JTG 2025 Poster Gallery
Large language models in OMFS triage
Introduction:
Accurate triage of OMFS referrals is essential for appropriate care. However, increasing volume and often poor referral quality place strain on consultant time. Large language models (LLMs), such as GPT-3.5 and GPT-4, are emerging as potential decision-support tools. This project combined a scoping review and pilot study to evaluate the effectiveness of LLMs in OMFS referral triage compared to clinicians.
Method:
A scoping review was conducted using the PRISMA-ScR framework to identify literature on LLMs in triage, diagnosis, and referral optimisation. Findings informed a pilot study. Fifty synthetic referrals were constructed using anonymised real-patient case summaries. Original referrals lacked sufficient detail, so synthetic versions were designed to reflect plausible clinical scenarios with adequate information for assessment. Each referral was input into GPT-3.5 and GPT-4 using a standardised prompt requesting: (1) suggested investigations, (2) likely diagnosis, and (3) initial management. Outputs were compared to actual clinical decisions for those cases.
Results:
The review found limited but growing evidence for LLMs in referral triage, with sparse coverage in surgical specialties. In the pilot, GPT-4 showed better clinical alignment than GPT-3.5 across all domains. Both models produced more appropriate suggestions with structured information, but struggled with vague inputs, mirroring challenges in human triage.
Conclusion:
LLMs, particularly GPT-4, show promise as triage adjuncts in OMFS. While not a replacement for clinician judgement, they may help streamline decision-making when referral detail is sufficient. Further validation is needed before clinical implementation.
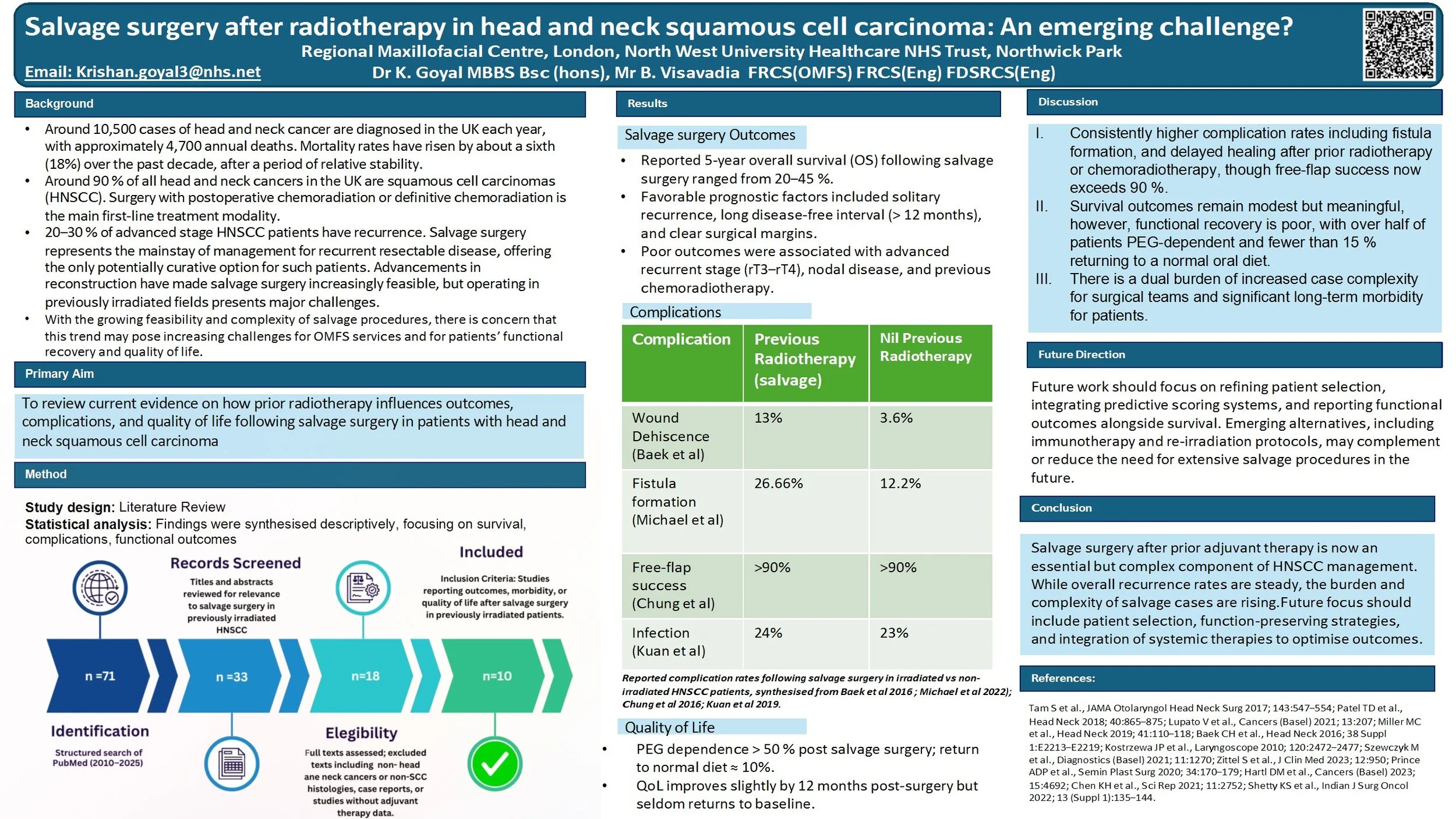
Salvage surgery after radiotherapy in head and neck squamous cell carcinoma: An emerging challenge?
