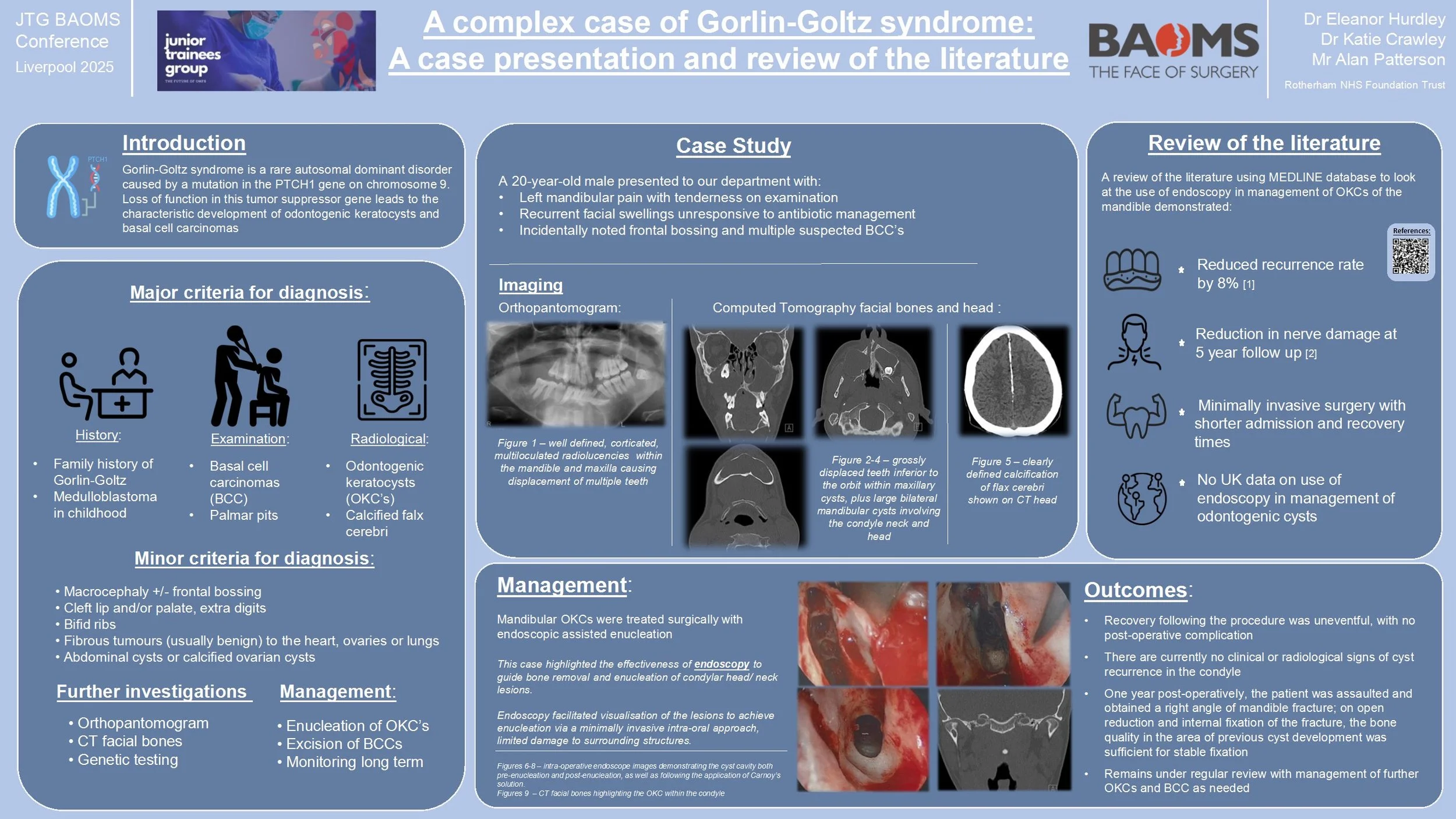
JTG 2025 Poster Gallery
Recurrent Upper Lip Cellulitis Due to MRSA : A Case Report
Abstract
Title: Recurrent Facial cellulitis due to MRSA : a case report.
Introduction
Cellulitis is a common bacterial skin infection that typically responds well to empirical antibiotic therapy. However, recurrent or non-responsive cases may signal underlying resistance, particularly due to community-acquired methicillin-resistant Staphylococcus aureus (MRSA). This report highlights the importance of microbiological diagnosis in guiding effective treatment.
Case Report
A 41-year-old male with a history of recurrent cellulitis presented with spreading erythema over the right perioral region following manipulation of a pimple. His general practitioner prescribed oral co-amoxiclav, but symptoms worsened, prompting hospital admission for intravenous flucloxacillin. The infection initially improved, but a small abscess developed and was surgically drained.
Ten days later, the patient reported significant improvement with only residual scarring. However, erythema recurred in the same area one week later. Oral metronidazole was initiated, resulting in partial improvement, but symptoms returned before the course was completed. Microbiological analysis of the drained abscess revealed MRSA, resistant to beta-lactam antibiotics and sensitive only to cotrimoxazole and vancomycin. The patient was transitioned to oral cotrimoxazole, leading to marked and sustained improvement at one-week follow-up.
Discussion
This case underscores the diagnostic challenges in managing recurrent cellulitis. Initial empirical therapy may be ineffective against resistant organisms such as MRSA, delaying recovery and increasing the risk of complications. Early microbiological sampling and sensitivity testing are essential in guiding targeted antibiotic therapy. Clinicians should maintain a high index of suspicion for MRSA in recurrent or non-responsive skin infections and consider culture-directed treatment to optimize outcomes and prevent recurrence.
