo more three-dimensional imaging pre/post-operatively
Experience more returns to theatre
Have a longer length of hospital stay
Are more likely to require a tracheostomy or intensive care stay
Results
We have shown that patients with higher BMI are subject to more investigations and operative intervention than their ‘healthy BMI’ counterparts. We attribute this to difficulties differentiating between excess adipose tissue and true oedema when assessing those patients with high BMI.
Conclusion
Between 2005-2006, the average annual cost of running a single operating theatre for 27 hours per week was £1.1 million. Furthermore, the cost of expensive three-dimensional imaging modalities and long hospital stays is significant. One can appreciate the significant cost-savings and decreased morbidity for patients with high BMI if unnecessary investigations and interventions could be avoided.
An Audit To Investigate Waiting Times For Patients Requiring Local Anaesthetic Procedures Under The Target Pathway
Introduction
Head and neck cancers represent a significant public health concern in the UK, with rising incidence, mortality rates and late diagnoses. Despite national efforts to streamline diagnostic pathways, delays persist for OMFS referrals. This audit evaluates the efficiency of the diagnostic pathway for suspected malignancies under local anaesthetic procedures (LASP), focusing on adherence to NHS England’s 28-day best-practice timeline, implemented from June 2024.
Method
A retrospective audit was conducted from August to October 2024, reviewing 46 patients referred under the two-week wait (2WW) pathway to OMFS across two sites (BGH and CF). Data was extracted from scheduled LASP lists, patient's documentation, assessing time intervals from referral to clinic, LASP appointments, histology, and follow-up. Comparisons were made with the previous audit cycle to identify trends and areas for improvement.
Results
Only 1 out of 46 patients met the 28-day referral-to-diagnosis target. While 91% of referral forms were dated, just 43% met the recommended 3–6 day upload window. Weekend referrals and ENT triage contributed to delays. LASP was performed within 14 days for 48% of patients, and histology results were available within 21 days for 59%. Malignant diagnoses accounted for 6% of lesions, with a notable increase in dysplastic findings (22%) compared to the previous cycle (7%). Buccal mucosa remained the most commonly biopsied site.
Conclusion
Despite some improvements, significant delays remain in achieving timely diagnosis for head and neck cancer referrals. Key bottlenecks include referral upload times, ENT triage, and limited adherence to the 28-day pathway. Enhanced education for referrers, dedicated LASP slots, and improved triage protocols are recommended to streamline the diagnostic process and improve patient outcomes. Further cycles will aim to include additional sites and refine data collection to support targeted interventions. This audit is targeted for improving patient clinical outcomes, safety and effectiveness of quality care.
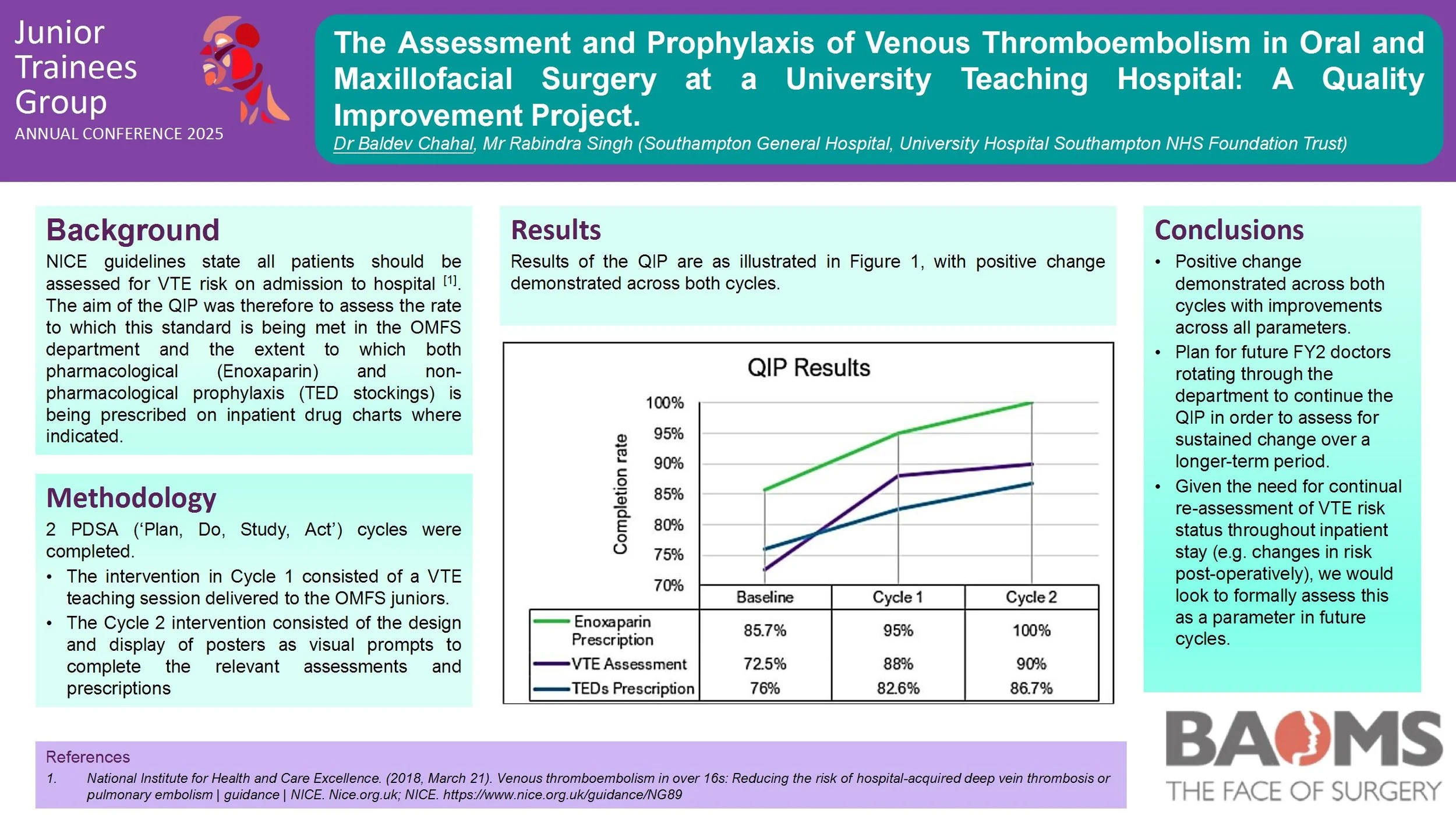
The Assessment and Prophylaxis of Venous Thromboembolism in Oral and Maxillofacial Surgery at a University Teaching Hospital: A Quality Improvement Project.
Introduction
The Oral and Maxillofacial Surgery (OMFS) department is unique in its composition of both medical and dental professionals, with the dental team often unfamiliar with the principles of venous thromboembolism (VTE) prophylaxis prior to commencing their placements. NICE guidelines state all patients should be assessed for VTE risk on admission to hospital. The aims of the QIP involved assessing adherence to this standard in the OMFS department and the extent to which both pharmacological (Enoxaparin) and non-pharmacological prophylaxis (TED stockings) is being prescribed on inpatient drug charts where indicated.