Head and neck squamous cell carcinoma (HNSCC) is often treated with surgery followed by adjuvant radiotherapy or chemoradiotherapy in high-risk cases. While radiotherapy improves initial control, up to 20–30% of patients still develop recurrence. For many, salvage surgery is the only potentially curative option. Advances in microvascular reconstruction now make salvage more feasible, but operating in irradiated tissues carries higher risks and often leaves patients with significant functional difficulties.
Aim:
To review current evidence on how prior radiotherapy influences outcomes and complications of salvage surgery in HNSCC, and to consider the implications for both patients and clinical teams.
Findings:
Five-year overall survival after salvage typically ranges from 20–45%, with the best outcomes seen in solitary, late recurrences. Prognosis is worse with short disease-free intervals, nodal recurrence, or previous adjuvant treatment. Surgery in irradiated fields is associated with greater rates of wound breakdown, fistula and reconstructive failure, though flap survival exceeds 90% in experienced centres. Functionally, many patients remain gastrostomy-dependent and return to a normal diet is rare. Only about one-third of patients with recurrence are suitable candidates for salvage, but the overall number of operations is increasing due to rising cancer incidence, longer survivorship, and wider surgical feasibility.
Discussion:
For patients, salvage after radiotherapy offers a chance of cure but at the cost of higher morbidity and quality-of-life compromise. For clinical teams, these operations are complex, resource-intensive and require multidisciplinary planning.
Conclusion:
Salvage surgery in previously irradiated HNSCC provides hope for selected patients, but remains a demanding intervention with significant risks and functional consequences. Future strategies, including better patient selection, quality-of-life research, and novel systemic options such as immunotherapy, are needed to refine care.
Rim Mandibulectomy: Safe, even in the face of understaging?
Background:
Bony invasion in oral squamous cell carcinoma (SCC) is a poor prognostic factor. It is diagnosed preoperatively utilising staging scans and periosteal stripping. Tumours with invasion into the medulla typically require segmental mandibulectomy (SM) to ensure oncological clearance. A more conservative rim/marginal mandibulectomy (RM) may be performed in cases of close tumour proximity to bone or cortical erosion. However, this procedure may risk under-treatment if the preoperative assessments underestimate the extent of bone invasion.
This retrospective cohort study explores the suitability of RM as a conservative alternative to SM in select patients.
Methods:
Patients undergoing mandibulectomy for SCC at a UK OMFS centre between 2018-2023, with >24months follow-up, were identified. Primary outcomes are survival and recurrence, analysed using multivariate regression. Subgroup analysis will be performed on RM patients who subsequently demonstrate histological medullary involvement.
Results:
RM (n=26) and SM (n=30) patients met inclusion criteria. Regression modelling did not identify RM or SM procedures as a significant factor in patient outcomes (p>0.9). Histological medullary involvement was found in 6 RM patients (23%). Survival outcomes and recurrences in these patients were not significantly different to the wider RM group. Presence of bone margin clearance of 5mm was significantly related to survival outcomes.
Conclusions:
Findings continue to support RM as a safe surgical option, even with inherent risk of under-staging. However, preoperative diagnostic accuracy is key to reducing the risks. A further 10 patients have been identified for analysis and will also be presented in the dataset.