Case Report: Reconstruction of Labial Commissure, Lip and Buccal Mucosa following Resection of Recurrent Squamous Cell Carcinoma in a Previously Irradiated Field
Background: 70-year-old female previously treated for Squamous Cell Carcinoma (SCC) of the right mandible and right labial commissure represents with a non-healing ulcer on the right labial mucosa extending to the maxillary alveolus. Reconstruction following resection of the SCC poses a significant challenge due to previous radiotherapy associated with treatment of the SCC on the right labial commissure, a field needed in reconstruction of the resected site. The aim of the patient’s treatment being tumour resection, restoration of function and a level of aesthetic restoration.
Methods: Careful consideration of reconstructive flap in this case was needed due to the compromised vascularity of the previously irradiated tissue. A modified Karapandzic flap along with a V-Y flap and placement of Integra intraorally was the treatment modality of choice, conserving nerves, enhancing blood supply as well as providing adequate adaptation and functional restoration.
Results: The selected flaps provided majority stable wound healing, restored oral competence, and preserved speech and oral intake. The patient recovered without major complications.
Conclusion: Oral commissure reconstruction in previously irradiated patients requires meticulous flap selection to optimise vascularity and function. A tailored approach is essential to achieving functional and aesthetic outcomes while satisfying the primary objective of complete tumour excision.
An incidental finding of a Complex Odontoma – A reminder regarding the importance of routine investigations
An incidental finding of a Complex Odontoma – A reminder regarding the importance of routine investigations
Maria-Alexandra Barbu1, Cristina Frezzini1, Iain Varley1
1-Department of Oral and Maxillofacial Surgery Department
Sheffield Teaching Hospitals NHS Foundation Trust
Abstract
Introduction:
Complex odontomas are rare odontogenic tumors composed of a disorganized mass of dental tissues, typically detected during routine radiographic examinations. They represent a developmental anomaly rather than a true neoplasm and are most often diagnosed in the first two decades of life. Although usually asymptomatic, complex odontomas may impede eruption of permanent teeth or alter the normal development of adjacent anatomical structures, warranting early recognition and appropriate management.
Case report:
We report the case of an 11-year-old fit and well female who presented with a complex odontoma of the LR7 region. This was an incidental finding following imaging taken for orthodontic treatment purposes.
We describe the investigation, diagnosis and management of this child’s condition.
Discussion:
This case highlights the incidental detection of a complex odontoma during orthodontic evaluation and underlines the potential implications for tooth eruption and mandibular growth. Multidisciplinary input involving orthodontics and oral and maxillofacial surgery is crucial for establishing an appropriate management plan, balancing surgical intervention with preservation of developing teeth and the inferior alveolar nerve. Early diagnosis allows timely intervention, preventing complications such as impaction, malocclusion, or pathological fracture. Recognition of odontomas as incidental findings on panoramic radiographs emphasizes their significance in orthodontic and pediatric dental practice.
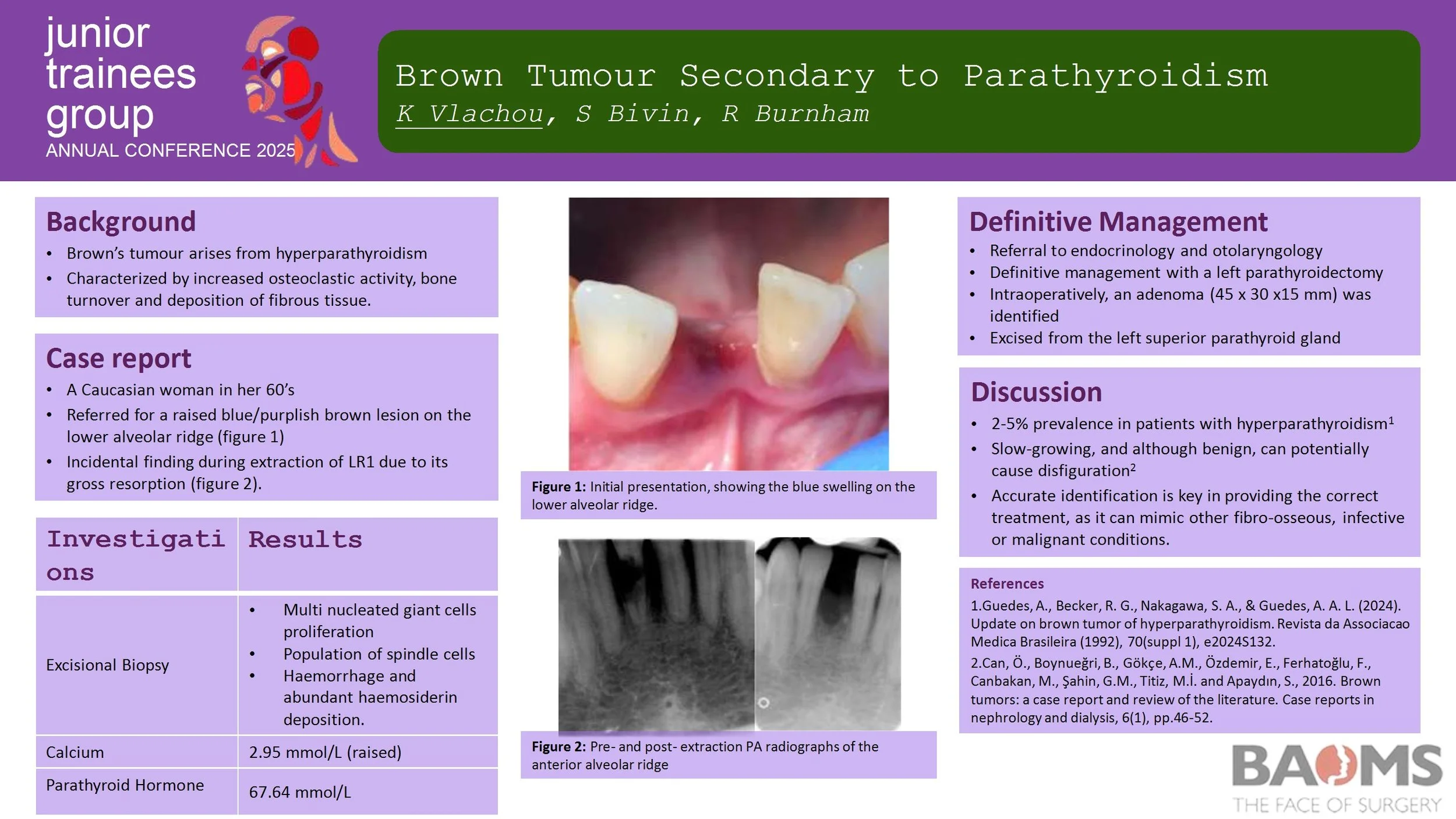
Brown Tumour Secondary to Parathyroidism
Introduction
Brown’s tumour (osteitis fibrosa cystica) is a rare, non-neoplastic condition resulting from hyperparathyroidism. It is characterized by increased osteoclastic activity and bone turnover, which subsequently leads to the deposition of fibrous tissue. It generally affects long bones of the body, however it can affect facial bones, particularly the mandible. It can mimic other fibro-osseous, infective or malignant conditions.
