JTG 2025 Poster Gallery
Recurrent Upper Lip Cellulitis Due to MRSA : A Case Report
Abstract
Title: Recurrent Facial cellulitis due to MRSA : a case report.
Introduction
Cellulitis is a common bacterial skin infection that typically responds well to empirical antibiotic therapy. However, recurrent or non-responsive cases may signal underlying resistance, particularly due to community-acquired methicillin-resistant Staphylococcus aureus (MRSA). This report highlights the importance of microbiological diagnosis in guiding effective treatment.
Case Report
A 41-year-old male with a history of recurrent cellulitis presented with spreading erythema over the right perioral region following manipulation of a pimple. His general practitioner prescribed oral co-amoxiclav, but symptoms worsened, prompting hospital admission for intravenous flucloxacillin. The infection initially improved, but a small abscess developed and was surgically drained.
Ten days later, the patient reported significant improvement with only residual scarring. However, erythema recurred in the same area one week later. Oral metronidazole was initiated, resulting in partial improvement, but symptoms returned before the course was completed. Microbiological analysis of the drained abscess revealed MRSA, resistant to beta-lactam antibiotics and sensitive only to cotrimoxazole and vancomycin. The patient was transitioned to oral cotrimoxazole, leading to marked and sustained improvement at one-week follow-up.
Discussion
This case underscores the diagnostic challenges in managing recurrent cellulitis. Initial empirical therapy may be ineffective against resistant organisms such as MRSA, delaying recovery and increasing the risk of complications. Early microbiological sampling and sensitivity testing are essential in guiding targeted antibiotic therapy. Clinicians should maintain a high index of suspicion for MRSA in recurrent or non-responsive skin infections and consider culture-directed treatment to optimize outcomes and prevent recurrence.
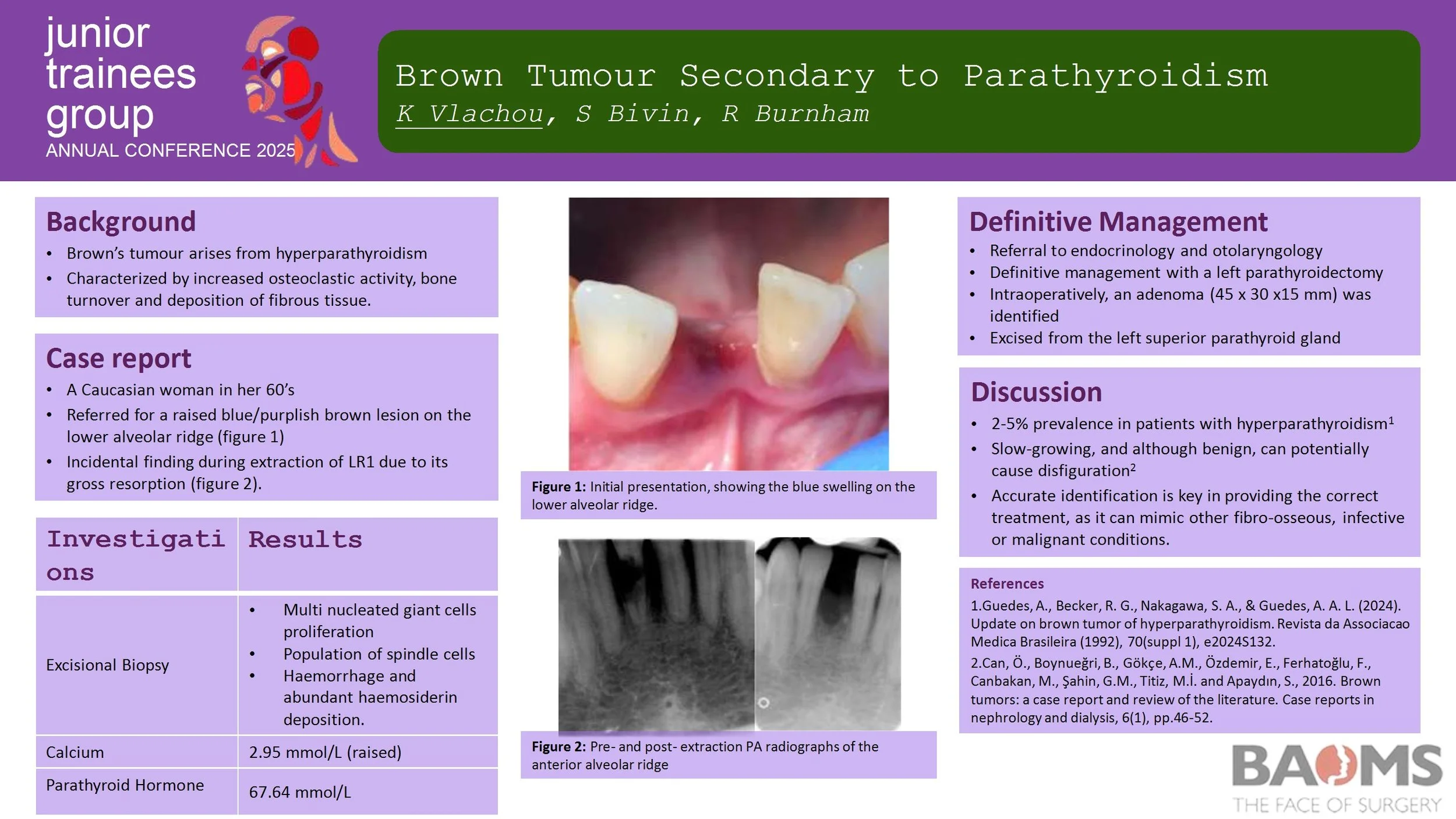
