JTG 2025 Poster Gallery
Implications of High BMI in the Investigation & Management of Cervico-Facial Infections
Introduction
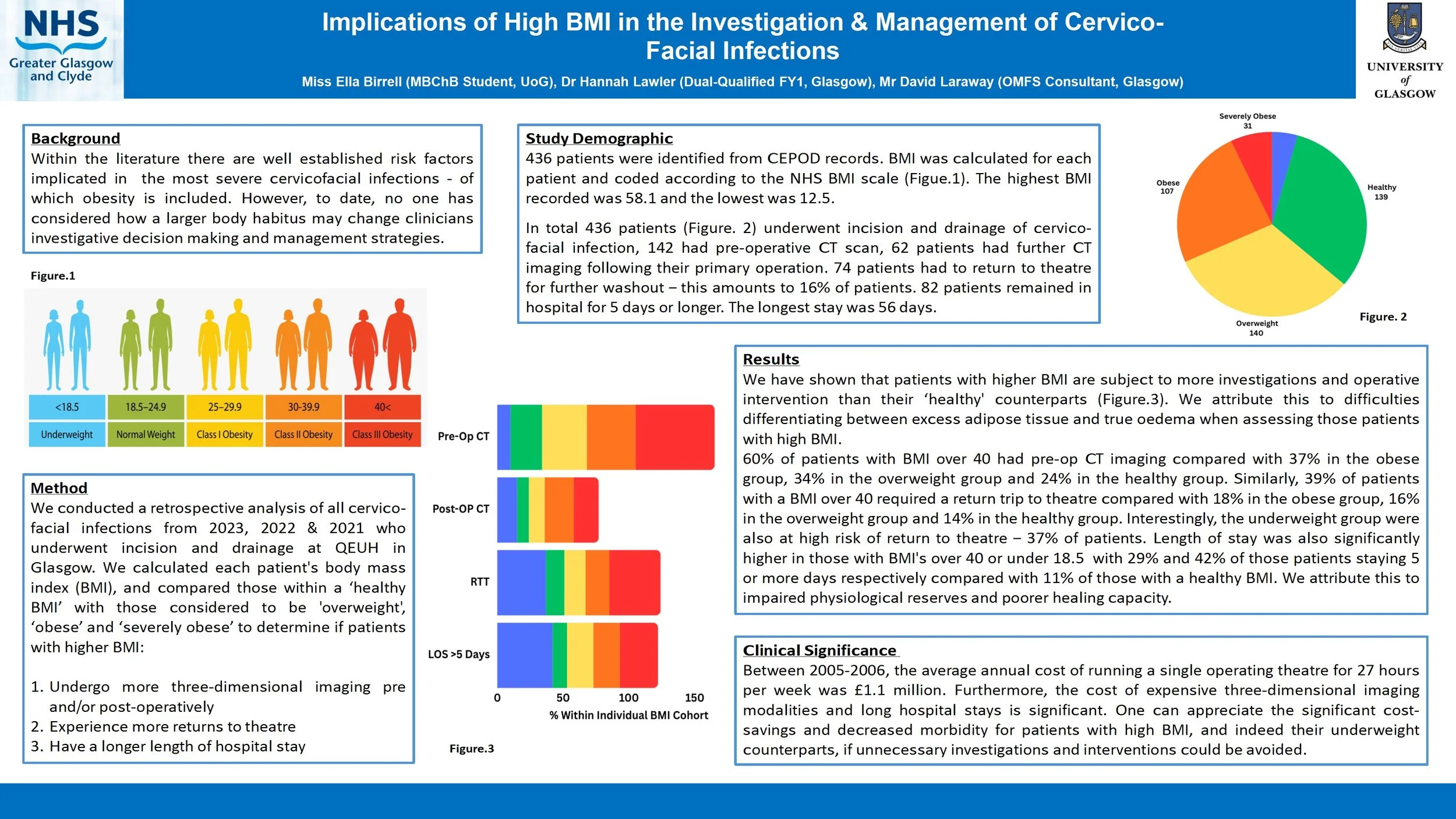
Within the literature there are well established risk factors implicated in the most severe cervicofacial infections - of which obesity is included. However, to date, no one has considered how a larger body habitus may change clinicians investigative decision making and management strategies.
Method
We conducted a retrospective analysis of all cervico-facial infections over the last 6 years who underwent incision and drainage at QEUH in Glasgow. We calculated each patient's body mass index (BMI), and compared those within a ‘healthy BMI’ with those considered to be ‘obese’ and ‘morbidly obese’ to determine if patients with higher BMI:
Undergo more three-dimensional imaging pre/post-operatively
Experience more returns to theatre
Have a longer length of hospital stay
Are more likely to require a tracheostomy or intensive care stay
Results
We have shown that patients with higher BMI are subject to more investigations and operative intervention than their ‘healthy BMI’ counterparts. We attribute this to difficulties differentiating between excess adipose tissue and true oedema when assessing those patients with high BMI.
