JTG 2025 Poster Gallery
Case Report: Reconstruction of Labial Commissure, Lip and Buccal Mucosa following Resection of Recurrent Squamous Cell Carcinoma in a Previously Irradiated Field
Background: 70-year-old female previously treated for Squamous Cell Carcinoma (SCC) of the right mandible and right labial commissure represents with a non-healing ulcer on the right labial mucosa extending to the maxillary alveolus. Reconstruction following resection of the SCC poses a significant challenge due to previous radiotherapy associated with treatment of the SCC on the right labial commissure, a field needed in reconstruction of the resected site. The aim of the patient’s treatment being tumour resection, restoration of function and a level of aesthetic restoration.
Methods: Careful consideration of reconstructive flap in this case was needed due to the compromised vascularity of the previously irradiated tissue. A modified Karapandzic flap along with a V-Y flap and placement of Integra intraorally was the treatment modality of choice, conserving nerves, enhancing blood supply as well as providing adequate adaptation and functional restoration.
Results: The selected flaps provided majority stable wound healing, restored oral competence, and preserved speech and oral intake. The patient recovered without major complications.
Conclusion: Oral commissure reconstruction in previously irradiated patients requires meticulous flap selection to optimise vascularity and function. A tailored approach is essential to achieving functional and aesthetic outcomes while satisfying the primary objective of complete tumour excision.
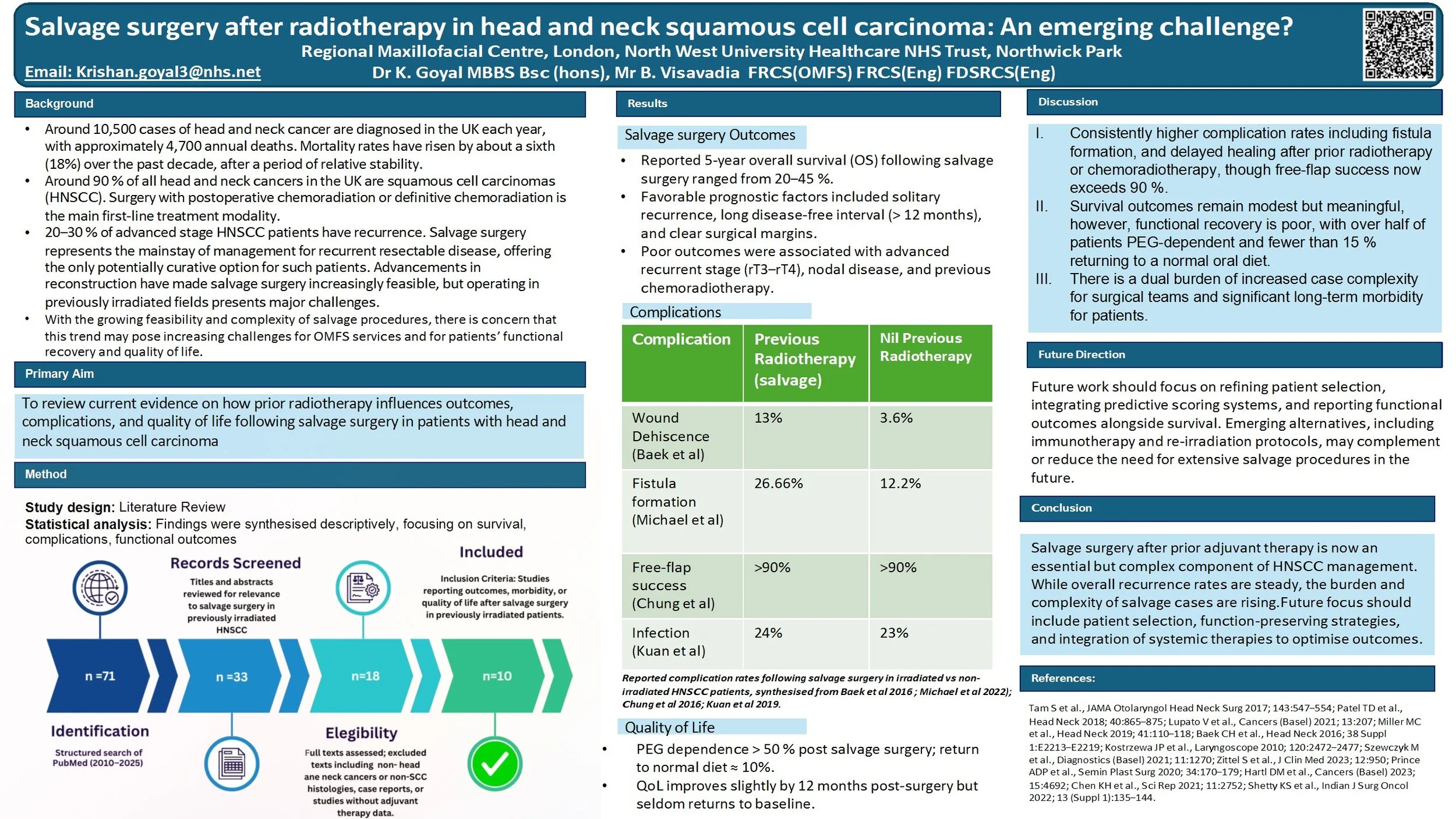
Salvage surgery after radiotherapy in head and neck squamous cell carcinoma: An emerging challenge?
Head and neck squamous cell carcinoma (HNSCC) is often treated with surgery followed by adjuvant radiotherapy or chemoradiotherapy in high-risk cases. While radiotherapy improves initial control, up to 20–30% of patients still develop recurrence. For many, salvage surgery is the only potentially curative option. Advances in microvascular reconstruction now make salvage more feasible, but operating in irradiated tissues carries higher risks and often leaves patients with significant functional difficulties.
Aim:
To review current evidence on how prior radiotherapy influences outcomes and complications of salvage surgery in HNSCC, and to consider the implications for both patients and clinical teams.
Findings:
Five-year overall survival after salvage typically ranges from 20–45%, with the best outcomes seen in solitary, late recurrences. Prognosis is worse with short disease-free intervals, nodal recurrence, or previous adjuvant treatment. Surgery in irradiated fields is associated with greater rates of wound breakdown, fistula and reconstructive failure, though flap survival exceeds 90% in experienced centres. Functionally, many patients remain gastrostomy-dependent and return to a normal diet is rare. Only about one-third of patients with recurrence are suitable candidates for salvage, but the overall number of operations is increasing due to rising cancer incidence, longer survivorship, and wider surgical feasibility.