Brown Tumour Secondary to Parathyroidism
Introduction
Brown’s tumour (osteitis fibrosa cystica) is a rare, non-neoplastic condition resulting from hyperparathyroidism. It is characterized by increased osteoclastic activity and bone turnover, which subsequently leads to the deposition of fibrous tissue. It generally affects long bones of the body, however it can affect facial bones, particularly the mandible. It can mimic other fibro-osseous, infective or malignant conditions.
Case Report
We report the case of a 67-year-old female with primary hyperparathyroidism. The initial swelling was found incidentally during an extraction. Radiographic appearance reported root resorption to adjacent teeth, whilst histological findings consisted of the typical multi-nucleated giant cells. Increased blood calcium and parathyroid hormone levels have confirmed primary impression.
Discussion
Brown's tumour is often a diagnostic challenge as it is misdiagnosed, particularly as a malignant lesion. Early detection is key in order to provide the appropriate treatment not only for the lesions but also for the underlying HPT.
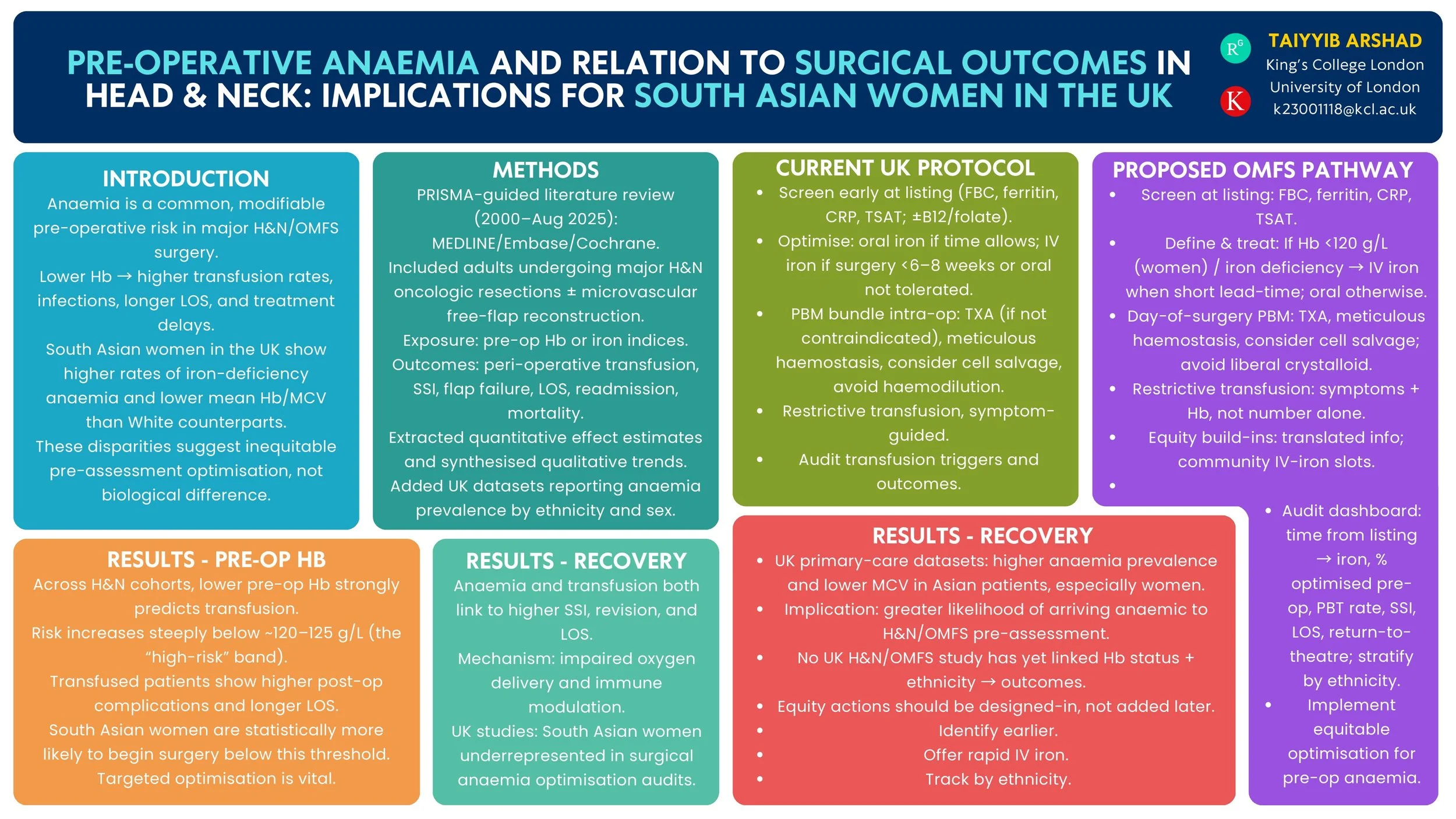
Pre-operative Anaemia and Surgical Outcomes in Head & Neck Surgery: Implications for South Asian Women in the UK
Introduction
Pre-operative anaemia is a modifiable risk factor that increases complications after head & neck (H&N) surgery. UK primary-care data show a higher burden of anaemia among women of Asian heritage than White women. We reviewed the evidence on pre-operative anaemia and H&N/OMFS surgical outcomes and summarised UK epidemiology by ethnicity to inform equity-focused peri-operative pathways.
Method
PRISMA-guided review (MEDLINE/Embase/Cochrane, 2000–Aug 2025). Inclusion: studies of H&N/OMFS surgery reporting pre-operative haemoglobin/iron indices vs peri-operative outcomes (transfusion, surgical-site infection, return to theatre, flap failure, length of stay, readmission, mortality, oncological endpoints). We additionally summarised UK population/primary-care studies reporting anaemia prevalence in women by ethnicity and current UK peri-operative anaemia guidance.