Methods
Baseline data collection was performed to identify areas for performance improvement. 2 PDSA (‘Plan, Do, Study, Act’) cycles were subsequently completed. The intervention in Cycle 1 consisted of a VTE teaching session delivered to the OMFS juniors. The Cycle 2 intervention consisted of the design and display of posters as visual prompts to complete the relevant assessments and prescriptions.
Results
The baseline data collection demonstrated a VTE risk assessment completion rate of 72.5% (29/40). Of the patients assessed to require enoxaparin prophylaxis, this was prescribed on the inpatient drug chart in 85.7% (18/21). Of the patients assessed to be suitable for TED stockings, these were only prescribed on the drug chart in 76% (22/29). Positive change was subsequently demonstrated in Cycle 1 with a risk assessment completion rate of 88% (23/26), enoxaparin prescription completion rate of 95% (19/20) and TEDS prescription rate of 82.6% (19/23). Cycle 2 demonstrated sustained change; risk assessment completion rate of 90% (15/20), enoxaparin prescription rate of 100% (15/15), and TEDS prescription rate of 86.7% (13/15).
Conclusion
Positive change demonstrated across both cycles with improvements across all
parameters. Plan for future FY2 doctors rotating through the department to continue the QIP in order to assess for and implement sustained change over a longer-term period.
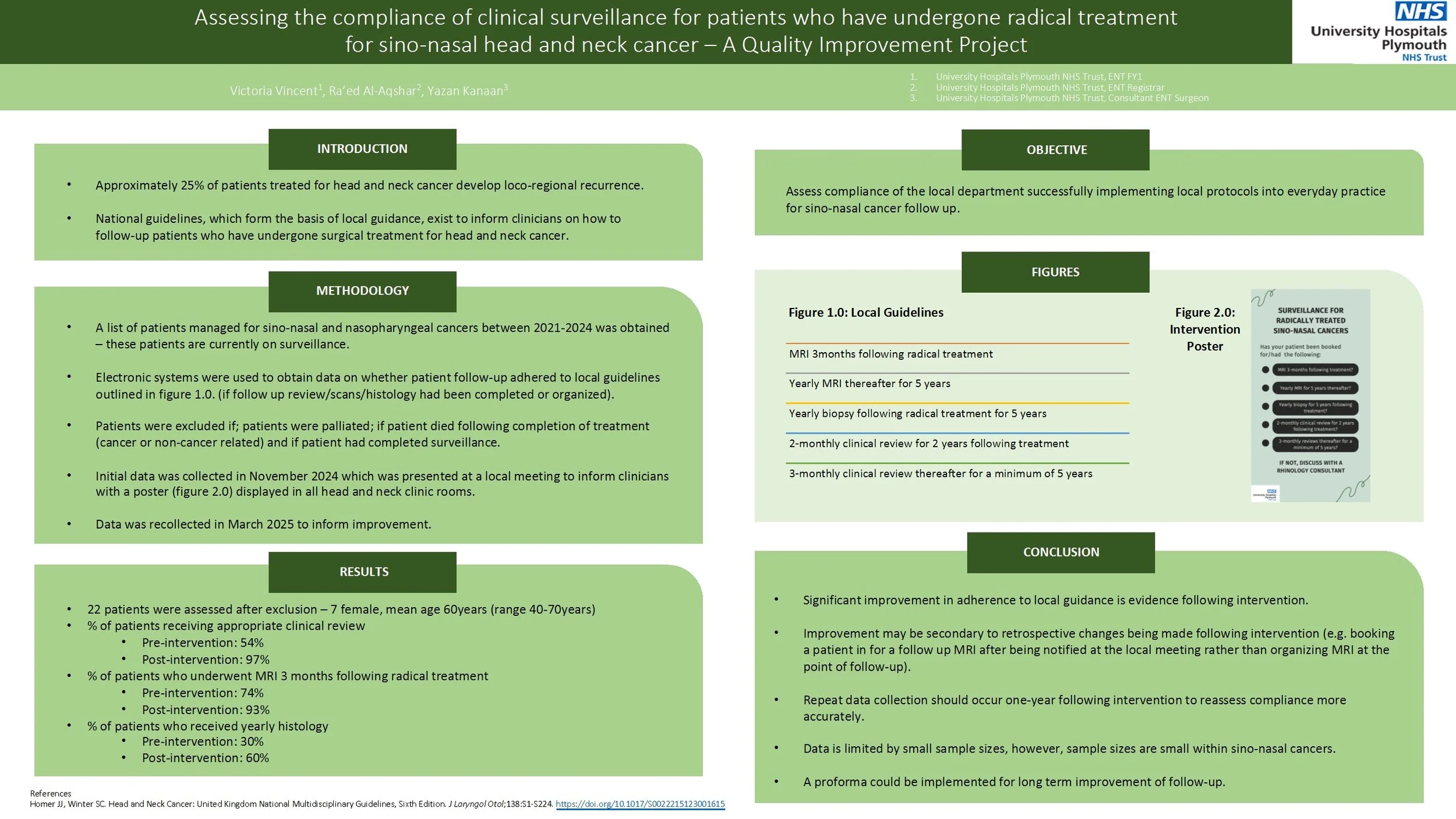
Assessing the compliance of clinical surveillance for patients who have undergone radical treatment for sino-nasal head and neck cancer – A Quality Improvement Project
Approximately 20% of patients treated for head and neck cancer develop loco-regional recurrence. National guidance, which forms the basis of local guidance, exists on how clinicians should follow-up patients following radical surgical treatment for head and neck cancer. The aim of the quality improvement project was to assess whether patients were being adequately followed up following radical management of sino-nasal cancers based upon local guidance.
Patients who underwent radical management of sino-nasal and nasopharyngeal cancers between 2020-2023 at one South West Trust were assessed using available online databases. Compliance to local guidance regarding follow up was assessed. Patients were excluded if they were palliated or if the patient died during treatment. Following the first cycle, the data was presented at the local departmental teaching and a poster reminding clinicians of the follow up criteria was implanted within clinic rooms. Data was then recollected 3 months later.
40 patients were coded as having new sino-nasal cancers. 22 patients were assessed after exclusion. There was improvement in the percentage of patients who had clinical review arranged within the correct timeframe from 54% to 97%. Percentage of patients who had an MRI arranged improved from 74% to 93%. Percentage of patients who had a biopsy arranged improved from 30% to 60%.
Although improvement was achieved within this audit, there were limitations within the study. Namely, the leading clinician was able to identify the patients who did not have correct follow up arranged from the initial audit cycle and arranged this himself, thus not demonstrating a direct link between intervention and change. There were also small sample sizes, however, this reflects the nature of the cohort of patients with sino-nasal cancers. Recommendations would include re-auditing at 1-2years to assess for continued improvement and to obtain more data.