Case Report
We report the case of a 67-year-old female with primary hyperparathyroidism. The initial swelling was found incidentally during an extraction. Radiographic appearance reported root resorption to adjacent teeth, whilst histological findings consisted of the typical multi-nucleated giant cells. Increased blood calcium and parathyroid hormone levels have confirmed primary impression.
Discussion
Brown's tumour is often a diagnostic challenge as it is misdiagnosed, particularly as a malignant lesion. Early detection is key in order to provide the appropriate treatment not only for the lesions but also for the underlying HPT.
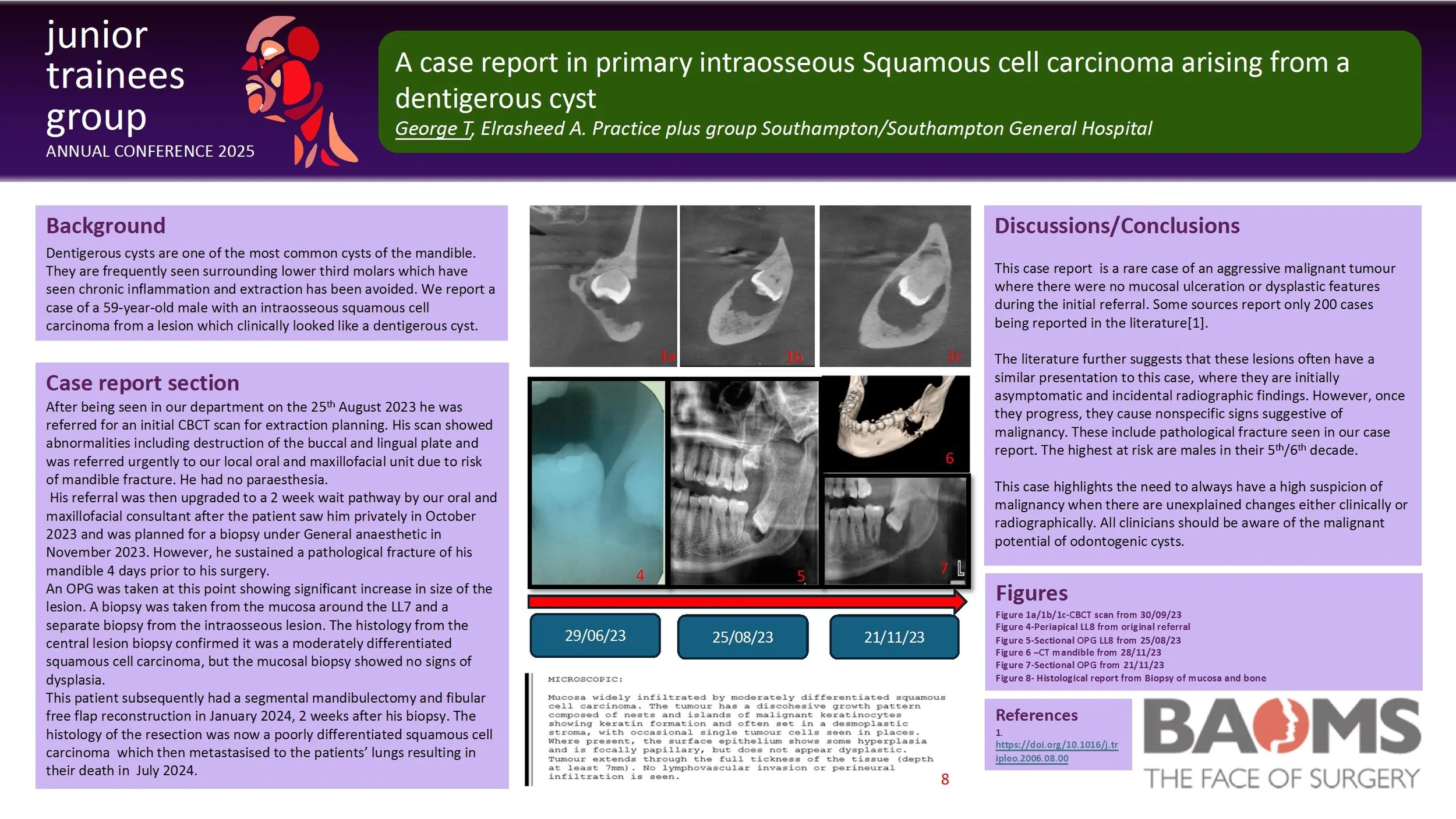
A case report in primary intraosseous Squamous cell carcinoma arising from a dentigerous cyst
Dentigerous cysts are one of the most common cysts of the mandible. They are frequently seen surrounding lower third molars which have seen chronic inflammation and extraction has been avoided. We report a case of a 59-year-old male with an intraosseous squamous cell carcinoma from a lesion which clinically looked like a dentigerous cyst.