Results
Across H&N cohorts and syntheses, lower pre-operative haemoglobin independently associates with higher peri-operative transfusion and adverse outcomes; a high-risk transfusion threshold is consistently observed around ~120 g/L. UK guidance recommends routine pre-operative screening and optimisation (including intravenous iron) for major surgery. UK primary-care datasets demonstrate higher anaemia prevalence and lower mean haemoglobin/MCV among Asian compared with White patients, indicating that women of South Asian heritage are more likely to present anaemic before surgery. No UK H&N/OMFS study has yet quantified outcome differences by both anaemia status and ethnicity.
Conclusion
Robust evidence links pre-operative anaemia with worse H&N surgical outcomes, and UK datasets show higher anaemia prevalence in Asian women. These findings support a standardised OMFS/H&N anaemia optimisation pathway—early case-finding, iron studies, rapid IV iron, and transfusion-sparing strategies—with particular attention to access and uptake among South Asian women. Future UK multicentre analyses should test whether ethnicity modifies anaemia-related surgical risk and evaluate pathway impact on complications and treatment delays.
Quality Improvement Project – analysing compliance of Russells Hall Hospital OMFS department against SDCEP Anticoagulant guidelines
Introduction
The Royal College of Anaesthetists (RCA) highlights key considerations when selecting anaesthetic modalities, including operator experience, diagnosis severity, and peri-operative compliance. This Quality Improvement Project (QIP) aimed to assess anaesthetic use in secondary care against RCA guidance and develop a long-term strategy to reduce reliance on CEPOD where possible. Benefits include minimising risks of GA-associated mortality, enabling immediate management, reducing anticipatory stress for children and parents, and optimising resource allocation by alleviating CEPOD pressures.