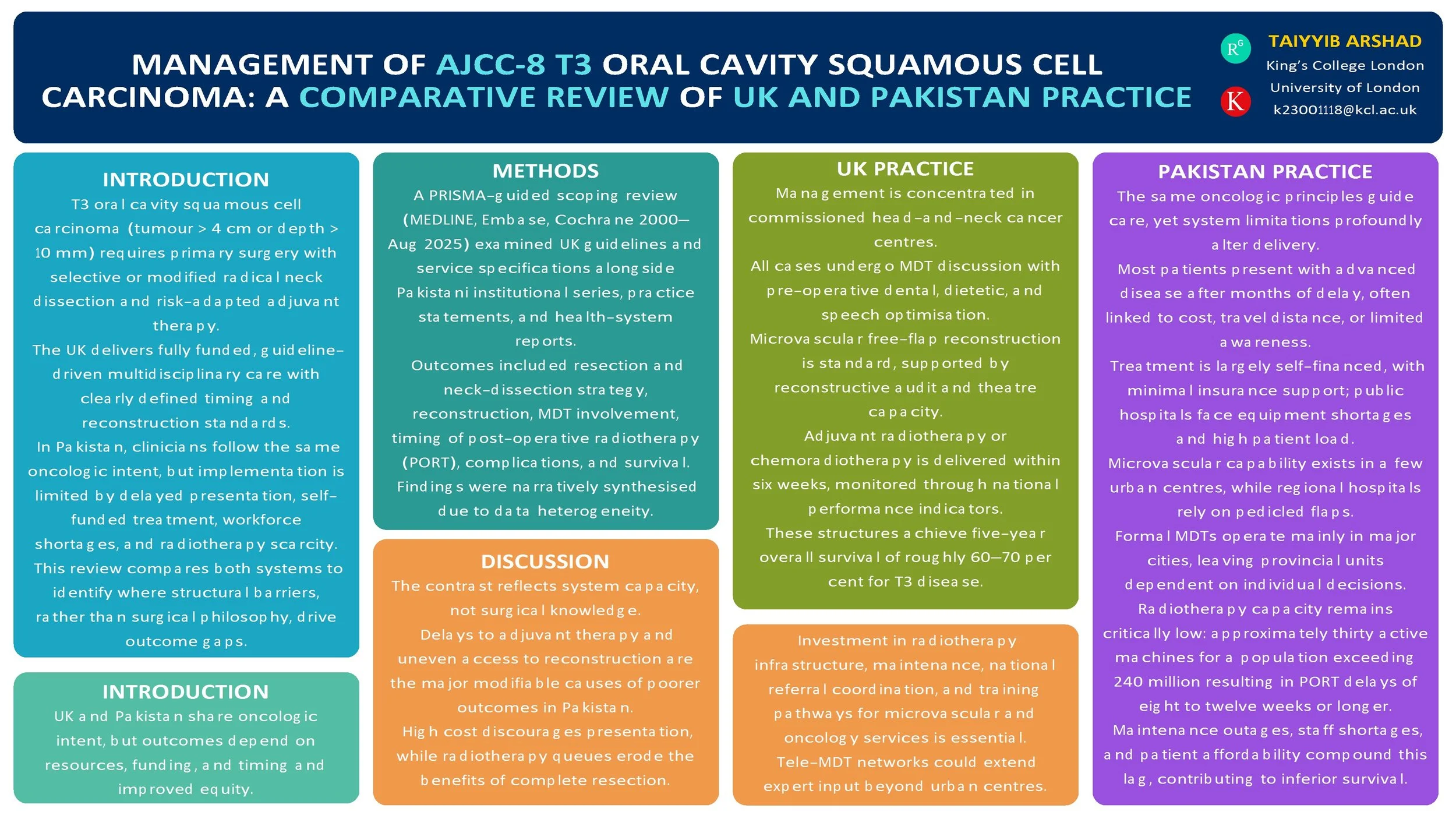
Management of AJCC-8 T3 Oral Cavity Squamous Cell Carcinoma: A Comparative Review of UK (NICE) and Pakistan Practices
Introduction
T3 oral cavity squamous cell carcinoma (OCSCC; AJCC-8: tumour > 4 cm or depth of invasion > 10 mm) is managed with primary surgery and risk-adapted adjuvant therapy. The UK delivers guideline-driven multidisciplinary care, while Pakistan applies the same oncologic principles within more heterogeneous resource settings. We compared published guidance and real-world practice to identify convergences, gaps, and opportunities for pathway improvement.
Method
PRISMA-guided scoping review (MEDLINE, Embase, Cochrane, and grey literature, 2000–Aug 2025). We included: (i) UK guidelines/standards for oral cavity cancer; (ii) Pakistan institutional series and practice statements for T3 OCSCC; (iii) health-system reports on multidisciplinary team (MDT) availability and radiotherapy capacity. Outcomes: resection and neck-dissection strategy, reconstruction modality, positive margins, time to post-operative radiotherapy (PORT), complications, recurrence, and survival. Data were charted narratively due to heterogeneity.
Results
UK sources consistently recommend upfront resection with appropriate ipsi/contralateral neck dissection, microvascular reconstruction when indicated, and adjuvant RT/CRT for adverse features, delivered through MDT pathways with staging, dental, and nutritional optimisation. Pakistan tertiary centres report adherence to core surgical principles with growing microvascular capability; regional flaps are used where resources are constrained. Across Pakistan reports, later stage at presentation is common; MDT access and radiotherapy capacity vary, contributing to PORT delays. Broader head-and-neck literature links delayed PORT (>6 weeks) with inferior outcomes. No head-to-head UK–Pakistan comparative cohort specific to T3 OCSCC outcomes was found.