He was referred by his General Dental Practitioner to our oral surgery department for extraction of a symptomatic LL8 in June 2023. His initial CBCT scan showed abnormalities including destruction of the buccal and lingual plate and was referred urgently to our local oral and maxillofacial unit due to risk of mandible fracture. He had no paraesthesia.
His referral was then upgraded to a 2 week wait pathway by our oral and maxillofacial consultant after the patient saw him privately in October 2023 and was planned for a biopsy under General anaesthetic in November 2023. However, he sustained a pathological fracture of his mandible 4 days prior to his surgery. An OPG was taken at this point showing significant increase in size of the lesion.
A biopsy was taken from the mucosa around the LL7 and a separate biopsy from the intraosseous lesion. The histology from the central lesion biopsy confirmed it was a moderately differentiated squamous cell carcinoma, but the mucosal biopsy showed no signs of dysplasia.
This patient subsequently had a segmental mandibulectomy and fibular free flap reconstruction in January 2024, 2 weeks after his biopsy. The histology of the resection was now a poorly differentiated squamous cell carcinoma.
This highlights an unusual case of an aggressive malignant tumour where there was no mucosal ulceration or dysplastic features. It emphasises the importance of reassessing the patient’s clinical picture and to be aware of the potential malignant change of odontogenic cysts.
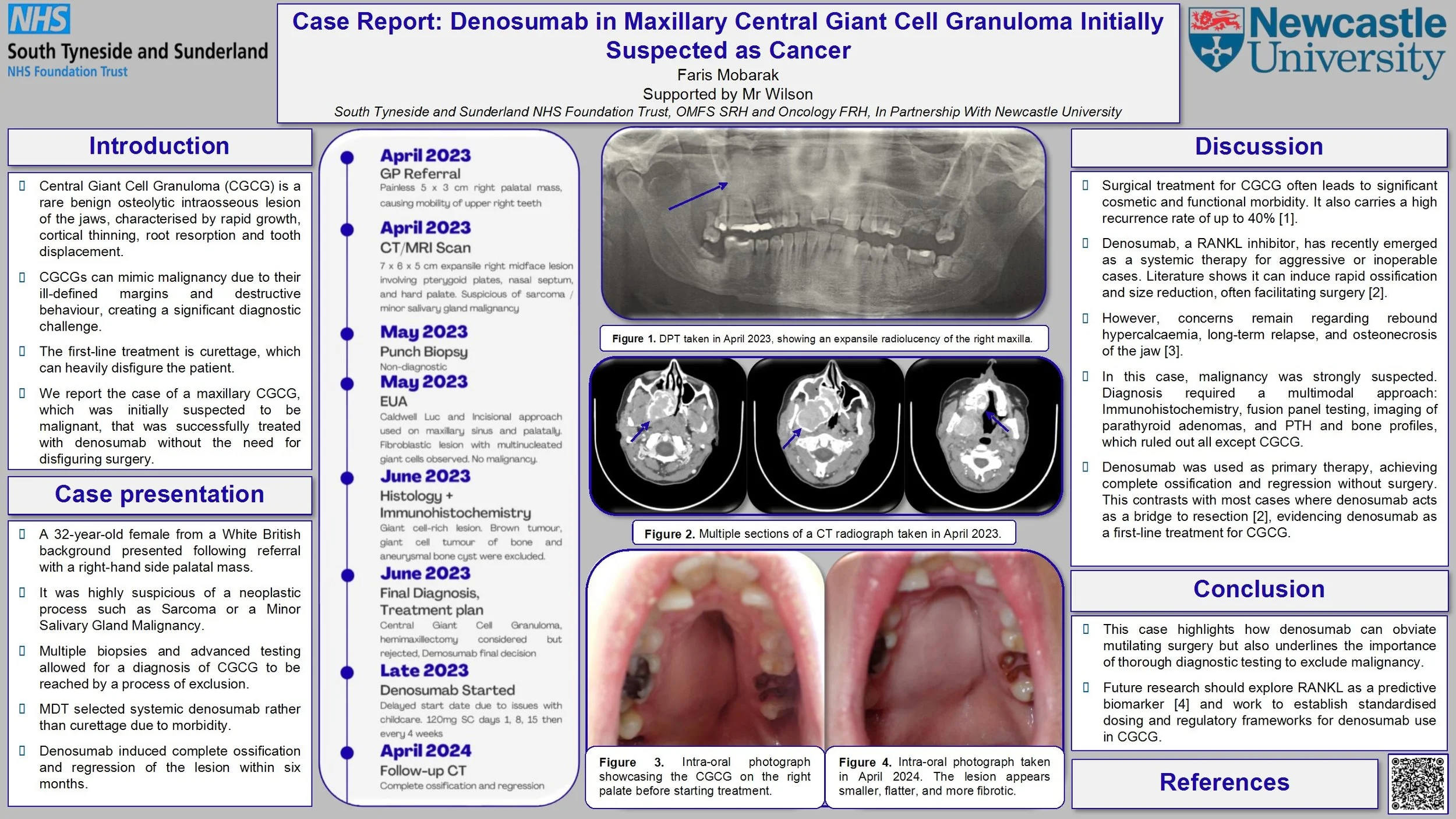
Case Report: Denosumab in Maxillary Central Giant Cell Granuloma Initially Suspected as Cancer
Introduction: Central Giant Cell Granuloma (CGCG) is a benign osteolytic lesion of the jaw that can present with aggressive radiographic features such as cortical thinning, root resorption, tooth displacement, and ill-defined margins that mimic malignancy and risk misdiagnosis. While surgical management remains the first-line therapy for CGCG, this case covers the use of denosumab, which successfully prompted ossification and lesion regression without the need for disfiguring surgery.