Method
A retrospective pilot cycle was conducted at University Hospital Wales, followed by two prospective cycles at Dudley Group Hospitals and Royal Wolverhampton Trusts. Each cycle included 20 paediatric OMFS presentations from the emergency department. Data collected comprised age, gender, diagnosis, mechanism of injury, pre-operative compliance, management, anaesthetic modality, and peri-operative compliance. Between the second and third cycle, an action plan was presented to paediatric and OMFS teams.
Results
In the first cycle (mean age 4.75; 70% male), 90% were managed with GA, 5% with inhalation sedation, and 5% with LA. The second cycle (mean age 9.7; 75% male) showed 25% GA, 5% inhalation sedation, and 70% LA. In the third cycle (mean age 8; 70% male), 40% were managed with GA, 5% inhalation sedation, 5% ketamine sedation, and 50% with LA.
Conclusion
The QIP demonstrated varied anaesthetic modalities with increasing uptake of sedation between the second and third cycles. Future improvements include implementing a proforma for children undergoing GA to evaluate alternative modalities, ensuring safer, more efficient decision-making. Incorporating Patient Reported Outcomes from parents and children could further inform service development, providing insights into waiting times, cosmetic results, and anxiolysis during treatment.
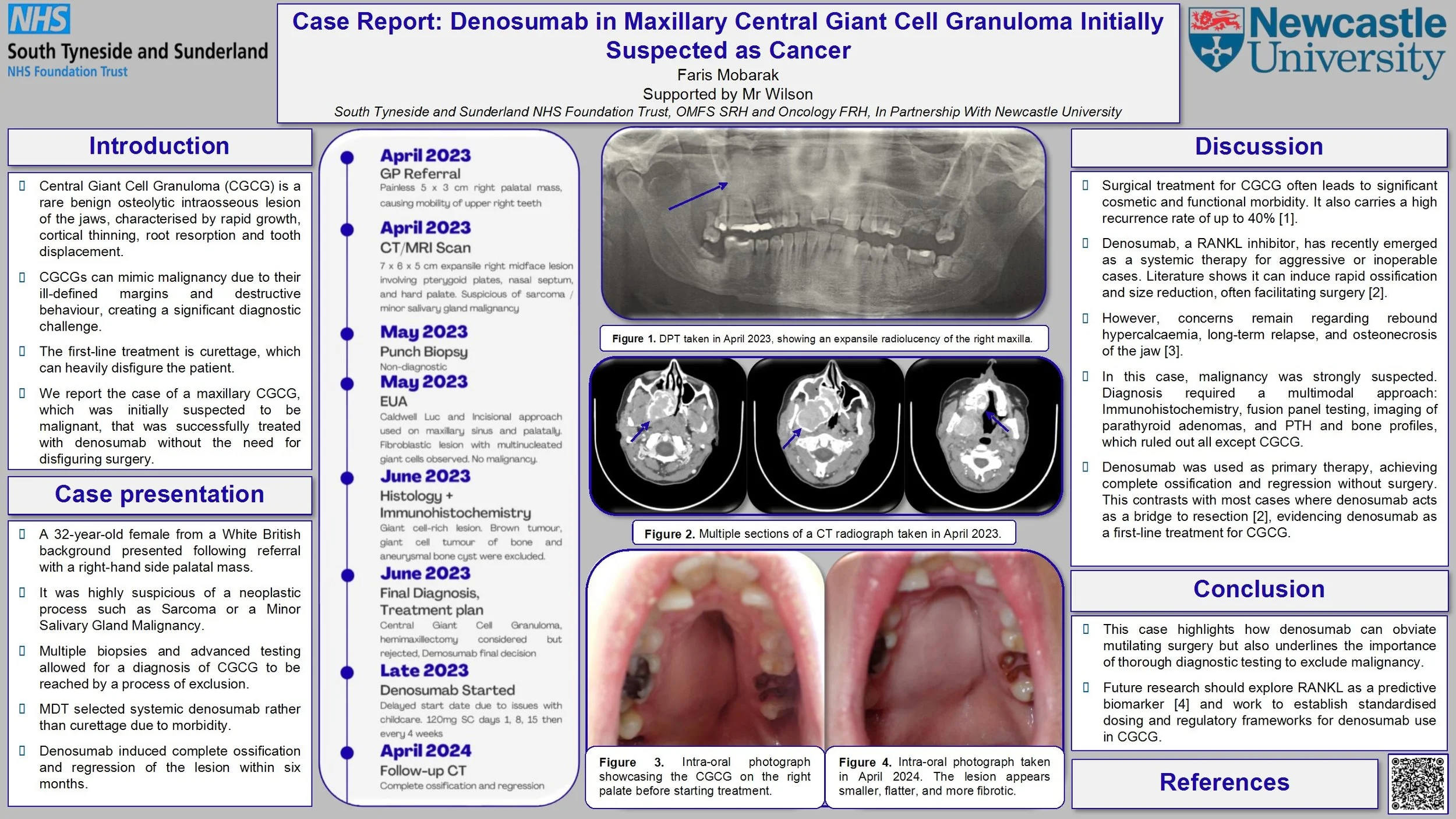
Case Report: Denosumab in Maxillary Central Giant Cell Granuloma Initially Suspected as Cancer
Introduction: Central Giant Cell Granuloma (CGCG) is a benign osteolytic lesion of the jaw that can present with aggressive radiographic features such as cortical thinning, root resorption, tooth displacement, and ill-defined margins that mimic malignancy and risk misdiagnosis. While surgical management remains the first-line therapy for CGCG, this case covers the use of denosumab, which successfully prompted ossification and lesion regression without the need for disfiguring surgery.
Case Report: We report the unusual case of a 32-year-old Caucasian female who presented in April 2023 at an emergency dental appointment with a 5 x 3 cm firm, non-ulcerated right palatal mass and mobile upper right molars. CBCT and MRI demonstrated an ill-defined, expansile, vascular lesion of the right maxilla invading the sinus, nasal floor and pterygoid plates without orbital or intracranial extension. Deep biopsies were taken under GA via Caldwell-Luc and palatal incision. Histology reported a fibro-cellular stroma with numerous osteoclast-type giant cells. Giant cell tumour of bone, aneurysmal bone cyst and brown tumour were excluded by immunohistochemistry testing and blood tests. A multidisciplinary