Conclusion
Between 2005-2006, the average annual cost of running a single operating theatre for 27 hours per week was £1.1 million. Furthermore, the cost of expensive three-dimensional imaging modalities and long hospital stays is significant. One can appreciate the significant cost-savings and decreased morbidity for patients with high BMI if unnecessary investigations and interventions could be avoided.
To Orbit or Not to Orbit: Using Pre-Operative Orbital Findings to Predict the Need for Orbital Exploration in Zygomaticomaxillary Complex (ZMC) Fractures
Introduction:
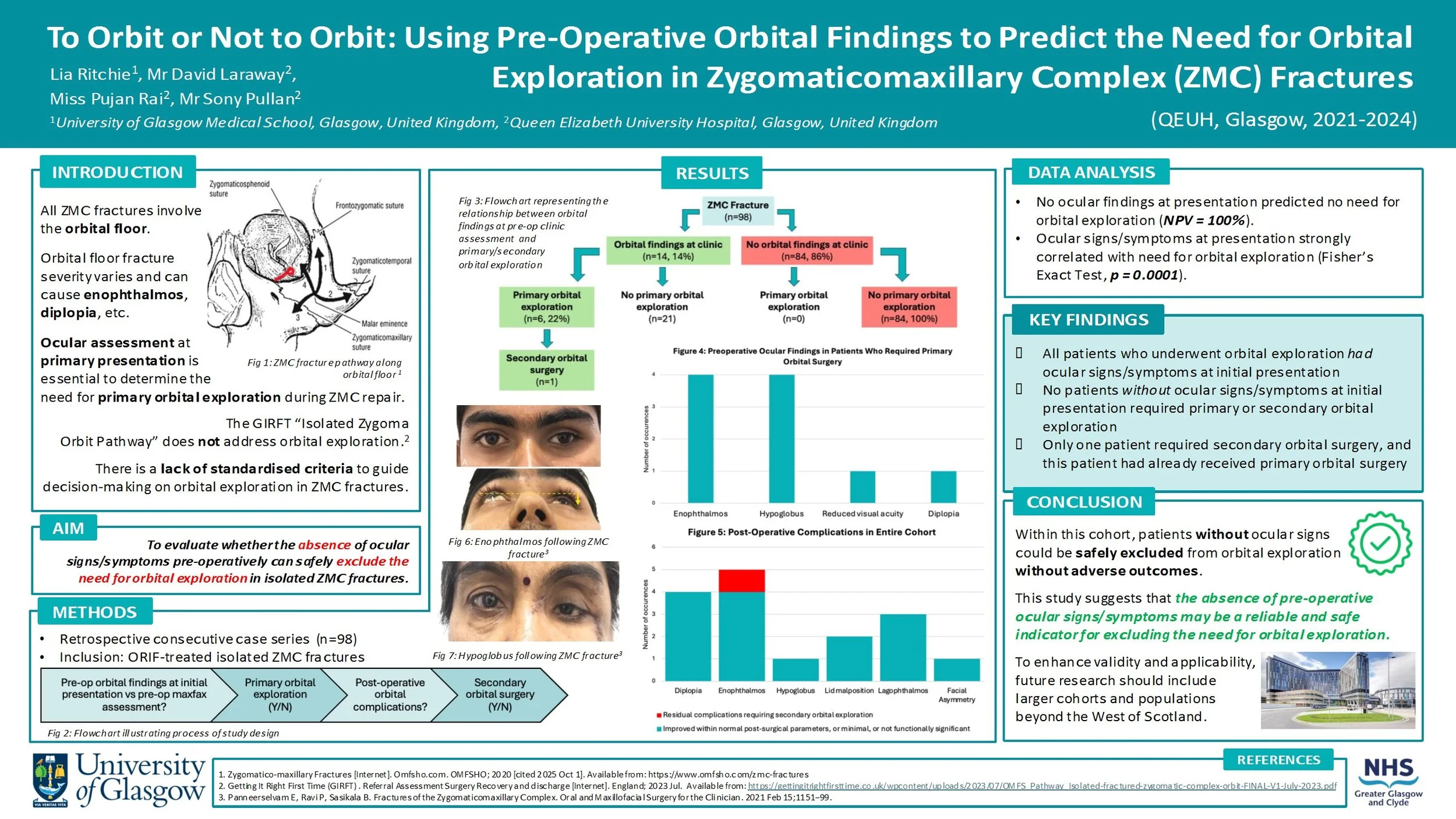
All ZMC fractures involve orbital fractures, with orbital floor fracture severity varying depending on the mechanism and energy of injury. Disruption of the orbital floor changes the orbital volume, increasing the risk of ocular signs/symptoms (e.g. enophthalmos, diplopia). This must be assessed at primary presentation to decide if primary orbital surgery should be performed alongside ZMC repair.