Discussion:
For patients, salvage after radiotherapy offers a chance of cure but at the cost of higher morbidity and quality-of-life compromise. For clinical teams, these operations are complex, resource-intensive and require multidisciplinary planning.
Conclusion:
Salvage surgery in previously irradiated HNSCC provides hope for selected patients, but remains a demanding intervention with significant risks and functional consequences. Future strategies, including better patient selection, quality-of-life research, and novel systemic options such as immunotherapy, are needed to refine care.
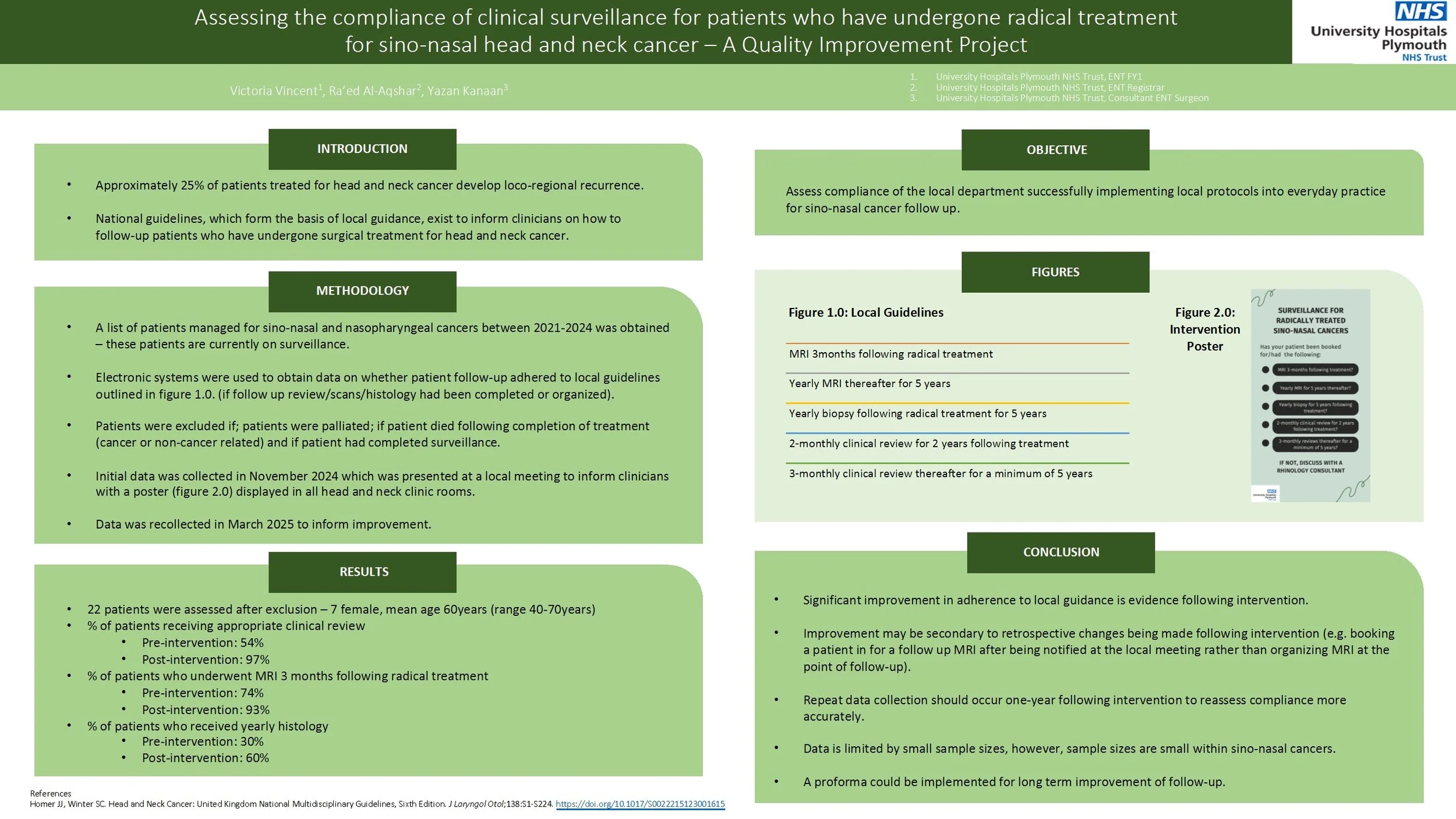
Assessing the compliance of clinical surveillance for patients who have undergone radical treatment for sino-nasal head and neck cancer – A Quality Improvement Project
Approximately 20% of patients treated for head and neck cancer develop loco-regional recurrence. National guidance, which forms the basis of local guidance, exists on how clinicians should follow-up patients following radical surgical treatment for head and neck cancer. The aim of the quality improvement project was to assess whether patients were being adequately followed up following radical management of sino-nasal cancers based upon local guidance.
Patients who underwent radical management of sino-nasal and nasopharyngeal cancers between 2020-2023 at one South West Trust were assessed using available online databases. Compliance to local guidance regarding follow up was assessed. Patients were excluded if they were palliated or if the patient died during treatment. Following the first cycle, the data was presented at the local departmental teaching and a poster reminding clinicians of the follow up criteria was implanted within clinic rooms. Data was then recollected 3 months later.
40 patients were coded as having new sino-nasal cancers. 22 patients were assessed after exclusion. There was improvement in the percentage of patients who had clinical review arranged within the correct timeframe from 54% to 97%. Percentage of patients who had an MRI arranged improved from 74% to 93%. Percentage of patients who had a biopsy arranged improved from 30% to 60%.
Although improvement was achieved within this audit, there were limitations within the study. Namely, the leading clinician was able to identify the patients who did not have correct follow up arranged from the initial audit cycle and arranged this himself, thus not demonstrating a direct link between intervention and change. There were also small sample sizes, however, this reflects the nature of the cohort of patients with sino-nasal cancers. Recommendations would include re-auditing at 1-2years to assess for continued improvement and to obtain more data.
Rim Mandibulectomy: Safe, even in the face of understaging?
Background:
Bony invasion in oral squamous cell carcinoma (SCC) is a poor prognostic factor. It is diagnosed preoperatively utilising staging scans and periosteal stripping. Tumours with invasion into the medulla typically require segmental mandibulectomy (SM) to ensure oncological clearance. A more conservative rim/marginal mandibulectomy (RM) may be performed in cases of close tumour proximity to bone or cortical erosion. However, this procedure may risk under-treatment if the preoperative assessments underestimate the extent of bone invasion.