Case Report: We report the unusual case of a 32-year-old Caucasian female who presented in April 2023 at an emergency dental appointment with a 5 x 3 cm firm, non-ulcerated right palatal mass and mobile upper right molars. CBCT and MRI demonstrated an ill-defined, expansile, vascular lesion of the right maxilla invading the sinus, nasal floor and pterygoid plates without orbital or intracranial extension. Deep biopsies were taken under GA via Caldwell-Luc and palatal incision. Histology reported a fibro-cellular stroma with numerous osteoclast-type giant cells. Giant cell tumour of bone, aneurysmal bone cyst and brown tumour were excluded by immunohistochemistry testing and blood tests. A multidisciplinary team (MDT) discussion confirmed the diagnosis of CGCG. Given the lesion’s size and location, systemic therapy with denosumab was initiated. Multiple CT scans indicated progressive ossification and reduction in lesion volume following administration of denosumab. At a 12-month follow-up after discontinuation of treatment, the lesion remained stable, with preserved dentition and no functional or aesthetic deficits.
Discussion: Our case illustrates the diagnostic dilemma in CGCG, necessitating deep surgical biopsy, comprehensive immunohistochemistry, and multidisciplinary team coordination to rule out malignancy. It also demonstrates denosumab as an effective, tissue-sparing alternative to the extensive resection typically carried out.
Parotid Secretory Carcinoma Presenting As A Cystic Lesion: A Case Report
Introduction:
Secretory carcinomas are low grade malignant tumours which most commonly affect the parotid glands. This report describes the case of a 29-year-old male presenting via the two-week-wait pathway with a left parotid lump without sinister features, risk factors and inconclusive pre-operative investigations. The option to pursue further lesion characterisation was discussed, however the patient elected to undergo treatment for the likely benign cystic lesion which was unexpectedly found to be a secretory carcinoma.
Case Report:
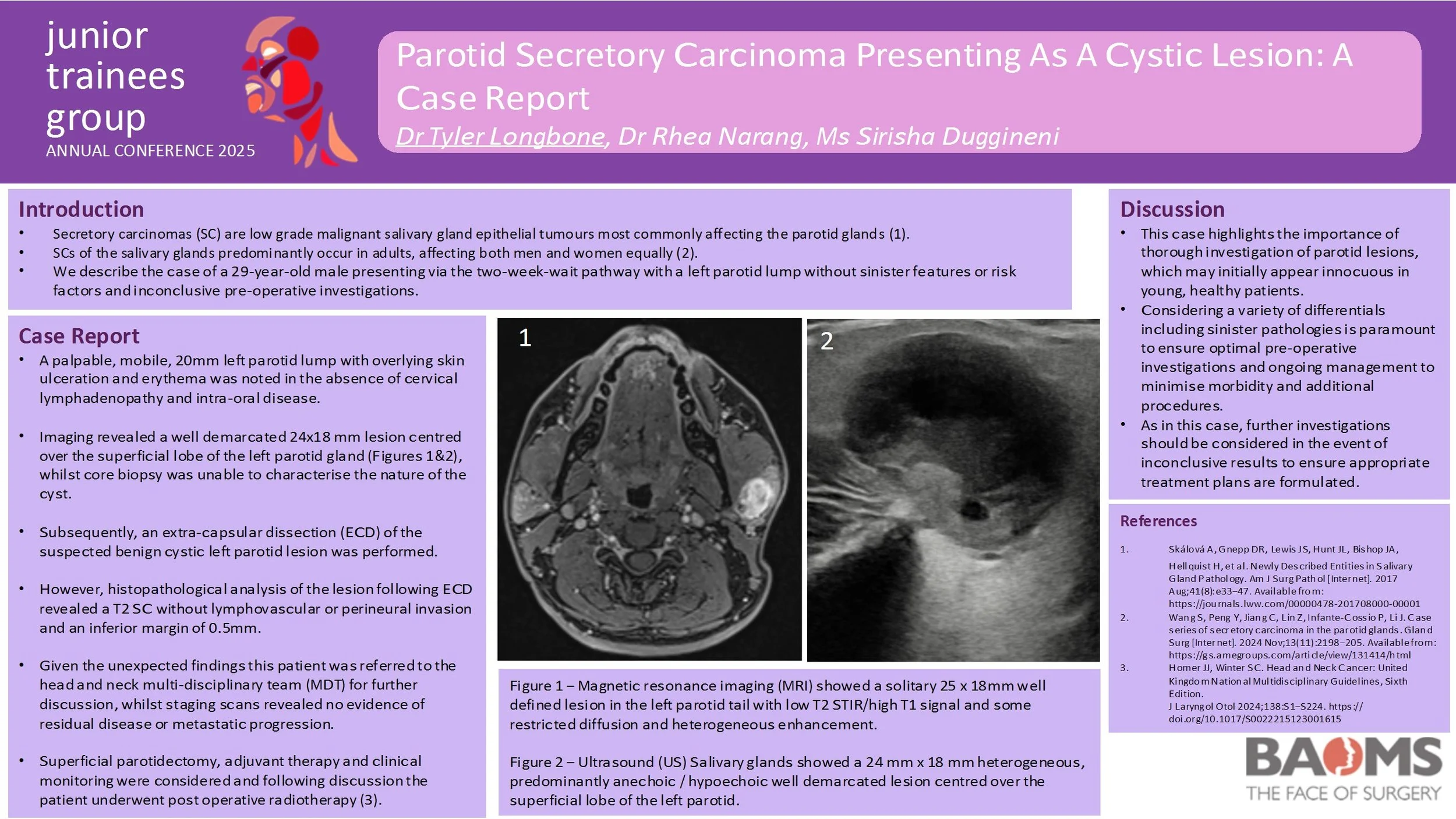
On review a palpable, mobile, 20mm left parotid lump with overlying skin ulceration and erythema was noted in the absence of cervical lymphadenopathy and intra-oral disease. Pre-operative imaging revealed a well demarcated 24x18 mm lesion centred over the superficial lobe of the left parotid gland, whilst core biopsy was unable to characterise the nature of the cyst. However, histopathological analysis of the left parotid lesion following extra-capsular dissection revealed a T2 secretory carcinoma without lymphovascular or perineural invasion and an inferior margin of 0.5mm. Subsequent staging scans did not demonstrate evidence of residual disease or metastatic progression.