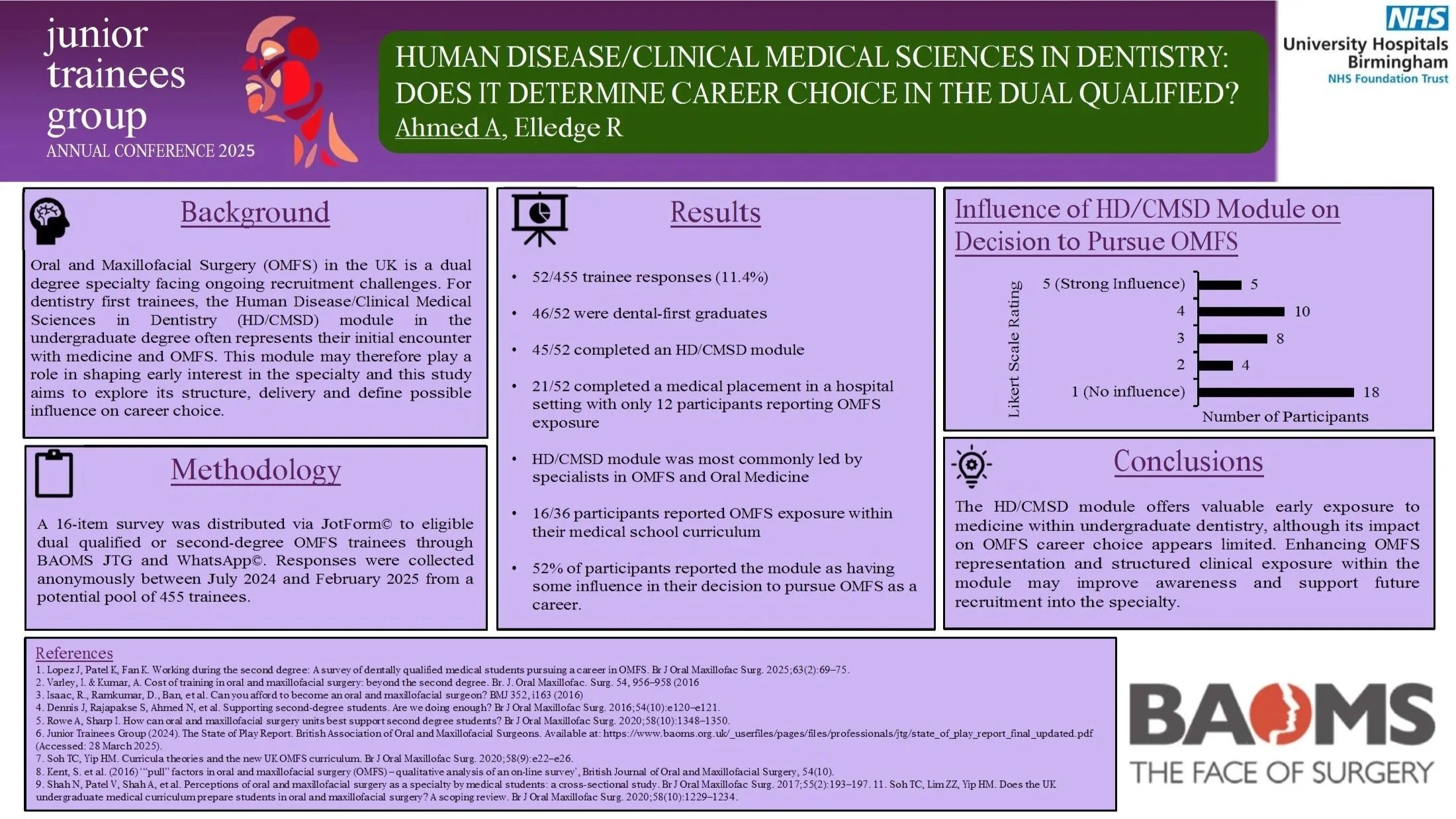
Human Disease/Clinical Medicine in Dentistry: Does it Determine Career Choice in the Dual Qualified?
Introduction: Oral and Maxillofacial Surgery (OMFS) in the UK is a dual degree specialty facing ongoing recruitment challenges. For dentistry first trainees, the Human Disease/Clinical Medical Sciences in Dentistry (HD/CMSD) module in the undergraduate degree often represents their initial encounter with medicine and OMFS. This module may therefore play a role in shaping early interest in the speciality and this study aims to explore its structure, delivery and define possible influence on career choice.
Methods: A 16-item survey was distributed via Jotform© to eligible dual qualified or second-degree OMFS trainees through BAOMS JTG and WhatsApp©. Responses were collected anonymously between July 2024 and February 2025 from a potential pool of 455 trainees.
Results: 52 trainees responded (response rate 11.4%) with 46/52 being dental-first graduates. 45/52 completed an HD/CMSD module, typically delivered a summative assessment. 21/52 completed a medical placement in a hospital setting as part of the module with only 12 participants reporting OMFS exposure within the placement. Leadership of the module varied with specialists in OMFS and Oral Medicine (OM) being the most common. 16/36 participants reported OMFS exposure within their medical school curriculum. 27/52 participants reported the module as having some influence in their decision to pursue OMFS as a career.
Conclusion: The HD/CMSD module offers valuable early exposure to medicine within undergraduate dentistry, although its impact on OMFS career choice appears limited. Enhancing OMFS representation and structured clinical exposure within the module may improve awareness and support future recruitment into the specialty.
Improving Compliance with Anticoagulant and Antiplatelet Guidelines in Minor Oral Surgery: A Quality Improvement project
Introduction:
The Scottish Dental Clinical Effectiveness Programme (SDCEP) published updated guidance in 2022 regarding the management of patients taking oral anticoagulant and antiplatelets for dental treatment including biopsies.
The aim of this audit is to investigate the outpatient clinic’s current compliance with SDCEP 2022 guidance. This involves reviewing the documentation of dictated letters and communication of pre-operative advice related to anticoagulant and anti-platelet therapy. All patients should be receiving appropriate and documented advice regarding their medications prior to surgery.
Method:
20 consecutive patients were selected between 25/01/25 and 28/02/25 from the MOS clinics. Inclusion criteria comprised patients having a planned local anaesthetic dentoalveolar procedure, such as a dental extraction or intra-oral biopsy, and take anticoagulant and/or antiplatelet.
Results:
Of the 20 patients, 8 received correct and documented pre-operative information regarding their medication. However,12 patients had no documented medication advice. Assuming patients continued their medications as usual, 7 patients would have managed their medications appropriately, while 5 would have done so incorrectly.
The primary issue identified among patients not receiving correct advice was the failure to instruct patient to withhold their morning doses of DOACs for high-risk bleeding procedures, such as intra-oral biopsies. To address these gaps, a teaching session will be delivered for all clinicians.
Conclusions:
Accurate documentation of pre-operative instructions regarding anticoagulants and anti-platelets is essential to minimise risk of post-operative complications and to mitigate potential medico-legal risks. This audit has highlighted key areas for improvement.
To ensure sustained improvement, a third cycle audit is recommended in six months to reassess compliance with SDCEP guidelines and evaluate the effectiveness of implemented changes.
What advice did second-degree students have for prospective students on reducing the impact of part-time employment on their medical education?
Introduction:
Student finance provisions for the second degree can be complex, with some finance agencies having specific policies for graduate-entry students who have previously studied medicine or dentistry. Second-degree students may take up part time employment during their studies to maintain clinical skills or to allow for the financing of their course in addition to other living costs. Doctors and dentists have several employment options available to them although these may be during unsocial hours owing to the full-time nature of medicine and dentistry courses.