This retrospective cohort study explores the suitability of RM as a conservative alternative to SM in select patients.
Methods:
Patients undergoing mandibulectomy for SCC at a UK OMFS centre between 2018-2023, with >24months follow-up, were identified. Primary outcomes are survival and recurrence, analysed using multivariate regression. Subgroup analysis will be performed on RM patients who subsequently demonstrate histological medullary involvement.
Results:
RM (n=26) and SM (n=30) patients met inclusion criteria. Regression modelling did not identify RM or SM procedures as a significant factor in patient outcomes (p>0.9). Histological medullary involvement was found in 6 RM patients (23%). Survival outcomes and recurrences in these patients were not significantly different to the wider RM group. Presence of bone margin clearance of 5mm was significantly related to survival outcomes.
Conclusions:
Findings continue to support RM as a safe surgical option, even with inherent risk of under-staging. However, preoperative diagnostic accuracy is key to reducing the risks. A further 10 patients have been identified for analysis and will also be presented in the dataset.
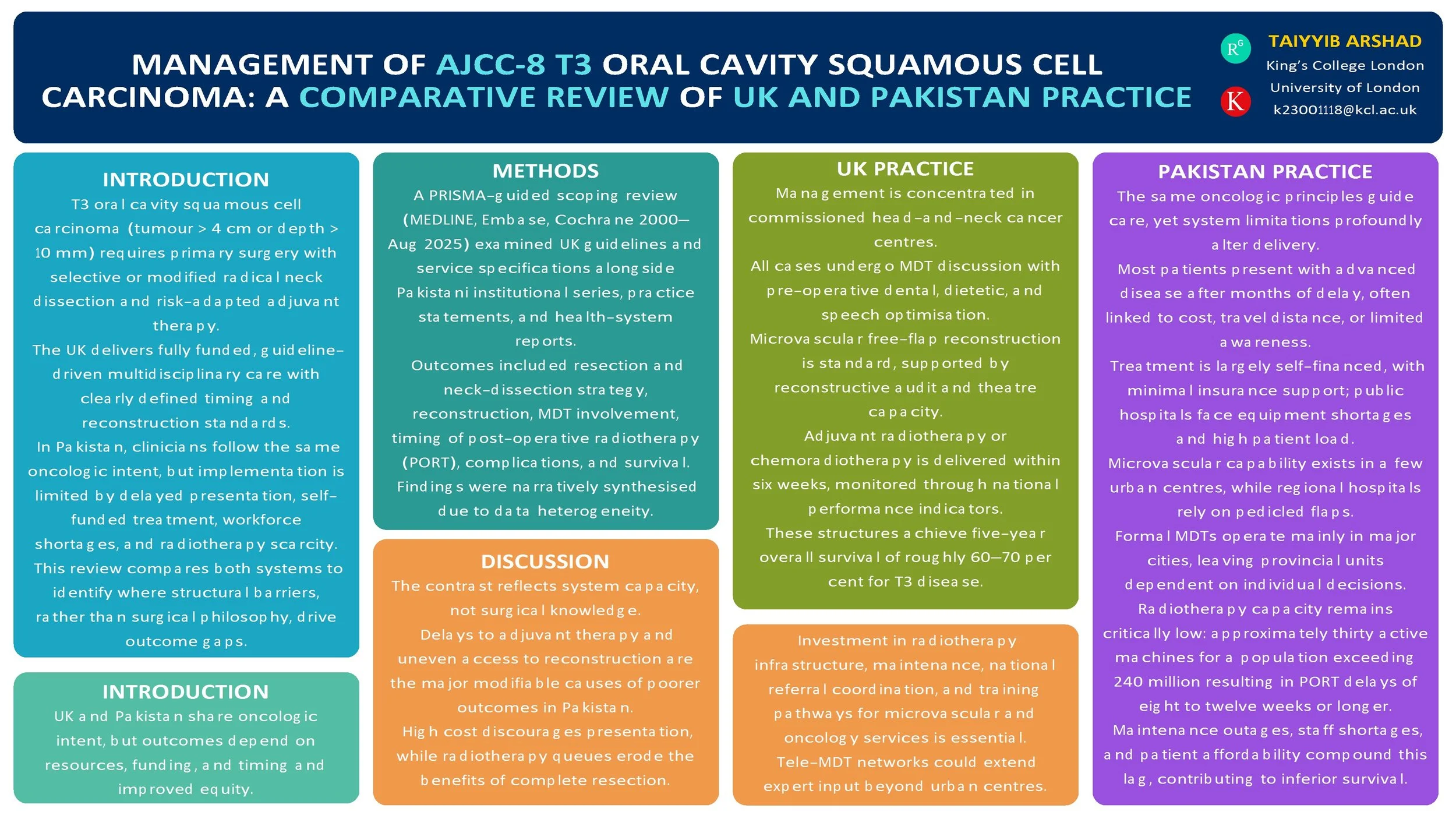
Management of AJCC-8 T3 Oral Cavity Squamous Cell Carcinoma: A Comparative Review of UK (NICE) and Pakistan Practices
Introduction
T3 oral cavity squamous cell carcinoma (OCSCC; AJCC-8: tumour > 4 cm or depth of invasion > 10 mm) is managed with primary surgery and risk-adapted adjuvant therapy. The UK delivers guideline-driven multidisciplinary care, while Pakistan applies the same oncologic principles within more heterogeneous resource settings. We compared published guidance and real-world practice to identify convergences, gaps, and opportunities for pathway improvement.
Method
PRISMA-guided scoping review (MEDLINE, Embase, Cochrane, and grey literature, 2000–Aug 2025). We included: (i) UK guidelines/standards for oral cavity cancer; (ii) Pakistan institutional series and practice statements for T3 OCSCC; (iii) health-system reports on multidisciplinary team (MDT) availability and radiotherapy capacity. Outcomes: resection and neck-dissection strategy, reconstruction modality, positive margins, time to post-operative radiotherapy (PORT), complications, recurrence, and survival. Data were charted narratively due to heterogeneity.
Results
UK sources consistently recommend upfront resection with appropriate ipsi/contralateral neck dissection, microvascular reconstruction when indicated, and adjuvant RT/CRT for adverse features, delivered through MDT pathways with staging, dental, and nutritional optimisation. Pakistan tertiary centres report adherence to core surgical principles with growing microvascular capability; regional flaps are used where resources are constrained. Across Pakistan reports, later stage at presentation is common; MDT access and radiotherapy capacity vary, contributing to PORT delays. Broader head-and-neck literature links delayed PORT (>6 weeks) with inferior outcomes. No head-to-head UK–Pakistan comparative cohort specific to T3 OCSCC outcomes was found.