This patient initially underwent extra-capsular dissection of the suspected benign cystic left parotid lesion. Given the unexpected histopathological findings this patient was referred to the head and neck multi-disciplinary team (MDT) for further discussion. Superficial parotidectomy, adjuvant therapy and clinical monitoring were considered and following discussion the patient underwent post operative radiotherapy.
Discussion:
This case highlights the importance of thorough investigation of parotid lesions, which may initially appear innocuous in young, healthy patients. Undoubtedly, considering a variety of differentials including sinister pathologies is paramount to ensure optimal pre-operative investigations and ongoing management to minimise morbidity and additional procedures.
Orbital Roof Reconstruction Utilizing Inverted Orbital Floor Plates - A Case-Based Technical Note
Background: Orbital roof fractures are rare [1] but significant injuries resulting from high-energy trauma, often alongside complex maxillofacial injuries [2,3]. Surgical repair is indicated for displaced fractures with neurological or ophthalmic compromise [4]. Traditional reconstruction with titanium mesh presents challenges such as insufficient rigidity, sharp edges, implant extrusion risk, and difficulty of removal if infected. As such, we propose using pre-shaped orbital floor plates, inverted for orbital roof reconstruction, offering improved structural support and a more ergonomic surgical experience.
Methods: Retrospective case series (n=4) of patients undergoing surgical repair for orbital roof fractures. A bicoronal and pericranial flap was raised, followed by hemifrontal craniotomy. Orbital roof defects were visualised, dural tears repaired, and reconstruction performed using inverted orbital floor plates secured with screws. A pericranial flap covered the repair, and the bone flap was re-fixed with low-profile plating. Postoperative outcomes were assessed.
Results: All cases achieved correct orbital roof alignment and restoration of orbital volume. No implant-related infections were found. Progressive recovery or complete resolution of ocular symptoms was observed, even in severe trauma patients.
Discussion: This case series demonstrates the feasibility, safety, and structural adequacy of using inverted orbital floor plates for orbital roof reconstruction. This alternative offers greater rigidity, easier handling, anatomical contour matching and immediate availability in trauma settings, with good outcomes even in severe trauma. Study limitations include small sample size due to the rarity of the fracture, heterogeneous trauma profiles, and limited long-term follow-up. Therefore, further studies are needed to confirm long-term outcomes.
Dental abscess or something more?
Introduction:
Necrotising fasciitis is a rare, rapidly progressive soft tissue infection with high morbidity and mortality, often polymicrobial (Type I) and associated with immunocompromised states. Prompt recognition and aggressive surgical management are essential.
Case report:
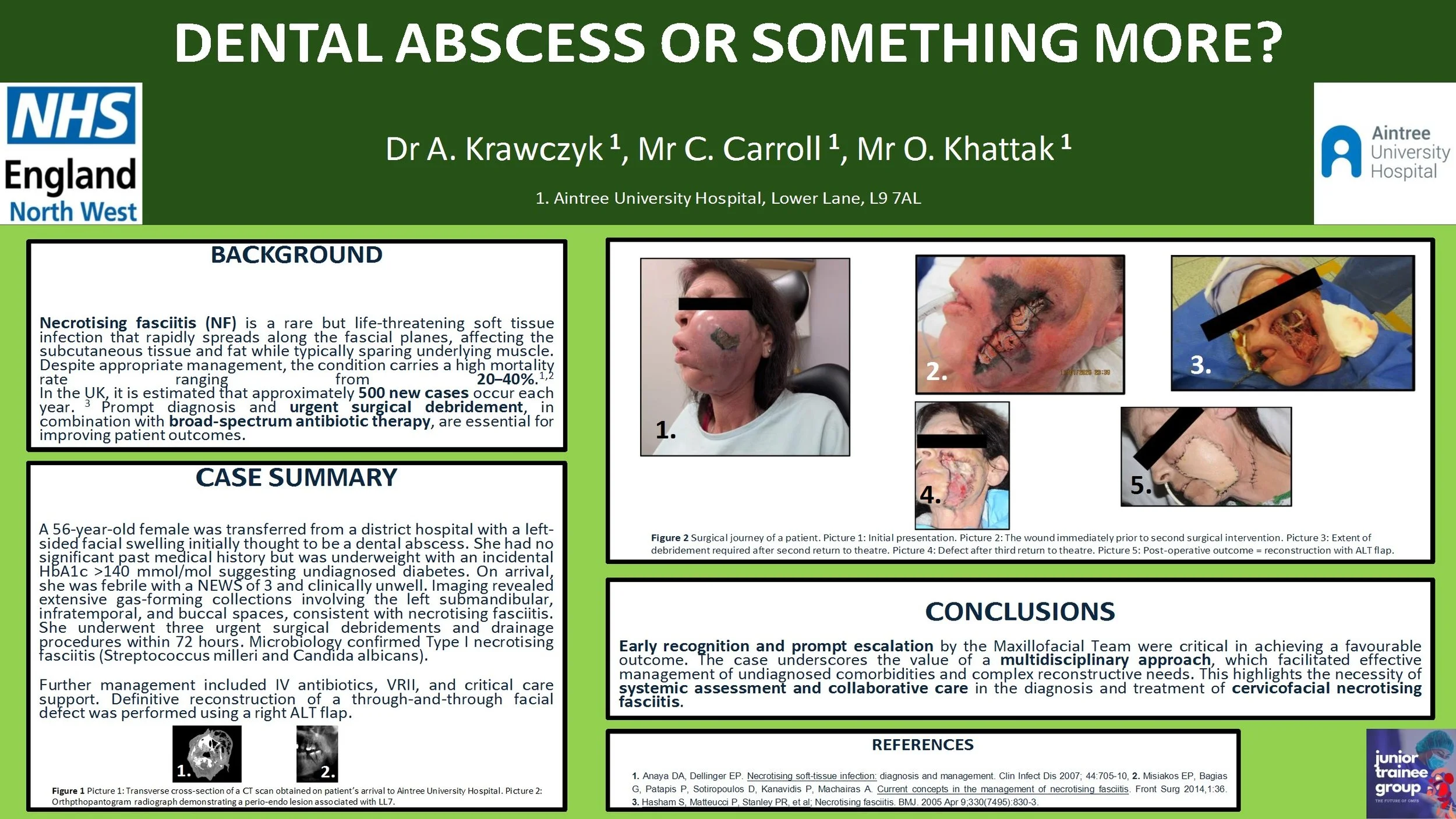