Methods:
This qualitative research study investigated the impact of employment on medical education during the second degree. In addition to educational impact, also explored were the reasons for taking on employment and what advice participants may have for prospective students on minimising impact. In total, 7 participants were interviewed over Microsoft Teams, following recruitment via a social media post. Those recruited were all dentistry-first and studied medicine as the second-degree. Participants were interviewed using a standardised interview schedule.
Results:
Participants reported both positive and negative impacts of work on medical education and the primary reason for working was financial. Positive impacts included maintenance and development of clinical skills, building of professional relationships and improved teaching skills. The predominant negative impact was that of tiredness, with additional negative impacts being loss of study time and poor academic performance.
Conclusion:
Second-degree students reported positive and negative impacts to their medical education as a result of part-time work during studies. Many expressed a desire for greater financial support during the second degree. Incidental findings also revealed other impacts to the student experience unrelated to medical education.
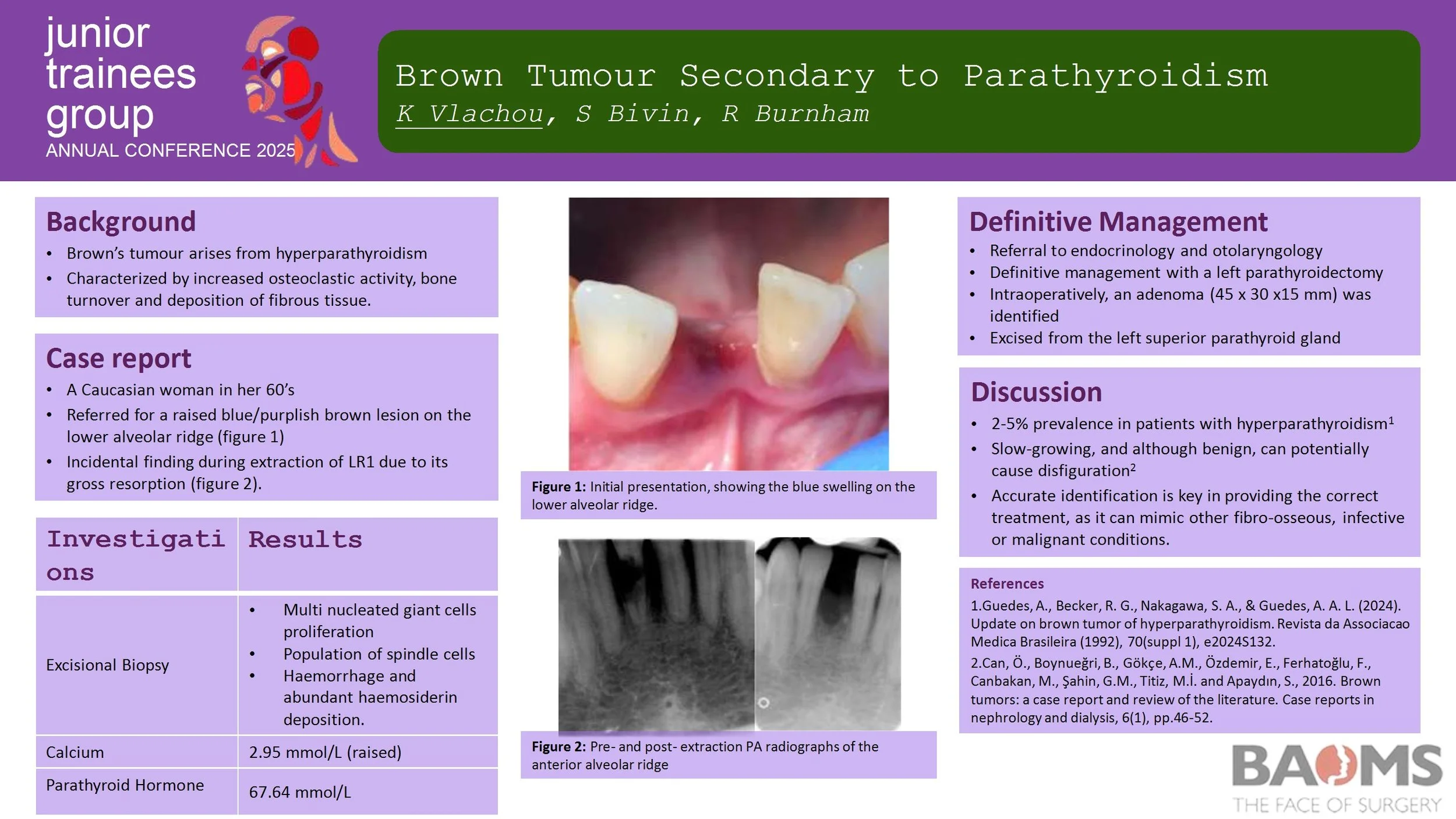
Brown Tumour Secondary to Parathyroidism
Introduction
Brown’s tumour (osteitis fibrosa cystica) is a rare, non-neoplastic condition resulting from hyperparathyroidism. It is characterized by increased osteoclastic activity and bone turnover, which subsequently leads to the deposition of fibrous tissue. It generally affects long bones of the body, however it can affect facial bones, particularly the mandible. It can mimic other fibro-osseous, infective or malignant conditions.
Case Report
We report the case of a 67-year-old female with primary hyperparathyroidism. The initial swelling was found incidentally during an extraction. Radiographic appearance reported root resorption to adjacent teeth, whilst histological findings consisted of the typical multi-nucleated giant cells. Increased blood calcium and parathyroid hormone levels have confirmed primary impression.
Discussion
Brown's tumour is often a diagnostic challenge as it is misdiagnosed, particularly as a malignant lesion. Early detection is key in order to provide the appropriate treatment not only for the lesions but also for the underlying HPT.
Rim Mandibulectomy: Safe, even in the face of understaging?
Background:
Bony invasion in oral squamous cell carcinoma (SCC) is a poor prognostic factor. It is diagnosed preoperatively utilising staging scans and periosteal stripping. Tumours with invasion into the medulla typically require segmental mandibulectomy (SM) to ensure oncological clearance. A more conservative rim/marginal mandibulectomy (RM) may be performed in cases of close tumour proximity to bone or cortical erosion. However, this procedure may risk under-treatment if the preoperative assessments underestimate the extent of bone invasion.
This retrospective cohort study explores the suitability of RM as a conservative alternative to SM in select patients.
Methods:
Patients undergoing mandibulectomy for SCC at a UK OMFS centre between 2018-2023, with >24months follow-up, were identified. Primary outcomes are survival and recurrence, analysed using multivariate regression. Subgroup analysis will be performed on RM patients who subsequently demonstrate histological medullary involvement.
Results:
RM (n=26) and SM (n=30) patients met inclusion criteria. Regression modelling did not identify RM or SM procedures as a significant factor in patient outcomes (p>0.9). Histological medullary involvement was found in 6 RM patients (23%). Survival outcomes and recurrences in these patients were not significantly different to the wider RM group. Presence of bone margin clearance of 5mm was significantly related to survival outcomes.
Conclusions:
Findings continue to support RM as a safe surgical option, even with inherent risk of under-staging. However, preoperative diagnostic accuracy is key to reducing the risks. A further 10 patients have been identified for analysis and will also be presented in the dataset.