Conclusion
Oncologic intent is aligned, but system-level factors—MDT coverage, reconstructive resources, and timely access to PORT—likely drive differences in delivered care and outcomes. Standardised, context-adapted pathways (routine MDT triage, clear neck algorithms, reconstruction choice matched to resources, and fast-tracked PORT) and a bi-national registry focused on T3 OCSCC are warranted to benchmark timing, treatment patterns, and outcomes.
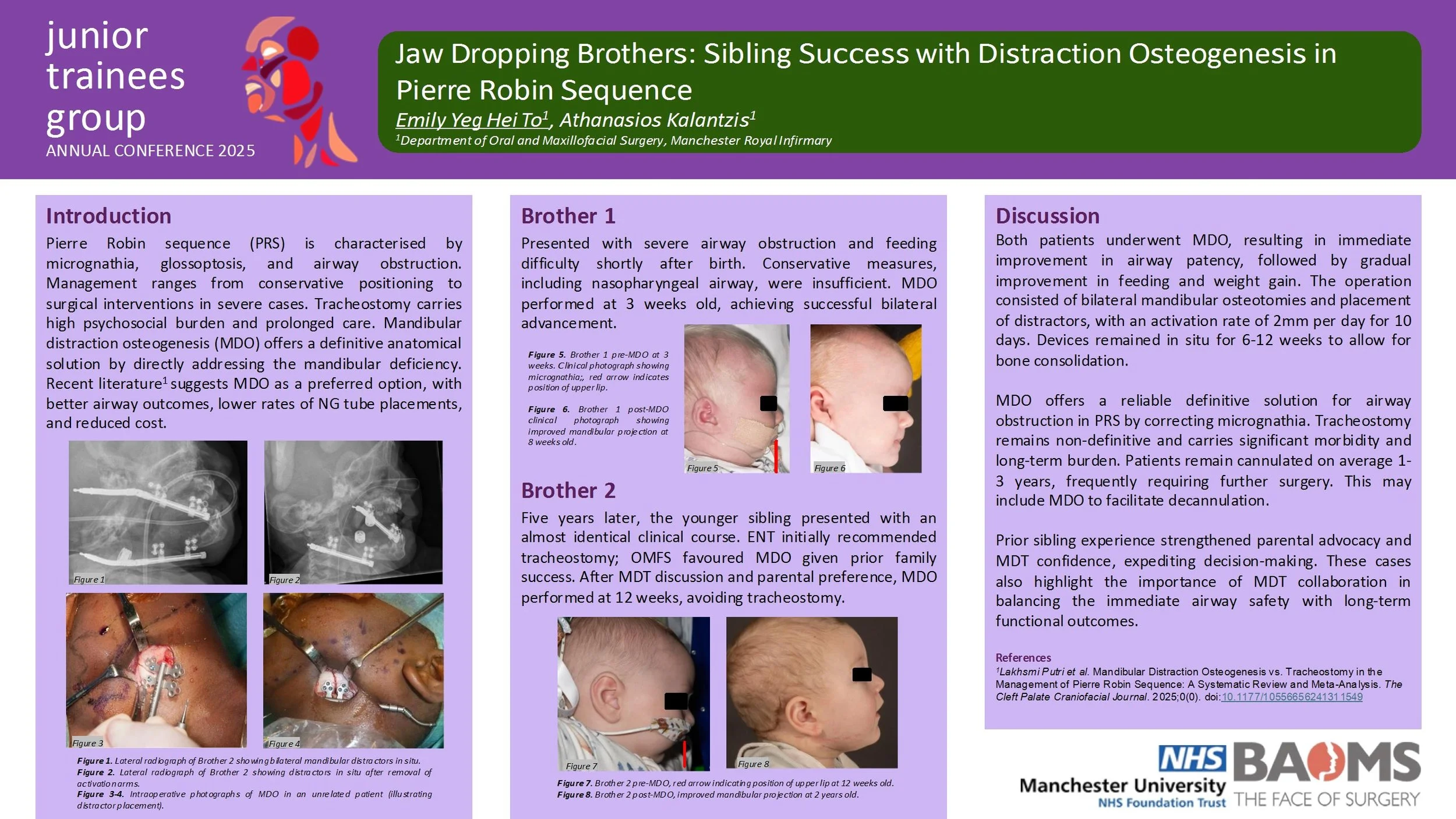
Jaw Dropping Brothers: Sibling Success with Distraction Osteogenesis in Pierre Robin Sequence
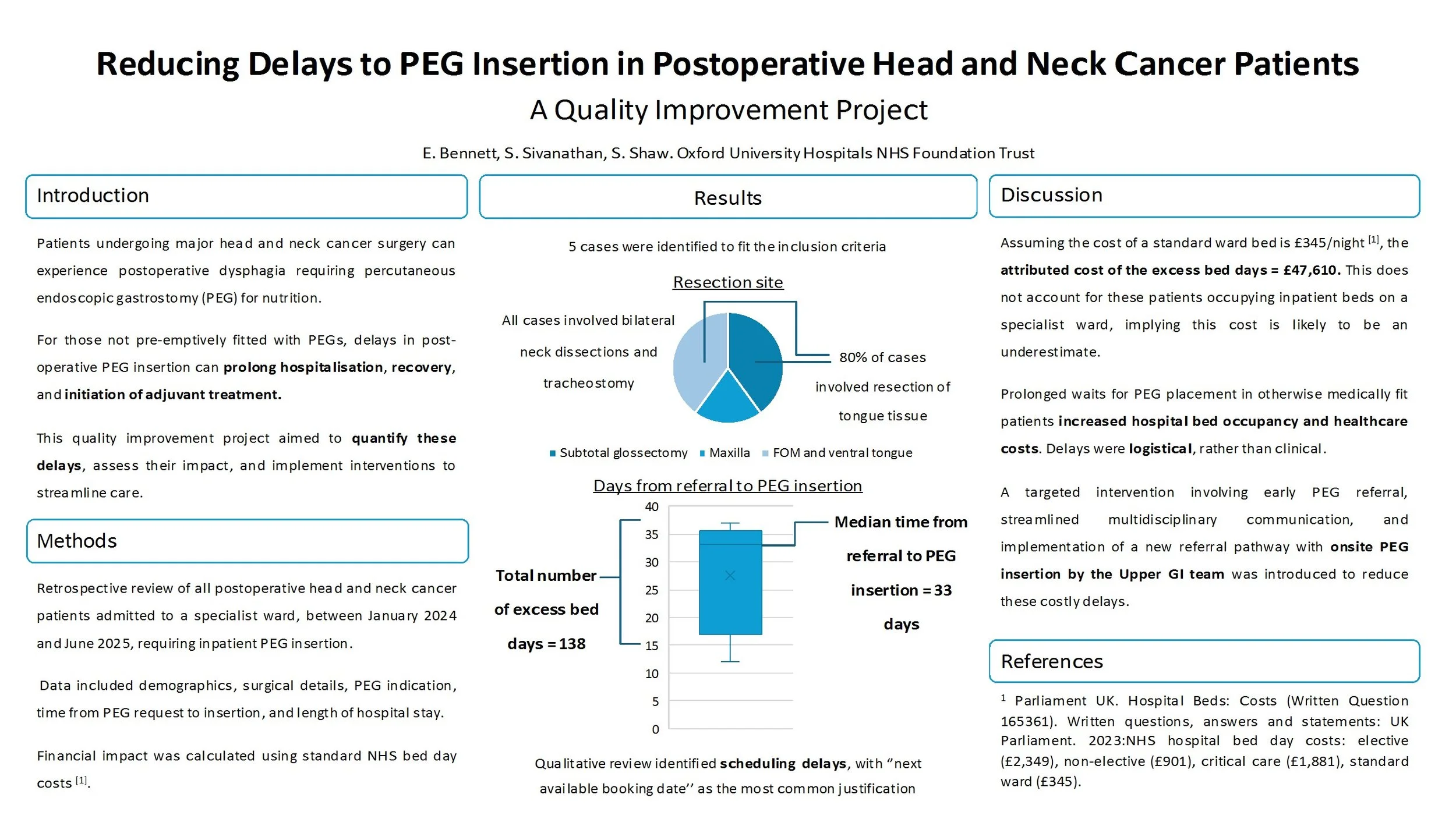
Reducing Delays to PEG Insertion in Postoperative Head and Neck Cancer Patients: A Quality Improvement Project
Introduction:
Patients undergoing major head and neck cancer surgery can experience postoperative dysphagia requiring percutaneous endoscopic gastrostomy (PEG) for nutrition. For those not pre-emptively fitted with PEGs, delays in post-operative PEG insertion can prolong hospitalisation, recovery, and initiation of adjuvant treatment. This quality improvement project aimed to quantify these delays, assess their impact, and implement interventions to streamline care.
Methods:
A retrospective review of all postoperative head and neck cancer patients admitted to a specialist ward, in a single centre, between January 2024, and June 2025, requiring inpatient PEG insertion was done. Data included demographics, surgical details, PEG indication, time from PEG request to insertion, and length of hospital stay. Financial impact was calculated using standard NHS bed day costs.
Results:
Five patients met inclusion criteria. All had extensive surgical procedures including bilateral neck dissections and tracheostomy. Median time from PEG request to insertion was 33 days (range: 12–37 days). Qualitative review revealed scheduling delays, with “next available booking date” as the most common justification. These delays accounted for 138 excess bed days, equating to an estimated cost of £47,610.
Discussion:
Prolonged waits for PEG placement in otherwise medically fit patients increased hospital bed occupancy and healthcare costs. Delays were logistical, rather than clinical. A targeted intervention involving early PEG referral, streamlined multidisciplinary communication, and onsite PEG insertion by the Upper GI team was introduced.
Conclusion:
Delayed PEG insertion in postoperative head and neck cancer patients leads to avoidable hospitalisation, financial burden, and may delay adjuvant treatment. Reasons for delay were specific to logistical factors within the unit. Results were presented and led to the implementation of an onsite referral pathway and improved interdepartmental coordination in order to offer a sustainable solution.
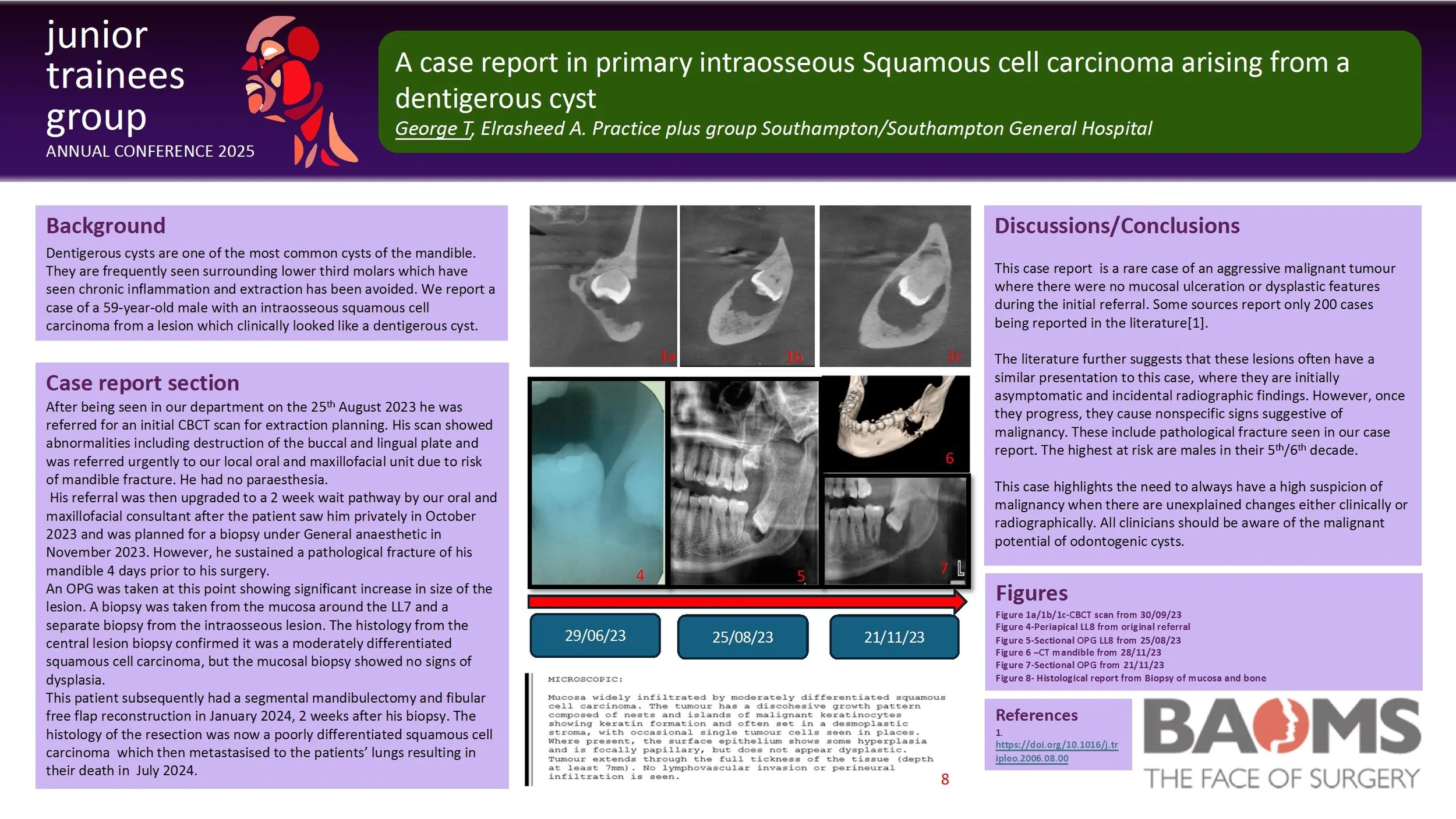
A case report in primary intraosseous Squamous cell carcinoma arising from a dentigerous cyst
Dentigerous cysts are one of the most common cysts of the mandible. They are frequently seen surrounding lower third molars which have seen chronic inflammation and extraction has been avoided. We report a case of a 59-year-old male with an intraosseous squamous cell carcinoma from a lesion which clinically looked like a dentigerous cyst.