Conclusion
Oncologic intent is aligned, but system-level factors—MDT coverage, reconstructive resources, and timely access to PORT—likely drive differences in delivered care and outcomes. Standardised, context-adapted pathways (routine MDT triage, clear neck algorithms, reconstruction choice matched to resources, and fast-tracked PORT) and a bi-national registry focused on T3 OCSCC are warranted to benchmark timing, treatment patterns, and outcomes.
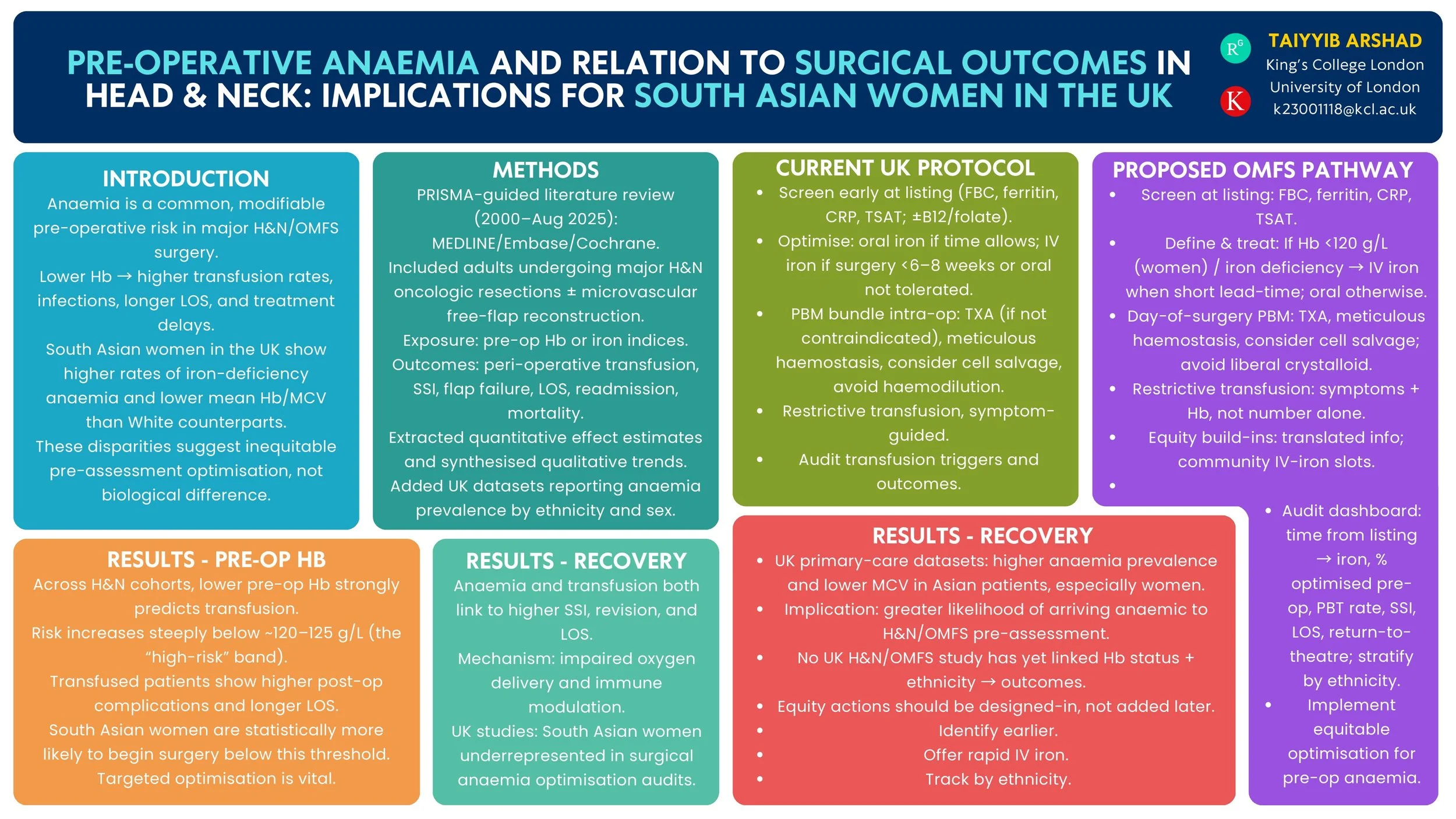
Pre-operative Anaemia and Surgical Outcomes in Head & Neck Surgery: Implications for South Asian Women in the UK
Introduction
Pre-operative anaemia is a modifiable risk factor that increases complications after head & neck (H&N) surgery. UK primary-care data show a higher burden of anaemia among women of Asian heritage than White women. We reviewed the evidence on pre-operative anaemia and H&N/OMFS surgical outcomes and summarised UK epidemiology by ethnicity to inform equity-focused peri-operative pathways.