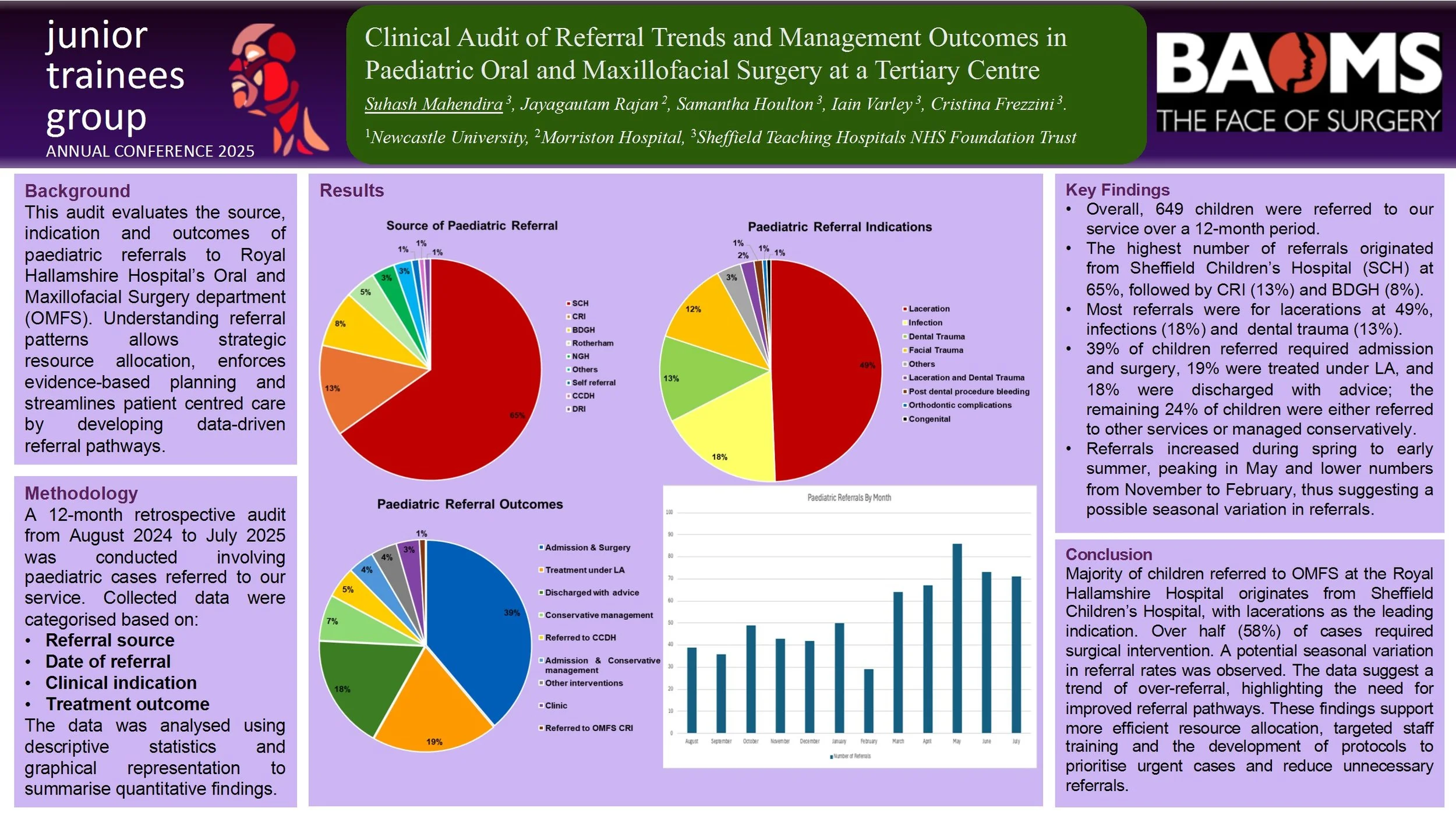
Clinical Audit of Referral Trends and Management Outcomes in Paediatric Oral and Maxillofacial Surgery at a Tertiary Centre
Introduction: Efficient referral pathways are crucial for prompt and exceptional paediatric surgical care. This audit evaluates the trend, demography and outcomes of paediatric referrals to Royal Hallamshire Hospital’s Oral and Maxillofacial Surgery department (OMFS). The understanding of referral patterns allows for strategic resource allocation, enforces evidence-based planning and streamlines patient centred care by developing data-driven referral pathways.
Methods: A retrospective audit was conducted involving 649 paediatric patients referred to our institution over a 12-month period (August 2024 to July 2025). The data was categorised according to referral source, date, clinical indication and subsequent management. The data was analysed using descriptive statistic and graphical representation for ease of interpretation.
Results: Preliminary analysis revealed a sizeable variation in referral sources and clinical indications. A notable portion of referrals originate from Sheffield Children’s Hospital (65%) with laceration (49%) being the major indication of referral. Majority of paediatric patients underwent admission and surgery at 39% followed by treatment under local anaesthesia (LA) at 19%. This audit also indicates the highest frequency of referrals are in the month of May at 86, inversely February reported the lowest frequency at 29.
Conclusion: The trend demonstrates significant seasonal variation and potential over-referral in certain categories. This audit emphasizes the need for closer cooperation and clear communication channels between primary care providers, district hospitals and other tertiary centres. The findings provide actionable insights to guide resource allocation, informed decision making and infrastructure development. Enhanced triage protocols, appropriate staff education, and adequate manpower could mitigate unnecessary hospital referrals and encourages timely interventions of high priority cases.