He was referred by his General Dental Practitioner to our oral surgery department for extraction of a symptomatic LL8 in June 2023. His initial CBCT scan showed abnormalities including destruction of the buccal and lingual plate and was referred urgently to our local oral and maxillofacial unit due to risk of mandible fracture. He had no paraesthesia.
His referral was then upgraded to a 2 week wait pathway by our oral and maxillofacial consultant after the patient saw him privately in October 2023 and was planned for a biopsy under General anaesthetic in November 2023. However, he sustained a pathological fracture of his mandible 4 days prior to his surgery. An OPG was taken at this point showing significant increase in size of the lesion.
A biopsy was taken from the mucosa around the LL7 and a separate biopsy from the intraosseous lesion. The histology from the central lesion biopsy confirmed it was a moderately differentiated squamous cell carcinoma, but the mucosal biopsy showed no signs of dysplasia.
This patient subsequently had a segmental mandibulectomy and fibular free flap reconstruction in January 2024, 2 weeks after his biopsy. The histology of the resection was now a poorly differentiated squamous cell carcinoma.
This highlights an unusual case of an aggressive malignant tumour where there was no mucosal ulceration or dysplastic features. It emphasises the importance of reassessing the patient’s clinical picture and to be aware of the potential malignant change of odontogenic cysts.
Reducing Delays to PEG Insertion in Postoperative Head and Neck Cancer Patients - A Quality Improvement Project
Reducing Delays to PEG Insertion in Postoperative Head and Neck Cancer Patients: A Quality Improvement Project
Introduction:
Patients undergoing major head and neck cancer surgery can experience postoperative dysphagia requiring percutaneous endoscopic gastrostomy (PEG) for nutrition. For those not pre-emptively fitted with PEGs, delays in post-operative PEG insertion can prolong hospitalisation, recovery, and initiation of adjuvant treatment. This quality improvement project aimed to quantify these delays, assess their impact, and implement interventions to streamline care.
Methods:
A retrospective review of all postoperative head and neck cancer patients admitted to a specialist ward, in a single centre, between January 2024, and June 2025, requiring inpatient PEG insertion was done. Data included demographics, surgical details, PEG indication, time from PEG request to insertion, and length of hospital stay. Financial impact was calculated using standard NHS bed day costs.
Results:
Five patients met inclusion criteria. All had extensive surgical procedures including bilateral neck dissections and tracheostomy. Median time from PEG request to insertion was 33 days (range: 12–37 days). Qualitative review revealed scheduling delays, with “next available booking date” as the most common justification. These delays accounted for 138 excess bed days, equating to an estimated cost of £47,610.
Discussion:
Prolonged waits for PEG placement in otherwise medically fit patients increased hospital bed occupancy and healthcare costs. Delays were logistical, rather than clinical. A targeted intervention involving early PEG referral, streamlined multidisciplinary communication, and onsite PEG insertion by the Upper GI team was introduced.
Conclusion:
Delayed PEG insertion in postoperative head and neck cancer patients leads to avoidable hospitalisation, financial burden, and may delay adjuvant treatment. Reasons for delay were specific to logistical factors within the unit. Results were presented and led to the implementation of an onsite referral pathway and improved interdepartmental coordination in order to offer a sustainable solution.