Method
PRISMA-guided review (MEDLINE/Embase/Cochrane, 2000–Aug 2025). Inclusion: studies of H&N/OMFS surgery reporting pre-operative haemoglobin/iron indices vs peri-operative outcomes (transfusion, surgical-site infection, return to theatre, flap failure, length of stay, readmission, mortality, oncological endpoints). We additionally summarised UK population/primary-care studies reporting anaemia prevalence in women by ethnicity and current UK peri-operative anaemia guidance.
Results
Across H&N cohorts and syntheses, lower pre-operative haemoglobin independently associates with higher peri-operative transfusion and adverse outcomes; a high-risk transfusion threshold is consistently observed around ~120 g/L. UK guidance recommends routine pre-operative screening and optimisation (including intravenous iron) for major surgery. UK primary-care datasets demonstrate higher anaemia prevalence and lower mean haemoglobin/MCV among Asian compared with White patients, indicating that women of South Asian heritage are more likely to present anaemic before surgery. No UK H&N/OMFS study has yet quantified outcome differences by both anaemia status and ethnicity.
Conclusion
Robust evidence links pre-operative anaemia with worse H&N surgical outcomes, and UK datasets show higher anaemia prevalence in Asian women. These findings support a standardised OMFS/H&N anaemia optimisation pathway—early case-finding, iron studies, rapid IV iron, and transfusion-sparing strategies—with particular attention to access and uptake among South Asian women. Future UK multicentre analyses should test whether ethnicity modifies anaemia-related surgical risk and evaluate pathway impact on complications and treatment delays.
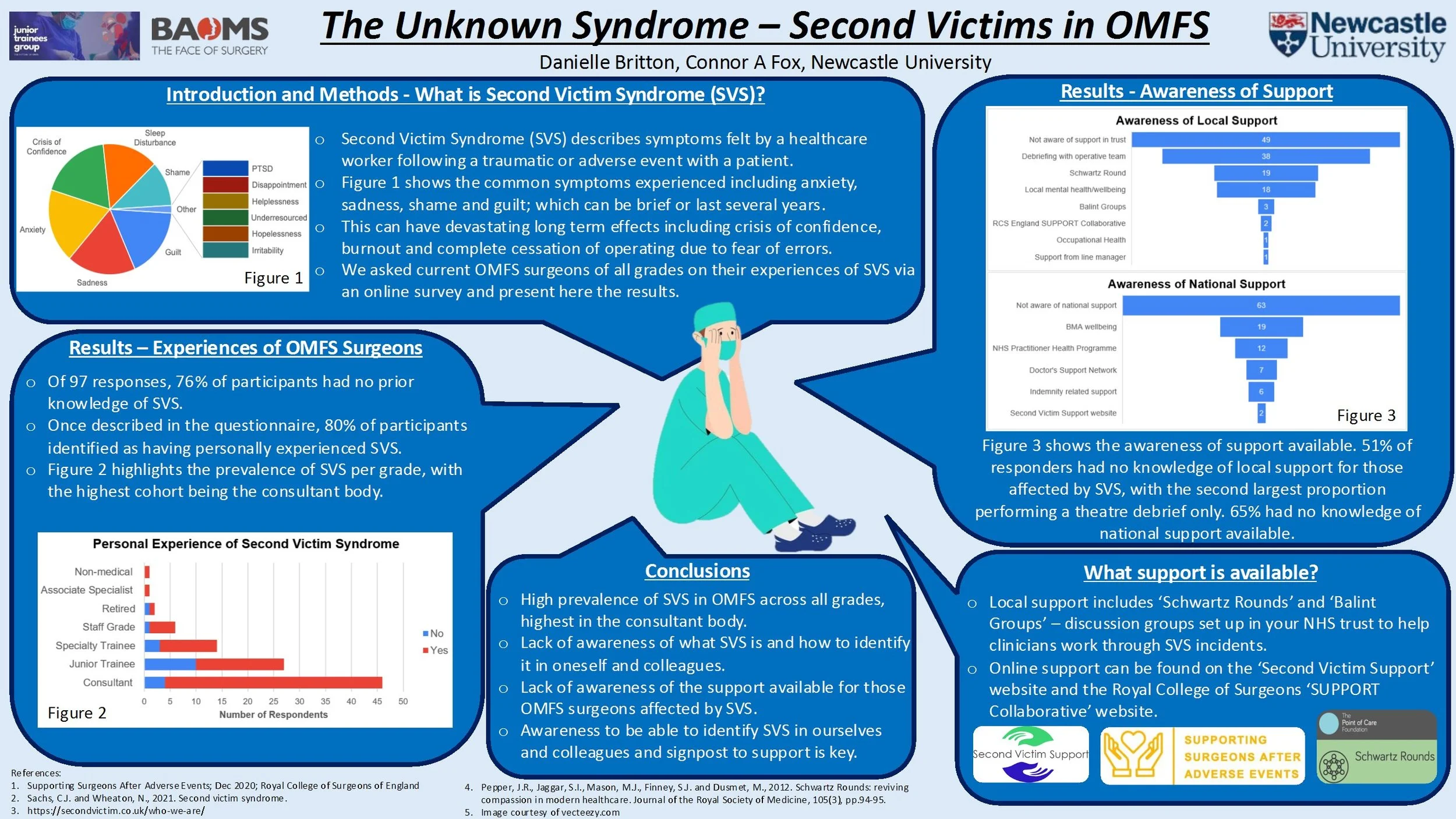
The Unknown Syndrome – Second Victims in OMFS
Second victim syndrome within surgery encompasses the psychological and physical symptoms surgeons can experience after an adverse event. Post-traumatic symptoms amongst surgeons equal those experienced by military personnel returning from conflict. These symptoms can lead to workplace errors, crises of self-confidence and, over time, complete cessation of operating.