A 56-year-old female was transferred from a district hospital with a left-sided facial swelling initially thought to be a dental abscess. She had no significant past medical history but was underweight with an incidental HbA1c >140 mmol/mol suggesting undiagnosed diabetes. On arrival, she was febrile with a NEWS of 3 and clinical unwell. Imaging revealed extensive gas-forming collections involving the left submandibular, infratemporal, and buccal spaces, consistent with necrotising fasciitis. She underwent three urgent surgical debridements and drainage procedures within 72 hours. Microbiology confirmed Type I necrotising fasciitis (Streptococcus milleri and Candida albicans). Further management included intravenous antibiotics, variable rate insulin infusion, and critical care support. Definitive reconstruction of a through-and-through facial defect was performed using a right antero-lateral thigh free flap.
Discussion:
Early recognition and escalation by the on-call Maxillofacial team were key to successful outcomes. A multidisciplinary approach enabled management of complex comorbidities and reconstruction. This case highlights the importance of systemic evaluation and team-based care in managing cervicofacial necrotising fasciitis.
Reconstruction of Multifocal Comminuted Facial Fractures Caused by a Horse Kick
Introduction
Naso-orbital-ethmoidal (NOE) fractures are uncommon, complex facial fractures that
are often sustained following higher energy injury mechanisms. Common
mechanisms include road traffic accidents, sports injuries and horse kicks.
Anatomically, the NOE complex lies close to key facial structures including the orbits
and the anterior cranial fossa so damage to this complex can result in damage to
nearby structures. This can result in serious complications such as changes to vision
and intercranial infections.
Case Report
This case presents a 19-year-old patient who presented to the emergency
department following a horse kick to the face. Initial examinations revealed proptosis
and increased intercanthal distance. Imaging showed us that there were multifocal
comminuted fractures that involved the NOE complex, anterior cranial fossa, the
orbits, a retro-orbital haematoma, a small subdural haemorrhage and a small,
depressed skull fracture. The NOE fracture was determined to be a type 2 fracture
according to the Markowitz and Manson classification. Despite the severity of the
injuries, the patient remained GCS 15 throughout their care. For repair, an open
reduction and internal fixation using a coronal flap with cranialisation of the frontal
sinus was carried out.
Discussion
This case discusses the importance of early recognition and multidisciplinary
management of NOE fractures. Appropriate surgical intervention based on the
Markowitz and Manson classification is important in reducing complications such as
meningitis, facial deformities and ocular changes. Management of NOE fractures is
also important in order to achieve a good aesthetic outcome for the patient.
In the Deep End: 2 Cases of Odontogenic Descending Necrotising Mediastinitis (DNM)
Introduction:
Descending necrotising mediastinitis (DNM) is a rare, potentially fatal, complication of a primary odontogenic or pharyngeal infection that spreads along the cervical fascial planes into the mediastinum. Odontogenic sources represent up to 58% of cases in some reports. This report describes the management of two patients with DNM.