team (MDT) discussion confirmed the diagnosis of CGCG. Given the lesion’s size and location, systemic therapy with denosumab was initiated. Multiple CT scans indicated progressive ossification and reduction in lesion volume following administration of denosumab. At a 12-month follow-up after discontinuation of treatment, the lesion remained stable, with preserved dentition and no functional or aesthetic deficits.
Discussion: Our case illustrates the diagnostic dilemma in CGCG, necessitating deep surgical biopsy, comprehensive immunohistochemistry, and multidisciplinary team coordination to rule out malignancy. It also demonstrates denosumab as an effective, tissue-sparing alternative to the extensive resection typically carried out.
An extensive Odontogenic Keratocyst in the left maxilla: a case report
Odontogenic Keratocysts (OKC) are benign cystic lesions that are known to be locally aggressive and have a high recurrence rate. Here we describe a case of a particularly extensive OKC.
A 28 year-old female presented to the Oral and Maxillofacial department with a 2-month history of facial swelling and pain. On examination, there was a left mid-facial swelling which was extremely tender on palpation, with intra-oral buccal expansion. Medically, she had depression and was a non-smoker. An OPG and CT neck with contrast was carried out; this revealed a substantial lesion, filling the left maxillary sinus, in association with a superiorly impacted UL8 tooth located just below the orbital apex. The lesion had cystic characteristics, measuring 6.6cm vertically, and 5.8 x 3.8cm in a transverse dimension. The lesion was shown to project medially into the nasal cavity, resulting in septal deviation to the right. Superiorly, there was associated convex bulging of the orbital floor.
Subsequently, antibiotics were prescribed; enucleation of the cyst and extraction of UL8 was carried out. The pathology result was in favour of Odontogenic Keratocyst. Infection reoccurred 1 month later which led to a washout of the cystic cavity, placement of a drain, extraction of a resorbed UL6 and additional antibiotic therapy. Gabapentin was then commenced due to associated neuropathic pain. 3 months following initial surgery, further enucleation of a 1x1cm residual cyst was carried out. 6 months later, a repeat CT scan revealed mildly progressive bony infill in line with ongoing healing and no evidence of recurrence.
This case highlights the aggressive nature of the OKC despite their slow growth. The presence of such an expansile lesion in the maxillary sinus with an associated ectopic tooth just below the orbital apex is rare. Close follow-up to detect recurrence is important.