The Royal College of Surgeons of England (RCS) recently developed guidance on supporting surgeons after adverse events and the “SUPPORT” collaborative to help those affected. At the time of writing, no work has been conducted into increasing awareness or evaluating the impacts of second victim syndrome within OMFS in the UK, nor how we as a specialty can best support those affected.
Performed as part of the BAOMS student bursary, this research assesses the prevalence of second victim symptomatology within OMFS colleagues of all levels (junior trainees to consultant level) through the use of electronic surveys. These surveys gathered information including awareness of second victim syndrome, knowledge of support currently available, anonymous personal experiences, and what further support could be beneficial for those affected.
With the knowledge gained, this project aims to provide education and increase awareness of second victim syndrome, its symptoms, signpost to support currently available for OMFS surgeons and trainees, and highlight how clinical leads can improve post-trauma support within their own units.
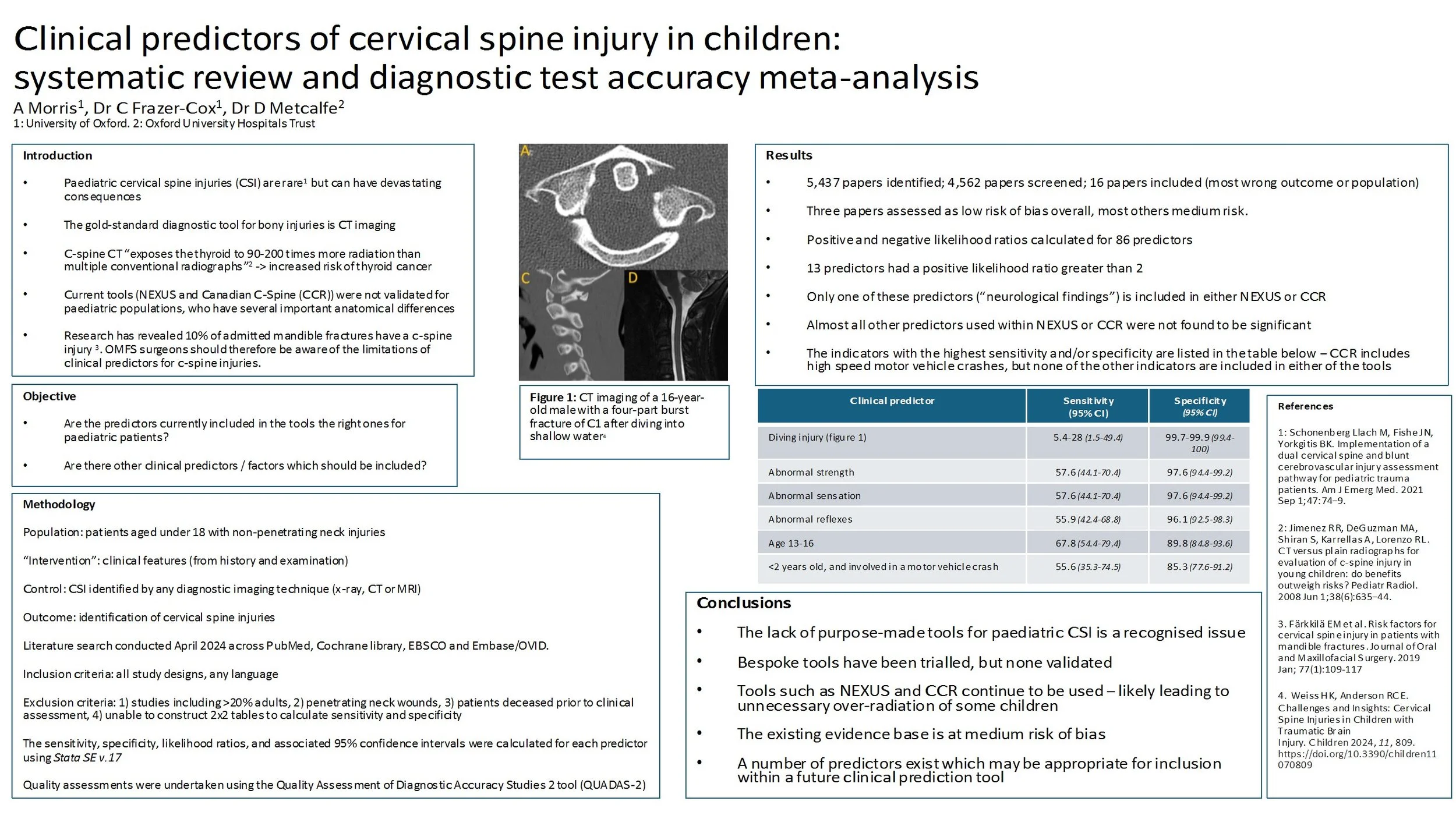
Clinical predictors of cervical spine injury in children: systematic review and diagnostic test accuracy meta-analysis
Introduction: Clinical decision rules for identifying which cervical spine injuries (CSI) require diagnostic radiography were validated in adult populations, whose necks are anatomically very different to those of children. Their accuracy in children is unclear. This review sought to identify clinical predictors of non-penetrating CSI in children and propose candidates for a modified decision tool.