There is currently no standardised set of criteria to guide the decision-making process for orbital exploration in ZMC fractures. This study will evaluate whether the absence of ocular signs/symptoms pre-operatively can safely exclude the need for orbital exploration.
Method:
Data was retrospectively collected from a consecutive series of 98 patients who had ZMC fractures requiring ORIF intervention at the QEUH between 2021-2024. The presence/absence of ocular signs/symptoms at initial assessment was recorded. The cohort was then assessed to determine which patients underwent primary orbital exploration. Post-operative outcomes were reviewed, including whether any patients subsequently required secondary orbital surgery.
Results:
27 patients (28%) presented with ocular signs/symptoms, 6 of them underwent primary orbital surgery. Among the 71 patients (72%) who had no ocular findings at initial presentation, none required orbital surgery. Only 1 patient in the cohort required secondary orbital surgery, and this patient had also undergone primary orbital surgery.
Conclusion:
The absence of pre-operative ocular signs/symptoms may be a reliable indicator for excluding the need for orbital exploration. No patients who did not receive primary orbital exploration needed secondary orbital exploration, proving there were no late ocular complications from this approach.
Orbital Roof Reconstruction Utilizing Inverted Orbital Floor Plates - A Case-Based Technical Note
Background: Orbital roof fractures are rare [1] but significant injuries resulting from high-energy trauma, often alongside complex maxillofacial injuries [2,3]. Surgical repair is indicated for displaced fractures with neurological or ophthalmic compromise [4]. Traditional reconstruction with titanium mesh presents challenges such as insufficient rigidity, sharp edges, implant extrusion risk, and difficulty of removal if infected. As such, we propose using pre-shaped orbital floor plates, inverted for orbital roof reconstruction, offering improved structural support and a more ergonomic surgical experience.
Methods: Retrospective case series (n=4) of patients undergoing surgical repair for orbital roof fractures. A bicoronal and pericranial flap was raised, followed by hemifrontal craniotomy. Orbital roof defects were visualised, dural tears repaired, and reconstruction performed using inverted orbital floor plates secured with screws. A pericranial flap covered the repair, and the bone flap was re-fixed with low-profile plating. Postoperative outcomes were assessed.
Results: All cases achieved correct orbital roof alignment and restoration of orbital volume. No implant-related infections were found. Progressive recovery or complete resolution of ocular symptoms was observed, even in severe trauma patients.
Discussion: This case series demonstrates the feasibility, safety, and structural adequacy of using inverted orbital floor plates for orbital roof reconstruction. This alternative offers greater rigidity, easier handling, anatomical contour matching and immediate availability in trauma settings, with good outcomes even in severe trauma. Study limitations include small sample size due to the rarity of the fracture, heterogeneous trauma profiles, and limited long-term follow-up. Therefore, further studies are needed to confirm long-term outcomes.
An extensive Odontogenic Keratocyst in the left maxilla: a case report
Odontogenic Keratocysts (OKC) are benign cystic lesions that are known to be locally aggressive and have a high recurrence rate. Here we describe a case of a particularly extensive OKC.
A 28 year-old female presented to the Oral and Maxillofacial department with a 2-month history of facial swelling and pain. On examination, there was a left mid-facial swelling which was extremely tender on palpation, with intra-oral buccal expansion. Medically, she had depression and was a non-smoker. An OPG and CT neck with contrast was carried out; this revealed a substantial lesion, filling the left maxillary sinus, in association with a superiorly impacted UL8 tooth located just below the orbital apex. The lesion had cystic characteristics, measuring 6.6cm vertically, and 5.8 x 3.8cm in a transverse dimension. The lesion was shown to project medially into the nasal cavity, resulting in septal deviation to the right. Superiorly, there was associated convex bulging of the orbital floor.
Subsequently, antibiotics were prescribed; enucleation of the cyst and extraction of UL8 was carried out. The pathology result was in favour of Odontogenic Keratocyst. Infection reoccurred 1 month later which led to a washout of the cystic cavity, placement of a drain, extraction of a resorbed UL6 and additional antibiotic therapy. Gabapentin was then commenced due to associated neuropathic pain. 3 months following initial surgery, further enucleation of a 1x1cm residual cyst was carried out. 6 months later, a repeat CT scan revealed mildly progressive bony infill in line with ongoing healing and no evidence of recurrence.
This case highlights the aggressive nature of the OKC despite their slow growth. The presence of such an expansile lesion in the maxillary sinus with an associated ectopic tooth just below the orbital apex is rare. Close follow-up to detect recurrence is important.