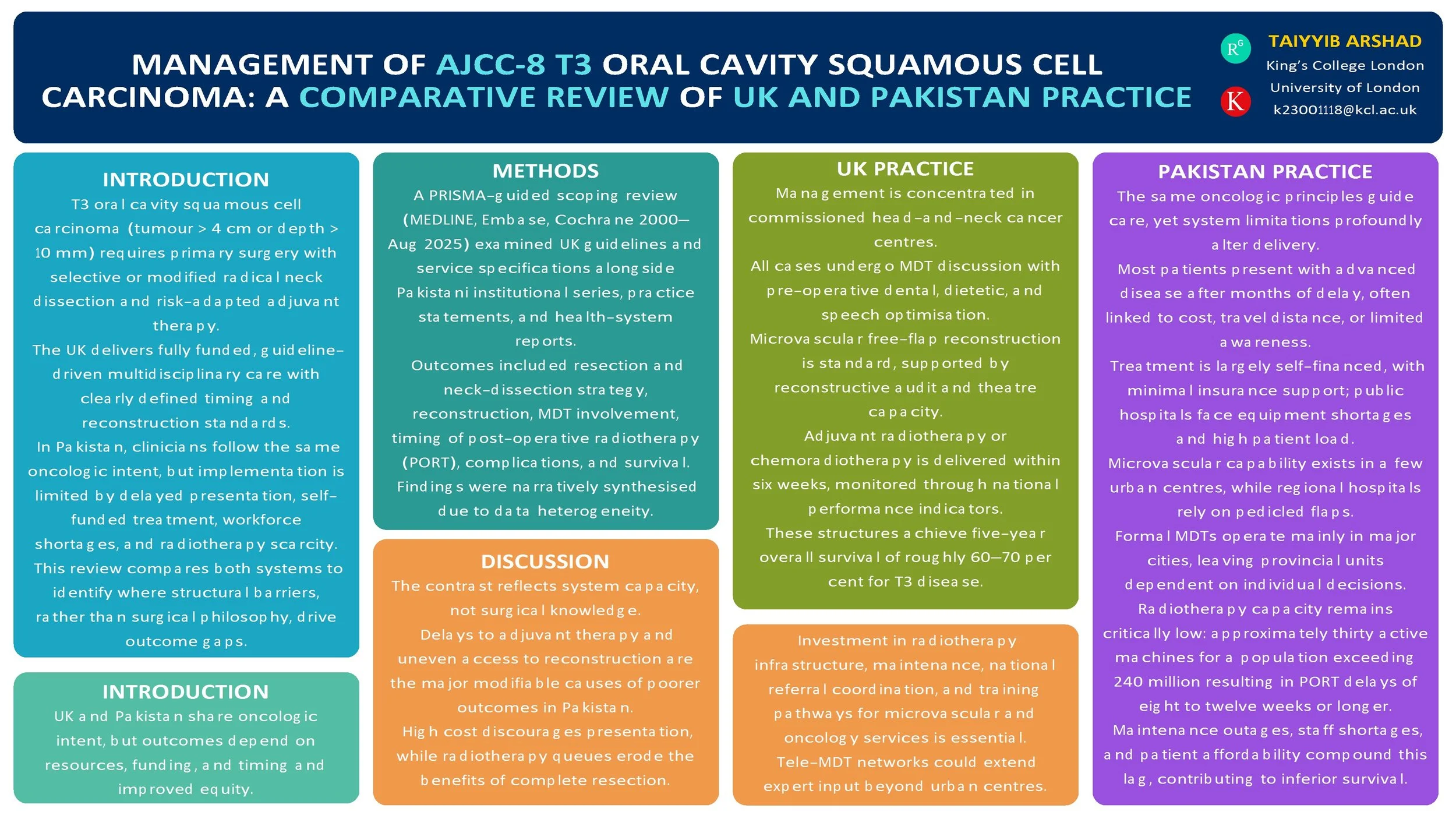
Management of AJCC-8 T3 Oral Cavity Squamous Cell Carcinoma: A Comparative Review of UK (NICE) and Pakistan Practices
Introduction
T3 oral cavity squamous cell carcinoma (OCSCC; AJCC-8: tumour > 4 cm or depth of invasion > 10 mm) is managed with primary surgery and risk-adapted adjuvant therapy. The UK delivers guideline-driven multidisciplinary care, while Pakistan applies the same oncologic principles within more heterogeneous resource settings. We compared published guidance and real-world practice to identify convergences, gaps, and opportunities for pathway improvement.
Method
PRISMA-guided scoping review (MEDLINE, Embase, Cochrane, and grey literature, 2000–Aug 2025). We included: (i) UK guidelines/standards for oral cavity cancer; (ii) Pakistan institutional series and practice statements for T3 OCSCC; (iii) health-system reports on multidisciplinary team (MDT) availability and radiotherapy capacity. Outcomes: resection and neck-dissection strategy, reconstruction modality, positive margins, time to post-operative radiotherapy (PORT), complications, recurrence, and survival. Data were charted narratively due to heterogeneity.
Results
UK sources consistently recommend upfront resection with appropriate ipsi/contralateral neck dissection, microvascular reconstruction when indicated, and adjuvant RT/CRT for adverse features, delivered through MDT pathways with staging, dental, and nutritional optimisation. Pakistan tertiary centres report adherence to core surgical principles with growing microvascular capability; regional flaps are used where resources are constrained. Across Pakistan reports, later stage at presentation is common; MDT access and radiotherapy capacity vary, contributing to PORT delays. Broader head-and-neck literature links delayed PORT (>6 weeks) with inferior outcomes. No head-to-head UK–Pakistan comparative cohort specific to T3 OCSCC outcomes was found.
Conclusion
Oncologic intent is aligned, but system-level factors—MDT coverage, reconstructive resources, and timely access to PORT—likely drive differences in delivered care and outcomes. Standardised, context-adapted pathways (routine MDT triage, clear neck algorithms, reconstruction choice matched to resources, and fast-tracked PORT) and a bi-national registry focused on T3 OCSCC are warranted to benchmark timing, treatment patterns, and outcomes.
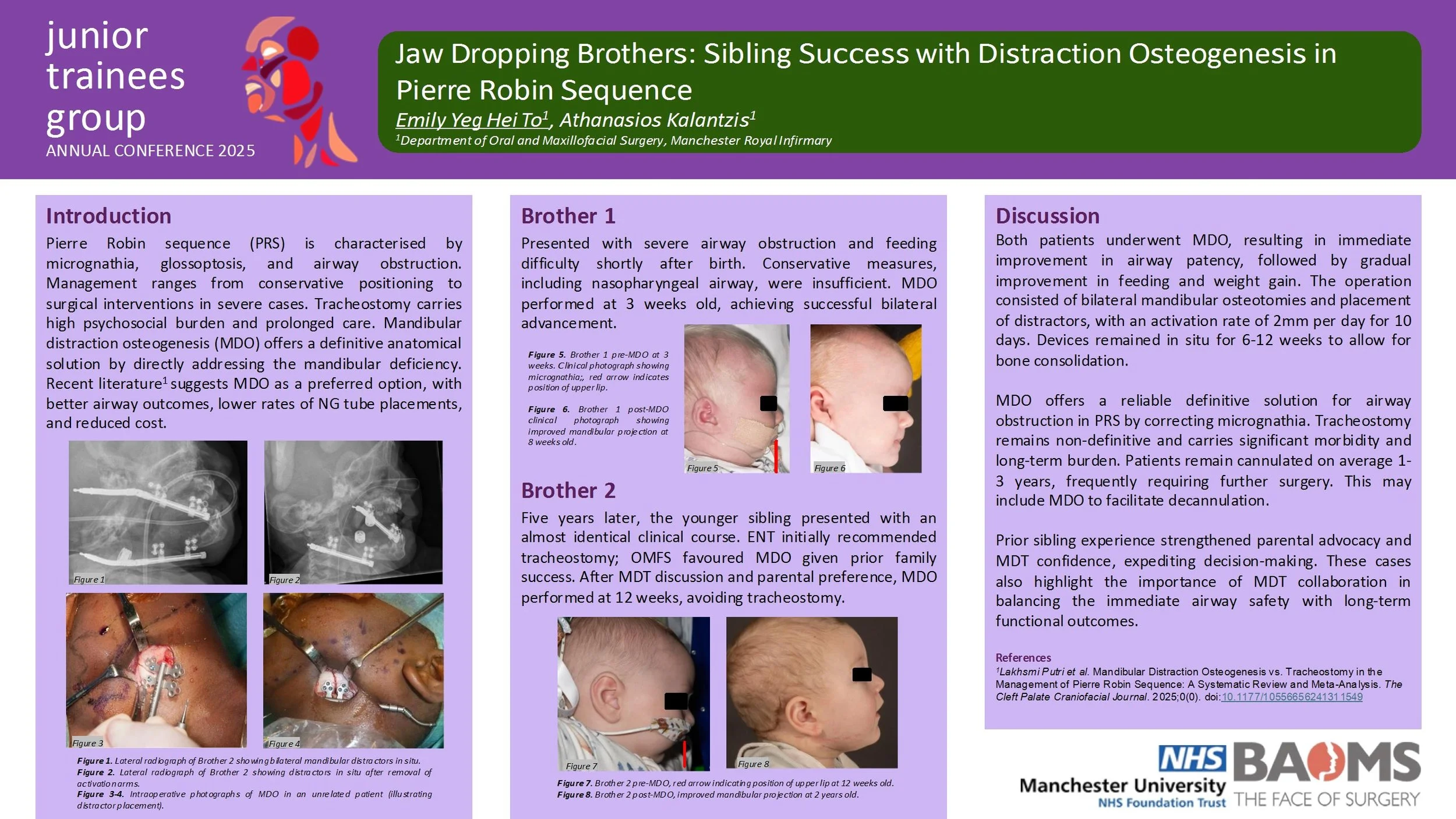
Jaw Dropping Brothers: Sibling Success with Distraction Osteogenesis in Pierre Robin Sequence
Reducing Delays to PEG Insertion in Postoperative Head and Neck Cancer Patients: A Quality Improvement Project
Introduction:
Patients undergoing major head and neck cancer surgery can experience postoperative dysphagia requiring percutaneous endoscopic gastrostomy (PEG) for nutrition. For those not pre-emptively fitted with PEGs, delays in post-operative PEG insertion can prolong hospitalisation, recovery, and initiation of adjuvant treatment. This quality improvement project aimed to quantify these delays, assess their impact, and implement interventions to streamline care.