Method: A systematic review and meta-analysis of diagnostic test accuracy studies that evaluated the ability of clinical features to identify CSI in patients younger than 18 years old. The search was conducted on 18 April 2024. Language limits were not applied. All traumatic, non-penetrating neck injuries were included, except where patients died due to their injuries prior to clinical assessment. The sensitivity, specificity, likelihood ratios, and associated 95% confidence intervals were reported for each predictor. Data reported by three studies was pooled using univariate random effects models, and those with four or more studies used multi-level mixed effects logistic regression models. Quality assessments were undertaken using the Quality Assessment of Diagnostic Accuracy Studies 2 tool.
Results: 16 studies reported on 9926 CSI. The most important potential source of bias was unclear/inconsistent utilisation of reference standard tools during patient assessment. The most useful clinical predictors were abnormal strength, sensation or reflexes, and age 13-16. The most important mechanisms of injury were diving, children under 2 years old involved in a motor vehicle crash, and firearms.
Conclusion: The existing evidence base is at moderate risk of bias. Predictors in existing clinical rules, validated in adults (e.g. NEXUS and CCR), often do not include good diagnostic characteristics for children. It is therefore possible that these rules do not perform as effectively in paediatric populations as in adults. A number of predictors exist that are potential candidates for inclusion within a future clinical prediction rule for paediatric CSI.
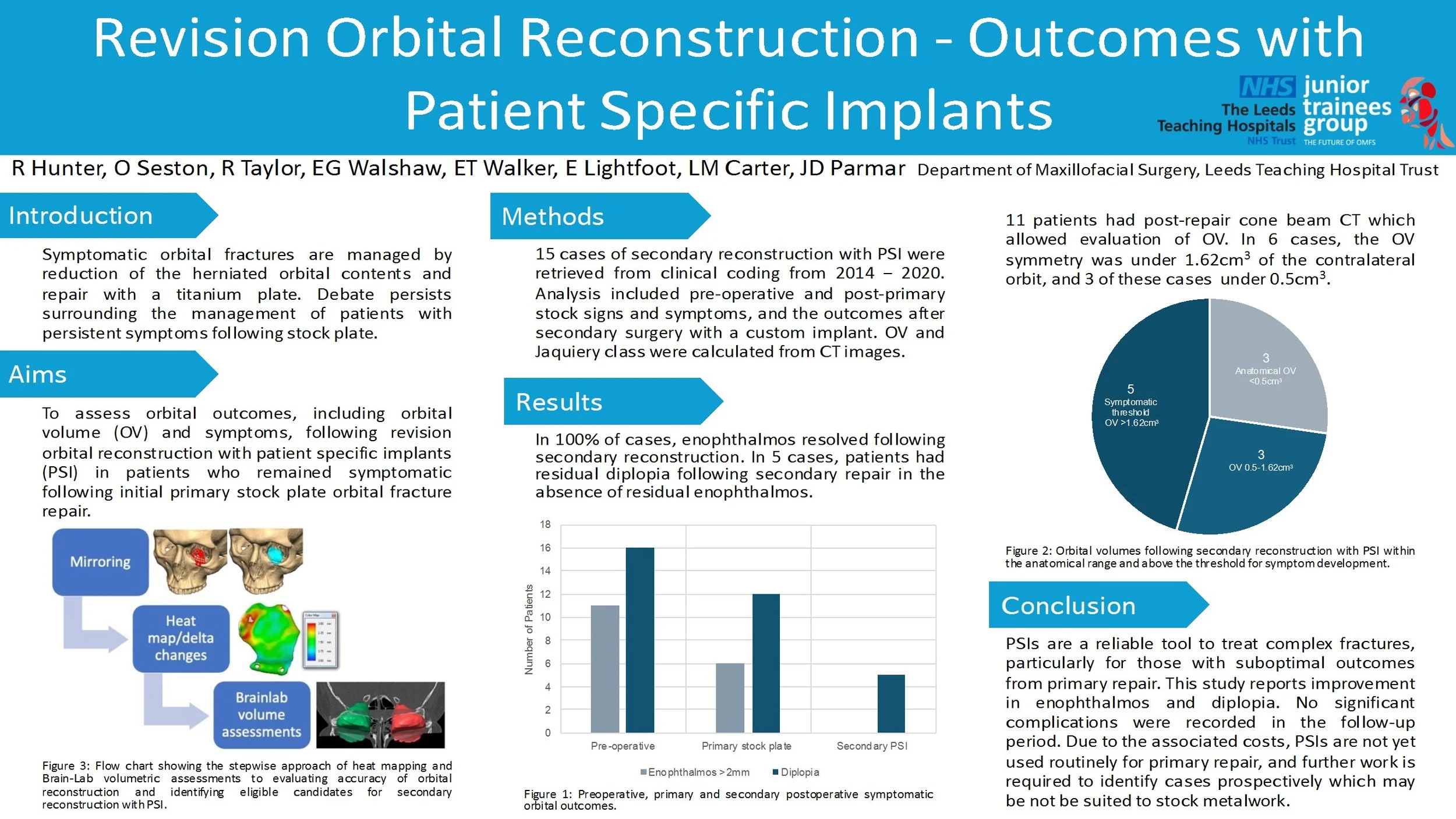
Revision Orbital Reconstruction - Outcomes with Patient Specific Implants
Introduction/Aims
The mainstay of treatment of symptomatic orbital fractures remains the reduction of herniated orbital contents and repair with a titanium plate. The management of patients who have had a stock plate with persistent symptoms is subject to debate. In this study, 15 patients underwent a novel analysis of orbital volumes (OV) and symptom assessment, prior to revision surgery with a patient specific implant (PSI).
Materials and Methods
Relevant cases were retrieved from clinical coding, operated between 2014 - 2020. After excluding 4 cases, 15 cases of revision reconstruction with PSI were analysed in detail, including pre-operative and post-primary-op signs and symptoms, and the outcomes after revision surgery with a custom implant. OV and Jaquiery class were calculated from CT images.
Results/Statistics