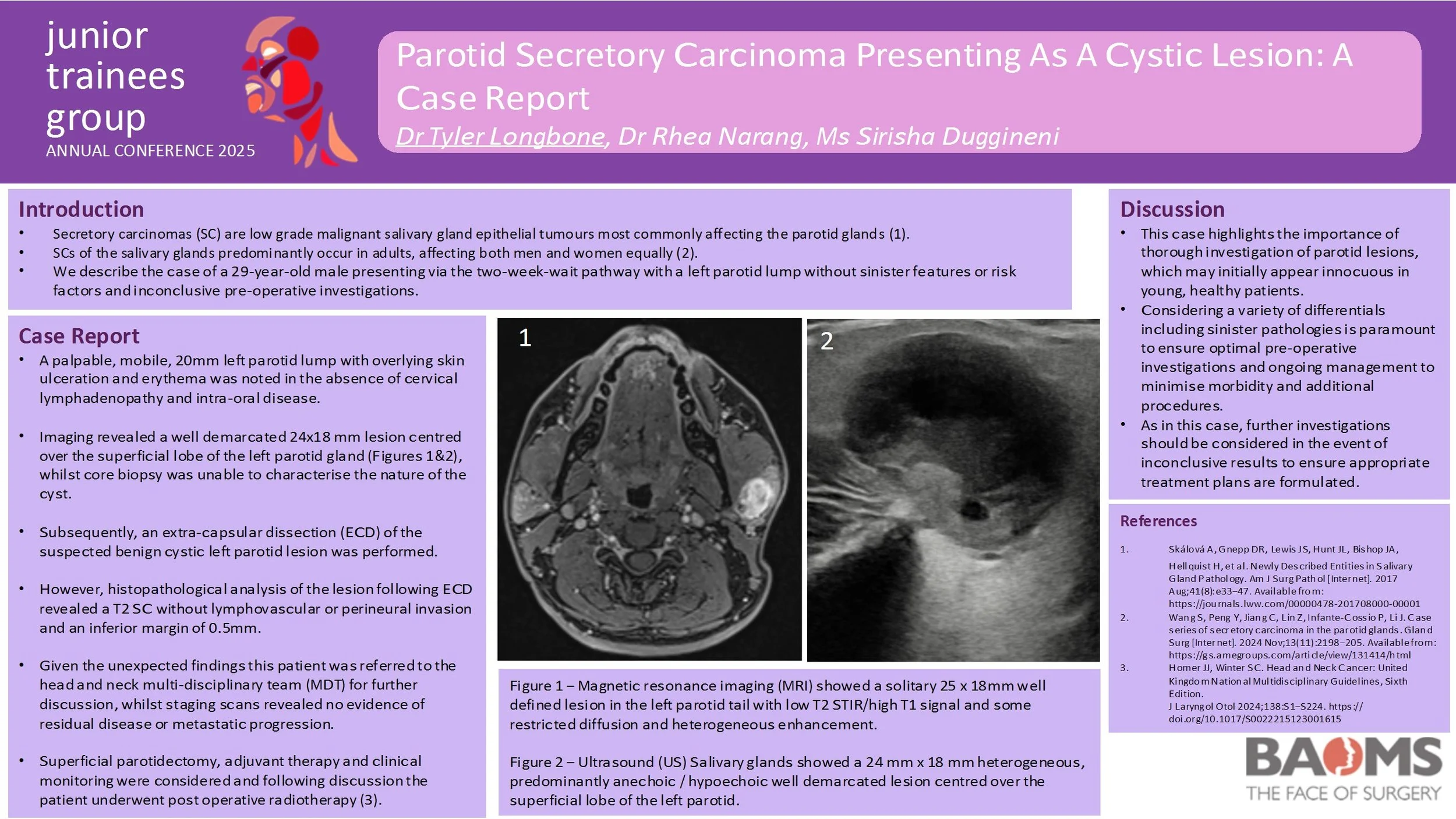
Parotid Secretory Carcinoma Presenting As A Cystic Lesion: A Case Report
Introduction:
Secretory carcinomas are low grade malignant tumours which most commonly affect the parotid glands. This report describes the case of a 29-year-old male presenting via the two-week-wait pathway with a left parotid lump without sinister features, risk factors and inconclusive pre-operative investigations. The option to pursue further lesion characterisation was discussed, however the patient elected to undergo treatment for the likely benign cystic lesion which was unexpectedly found to be a secretory carcinoma.
Case Report:
On review a palpable, mobile, 20mm left parotid lump with overlying skin ulceration and erythema was noted in the absence of cervical lymphadenopathy and intra-oral disease. Pre-operative imaging revealed a well demarcated 24x18 mm lesion centred over the superficial lobe of the left parotid gland, whilst core biopsy was unable to characterise the nature of the cyst. However, histopathological analysis of the left parotid lesion following extra-capsular dissection revealed a T2 secretory carcinoma without lymphovascular or perineural invasion and an inferior margin of 0.5mm. Subsequent staging scans did not demonstrate evidence of residual disease or metastatic progression.
This patient initially underwent extra-capsular dissection of the suspected benign cystic left parotid lesion. Given the unexpected histopathological findings this patient was referred to the head and neck multi-disciplinary team (MDT) for further discussion. Superficial parotidectomy, adjuvant therapy and clinical monitoring were considered and following discussion the patient underwent post operative radiotherapy.
Discussion:
This case highlights the importance of thorough investigation of parotid lesions, which may initially appear innocuous in young, healthy patients. Undoubtedly, considering a variety of differentials including sinister pathologies is paramount to ensure optimal pre-operative investigations and ongoing management to minimise morbidity and additional procedures.
The use of dermal matrices in the reconstruction of defects following the resection of oral potentially malignant disorders: a scoping review
Introduction:
Dysplasia and oral potentially malignant disorders (OPMDs) of the oral cavity often require surgical resection to prevent malignant transformation. These lesions are frequently left to heal by secondary intention, exposing patients to discomfort and an increased risk of post-operative infection. Dermal matrices offer a promising reconstructive alternative, providing biocompatibility and favourable healing outcomes. However, their clinical use in this specific context has not yet been comprehensively reviewed. This scoping review aims to systematically map and critically appraise the current evidence on the use of dermal matrices in reconstructive surgery following resection of dysplastic lesions and OPMDs of the oral cavity, and to identify current evidence, innovation, and gaps in knowledge.
Methods:
A scoping review was conducted following the PRISMA-ScR guidelines. The electronic databases PubMed, Scopus and Medline were searched without date restrictions. Grey literature was also explored via Google Scholar. Two reviewers independently screened the articles, with discrepancies resolved by a third reviewer. Data were extracted on factors such as study design, type of dermal matrix used, surgical outcomes and disease recurrence.
Results:
From an initial yield of 6229 titles, 25 studies met the inclusion criteria. These involved various dermal matrix types, including acellular human dermal matrices and bovine-derived collagen scaffolds. Most studies reported satisfactory integration and minimal complications. However, heterogeneity in study design, outcome measures, and follow-up limited direct comparisons. Few studies specifically addressed long-term recurrence or malignant transformation post-reconstruction.
Conclusion:
Dermal matrices may represent a viable and increasingly utilised option for reconstructing defects following the resection of dysplasia and OPMDs of the oral cavity. While this review highlights early successes, it also underscores key limitations in the existing literature and calls for targeted research to validate dermal matrices as a standard reconstructive strategy in oral oncology.
Connecting Patients and Providers: A Quality Improvement Initiative in Head and Neck Cancer Care
Introduction
Patients with head and neck cancer are often treated across multiple hospitals, leading to confusion about appointments, treatment stages, and who to contact. This quality improvement project aimed to improve communication by introducing a clear, unified leaflet outlining the full treatment pathway. The project involved trusts in London and Essex, with UCLH as the central site for surgery.
Methodology
The leaflet was co-developed with input from consultants, clinical nurse specialists, and admin staff from UCLH, Queen’s, and the Royal London Hospital. It explained each step of the patient journey from diagnosis to surgery and follow-up and was translated into several languages to reflect local populations. Patients received the leaflet at pre-assessment and were asked to complete a six-question survey before and an eight-question survey after reading it.