Methods:
A retrospective review of all postoperative head and neck cancer patients admitted to a specialist ward, in a single centre, between January 2024, and June 2025, requiring inpatient PEG insertion was done. Data included demographics, surgical details, PEG indication, time from PEG request to insertion, and length of hospital stay. Financial impact was calculated using standard NHS bed day costs.
Results:
Five patients met inclusion criteria. All had extensive surgical procedures including bilateral neck dissections and tracheostomy. Median time from PEG request to insertion was 33 days (range: 12–37 days). Qualitative review revealed scheduling delays, with “next available booking date” as the most common justification. These delays accounted for 138 excess bed days, equating to an estimated cost of £47,610.
Discussion:
Prolonged waits for PEG placement in otherwise medically fit patients increased hospital bed occupancy and healthcare costs. Delays were logistical, rather than clinical. A targeted intervention involving early PEG referral, streamlined multidisciplinary communication, and onsite PEG insertion by the Upper GI team was introduced.
Conclusion:
Delayed PEG insertion in postoperative head and neck cancer patients leads to avoidable hospitalisation, financial burden, and may delay adjuvant treatment. Reasons for delay were specific to logistical factors within the unit. Results were presented and led to the implementation of an onsite referral pathway and improved interdepartmental coordination in order to offer a sustainable solution.
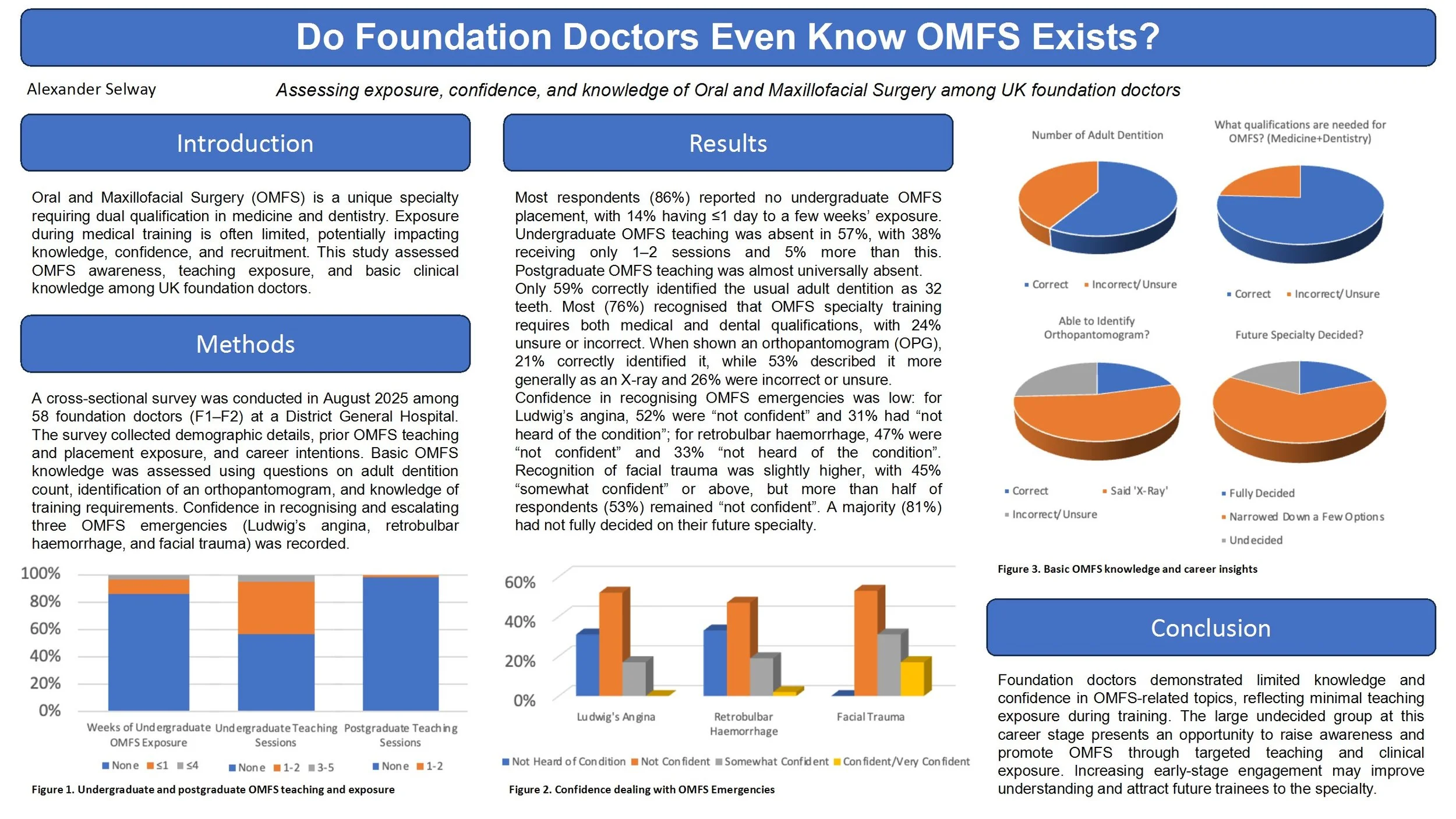
Do Foundation Doctors Even Know OMFS Exists? Assessing exposure, confidence, and knowledge of Oral and Maxillofacial Surgery among UK foundation doctors
Introduction
Oral and Maxillofacial Surgery (OMFS) is a unique specialty requiring dual qualification in medicine and dentistry. Exposure during medical training is often limited, potentially impacting knowledge, confidence, and recruitment. This study assessed OMFS awareness, teaching exposure, and basic clinical knowledge among UK foundation doctors.