In 100% of cases, exophthalmos and hypoglobus resolved following revision reconstruction. In 5 cases, patients had residual diplopia following revision repair in the absence of residual exophthalmos or hypoglobus. 11 patients had post-repair cone beam CT which allowed evaluation of OV. In 6 cases, the OV symmetry was under 1.62cm3 of the contralateral orbit, and 3 of these cases under 0.5cm3.
Conclusions/Clinical Relevance
PSIs are a reliable tool to treat complex fractures, particularly for those with suboptimal outcomes from primary repair. This study reports good outcomes in terms of enophthalmos and hypoglobus with no significant complications in the followup period. Due to the associated costs, PSIs are not yet used routinely for primary repair, and further work is required to identify cases prospectively which may be not be suited to stock metalwork.
Literature review: Intraosseous Hemangiomas of the facial bones: Diagnosis and management
Introduction
Intraosseous hemangiomas of the facial bones are rare benign tumours which are vascular in nature. This vascularity makes management difficult and often require a multidisciplinary approach for management. I have reviewed published literature to outline their presentation, the diagnostic tools available and management options.
Method
Articles were searched for by using pubmed medical database and reviewing articles references for similar articles.
Results
Intraosseous haemangiomas can present as painless bony lumps on the face or as space occupying lesions which compress structures, causing associated symptoms. These can include proptosis, facial deformity and dysethesia. Rarely they are painful. They can have differing vascular pressure, with a small number presenting as a pulsatile mass with bruit. There is no clear consensus on why they form, with a history of trauma and congenital reasons being suggested.
They are often first noted on CT imaging, showing heterogeneous honeycomb appearance. The benefit of MRI in diagnosis is disputed, as they can present as either high, low or mixed intensity on T1. However, MRI is useful to review vascularity within the lesion. Incisional biopsies have a limited role due to bleeding risk.
If no functional or aesthetic concern they can be managed conservatively. Non-surgical options attempted include needle aspiration, sclerotherapy and radiotherapy, all showing mixed results.
Surgical options are complicated by bleeding risks. This can be managed by removal ‘en-bloc’ to eliminate the need to enter the lesion, whilst pre-surgery embolization has also be utilised. Partial lesion removal has also been attempted, to restore function only.
Conclusion
Intraosseous hemangiomas of the facial bones are rare and limited published evidence exists, mainly case reports. There is not yet a consensus on the most useful diagnostic tools or their management. Each lesion presents its own challenges in removal and reconstruction dependent on size and location.