Results
Survey results were on a scale from 1-5 and displayed marked improvements. Familiarity with the care process rose from an average of 2.3 to 4.2. Confidence in navigating appointments and services improved from 2.1 to 4.1. Understanding of treatment stages increased from 2.4 to 4.3. Clarity around locations and contact points also improved. More than 90% of patients rated the leaflet as clear and helpful. At £50 per 1000 copies, the leaflet was low-cost. Challenges included translation funding, legal permissions, and coordination between sites, though these were manageable.
Conclusion
This QIP offers a simple, scalable solution to a common communication gap in cancer care. By creating a multilingual, patient-friendly resource in both print and digital formats, the project has improved patient understanding and pathway navigation. Future work will assess long-term effects on patient satisfaction and whether the approach can be expanded to other specialties.
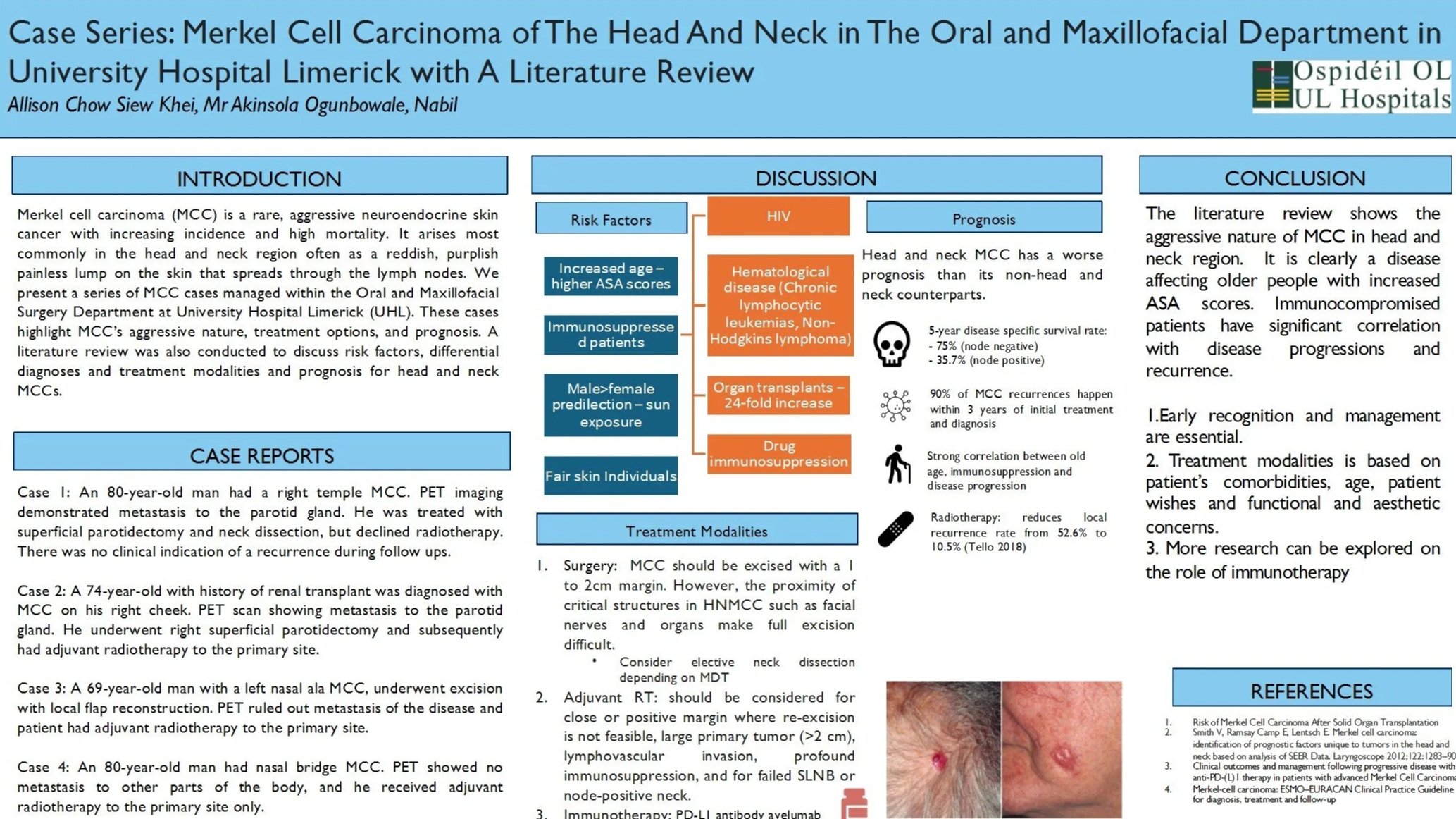
Case Series: Merkel Cell Carcinoma of The Head And Neck in The Oral and Maxillofacial Department in University Hospital Limerick with A Literature Review
Introduction
Merkel cell carcinoma (MCC) is a rare, aggressive neuroendocrine skin cancer with increasing incidence and high mortality. Early recognition and management are essential. We present a series of MCC cases managed within the Oral and Maxillofacial Surgery Department at University Hospitals Limerick (UHL). These cases highlight MMC’s aggressive nature, treatment options, and prognosis.
Case Reports
Case 1: A 74-year-old man diagnosed with right cheek MCC with metastatic to the parotid gland. He underwent right superficial parotidectomy followed by chemo-radiotherapy.
Case 2: An 80-year-old man had a right temple MCC. PET imaging demonstrated metastasis to parotid. He was treated with superficial parotidectomy and neck dissection, but declined radiotherapy.
Case 3: A 69-year-old man with an left nasal ala MCC, underwent excision with local flap reconstruction. PET ruled out metastasis of the disease and he received adjuvant radiotherapy to the primary site.
Case 4: An 80-year-old man had an nasal bridge MCC. PET showed no metastasis, and he received adjuvant radiotherapy to the primary site only.
Discussion
MCC is an uncommon but highly aggressive cutaneous malignancy, most often arising on the head and neck. Risk factors include immunosuppression, with solid organ recipients carrying a 24-fold increased risk. Surgery is the mainstay of treatment, usually followed by adjuvant radiotherapy. Chemotherapy is reserved for advanced disease, while immunotherapy is an emerging and promising option.
Conclusion
MCC is rarely suspected clinically but is rapidly becoming more common. Imaging, particularly PET, should be considered where clinically indicated. Management typically involves surgery with adjuvant radiotherapy; chemotherapy and immunotherapy may be considered in metastatic or recurrent disease. Further studies surrounding knowledge of disease progression and management, should be carried out