Methods
A cross-sectional survey was conducted in August 2025 among 58 foundation doctors (F1–F2) at a District General Hospital. The survey collected demographic details, prior OMFS teaching and placement exposure, and career intentions. Basic OMFS knowledge was assessed using questions on adult dentition count, identification of an orthopantomogram, and knowledge of training requirements. Confidence in recognising and escalating three OMFS emergencies (Ludwig’s angina, retrobulbar haemorrhage, and facial trauma) was recorded.
Results
Most respondents (86%) reported no undergraduate OMFS placement, with 14% having ≤1 day to a few weeks’ exposure. Undergraduate OMFS teaching was absent in 57%, with 38% receiving only 1–2 sessions and 5% more than this. Postgraduate OMFS teaching was almost universally absent. Only 59% correctly identified the usual adult dentition as 32 teeth. Most (76%) recognised that OMFS specialty training requires both medical and dental qualifications, with 24% unsure or incorrect. Confidence in recognising Ludwig’s angina was low, with 52% “not confident” and 31% “not heard of condition”. For retrobulbar haemorrhage, 47% “not confident” and 33% “not heard of condition”. Facial trauma recognition had slightly higher confidence (45% “somewhat confident” or above), but more than half of respondents (53%) remained “not confident”. A majority (81%) had not fully decided on their future specialty.
Conclusions
Foundation doctors demonstrated limited knowledge and confidence in OMFS-related topics, reflecting minimal teaching exposure during training. The large undecided group at this career stage presents an opportunity to raise awareness and promote OMFS through targeted teaching and clinical exposure. Increasing early-stage engagement may improve understanding and attract future trainees to the specialty.
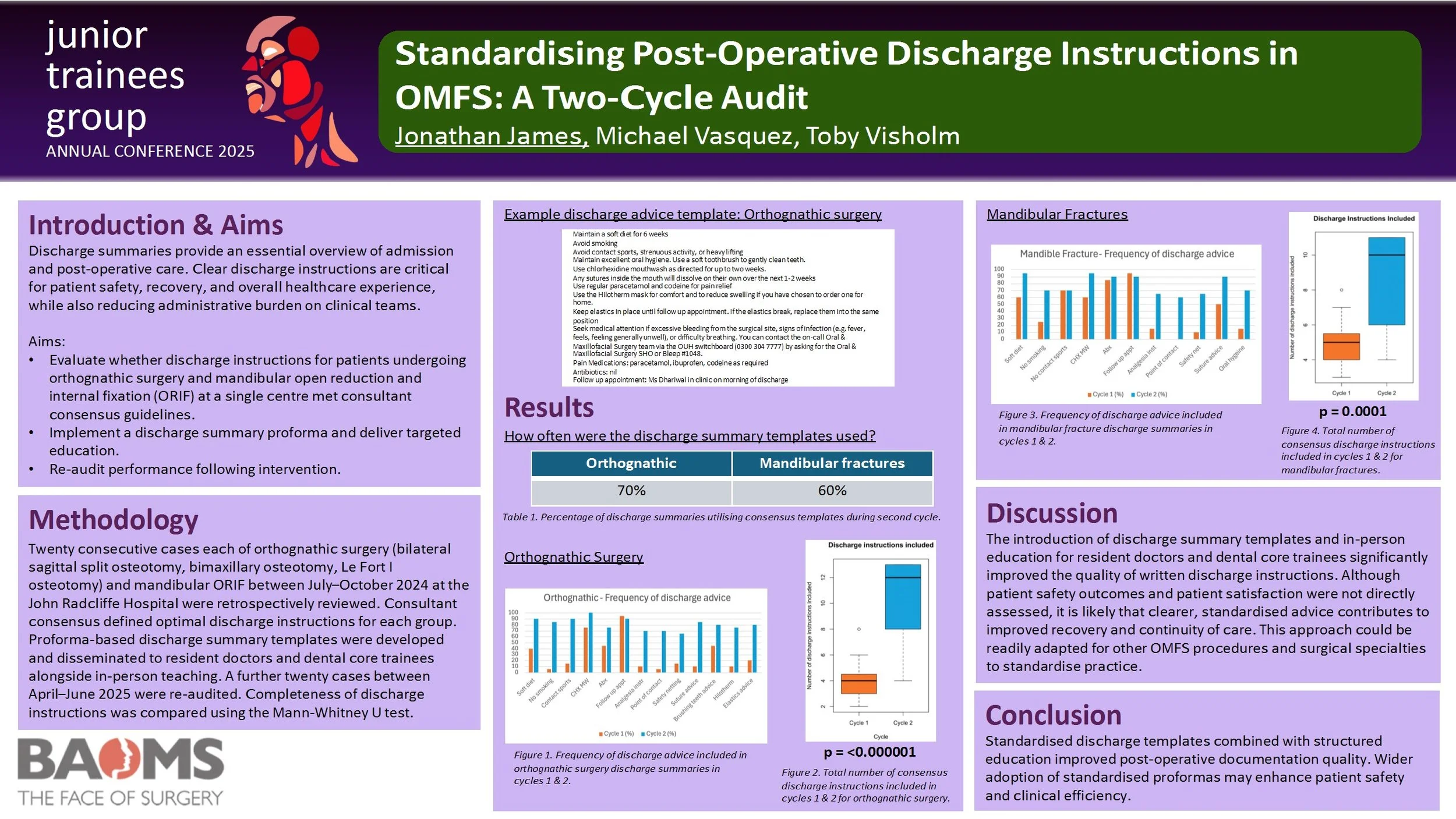
Standardising Post-Operative Discharge Instructions in OMFS: A Two-Cycle Audit
Introduction
Discharge summaries provide an essential overview of admission and post-operative care. Clear discharge instructions are critical for patient safety, recovery, and overall healthcare experience, while also reducing administrative burden on clinical teams.
Aims
1. To evaluate whether discharge instructions for patients undergoing orthognathic surgery and mandibular open reduction and internal fixation (ORIF) at a single centre met consultant consensus guidelines.
2. To implement a discharge summary proforma with targeted education.
3. To re-audit performance following intervention.
Methods
Twenty consecutive cases of orthognathic surgery (bilateral sagittal split osteotomy, bimaxillary osteotomy, Le Fort I osteotomy) and mandibular ORIF between July–October 2024 at the John Radcliffe Hospital were retrospectively reviewed. Consultant consensus defined optimal discharge instructions for each group. Proforma-based discharge summary templates were developed and disseminated to resident doctors and dental core trainees alongside in-person teaching. A further twenty cases between April–June 2025 were re-audited. Completeness of discharge instructions was compared using the Mann-Whitney U test.
Results
In the second cycle, templates were used in 70% of orthognathic cases and 60% of mandibular fracture cases. There was a significant improvement in the total number of relevant discharge instructions included for both orthognathic surgery (p = 0.0000006) and mandibular fractures (p = 0.0001).
Discussion
The introduction of discharge summary templates and in-person education for resident doctors and dental core trainees significantly improved the quality of written discharge instructions. Although patient safety outcomes and patient satisfaction were not directly assessed, it is likely that clearer, standardised advice contributes to improved recovery and continuity of care. This approach could be readily adapted for other OMFS procedures and surgical specialties to standardise practice.
Conclusion
Standardised discharge templates combined with structured education improved post-operative documentation quality. Wider adoption of standardised proformas may enhance patient safety and clinical efficiency.