Case Report:
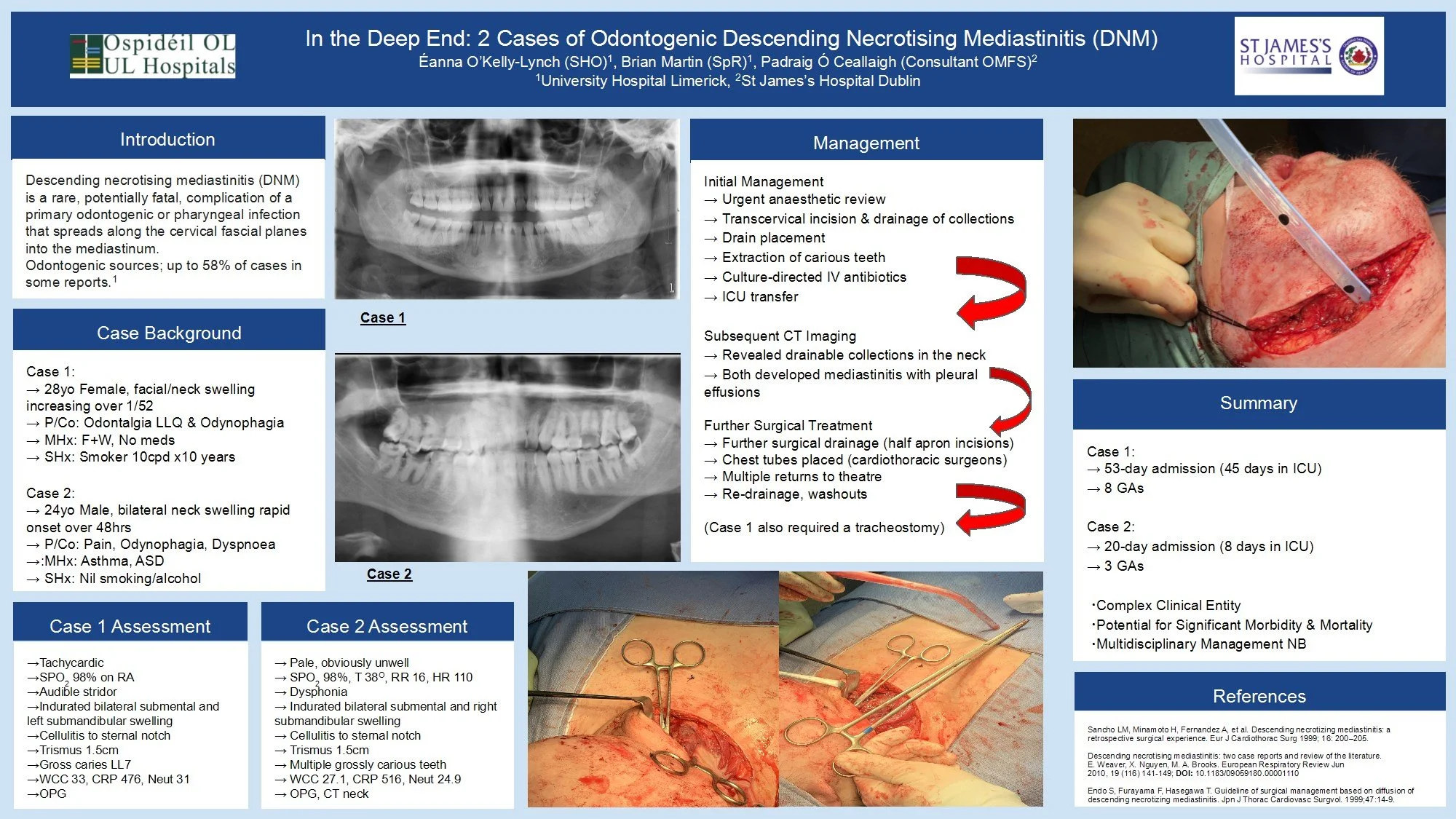
Case 1: A 28-year-old healthy female patient with one week of increasing facial and neck swelling, odontalgia and odynophagia.
Case 2: A 24-year-old male patient (asthmatic, ASD) with 48 hours of rapid-onset of bilateral neck swelling, pain, odynophagia and dyspnoea.
Both patients were tachycardic with indurated neck swellings and cellulitis, trismus, and grossly carious teeth. Bloodwork showed leukocytosis and elevated CRP.
Initial management for both involved urgent anaesthetic review, transcervical incision & drainage of collections with drain placement, and extraction of carious teeth. Culture-directed IV antibiotics were administered following ICU transfer.
Subsequent CT imaging confirmed the presence of drainable collections and need for surgical intervention. Both patients developed mediastinitis with pleural effusions, requiring drainage and placement of chest tubes.
Discussion:
Management of these cases required a multidisciplinary approach (OMFS, Cardiothoracics, Anaesthetics/Critical Care, Radiology, Microbiology) and both patients were discharged after extensive treatment courses.
Case 1: 53-day admission (45 in ICU), 8 general anaesthetics.
Case 2: 20-days admission (9 in ICU), 3 general anaesthetics.
Odontogenic infections, though common, have the potential for significant morbidity and mortality. DNM represents a challenging clinical entity that requires a prolonged and complex course of treatment. Oral and Maxillofacial Surgeons must be prepared to manage these cases and multidisciplinary input is essential.
An extensive Odontogenic Keratocyst in the left maxilla: a case report
Odontogenic Keratocysts (OKC) are benign cystic lesions that are known to be locally aggressive and have a high recurrence rate. Here we describe a case of a particularly extensive OKC.
A 28 year-old female presented to the Oral and Maxillofacial department with a 2-month history of facial swelling and pain. On examination, there was a left mid-facial swelling which was extremely tender on palpation, with intra-oral buccal expansion. Medically, she had depression and was a non-smoker. An OPG and CT neck with contrast was carried out; this revealed a substantial lesion, filling the left maxillary sinus, in association with a superiorly impacted UL8 tooth located just below the orbital apex. The lesion had cystic characteristics, measuring 6.6cm vertically, and 5.8 x 3.8cm in a transverse dimension. The lesion was shown to project medially into the nasal cavity, resulting in septal deviation to the right. Superiorly, there was associated convex bulging of the orbital floor.
Subsequently, antibiotics were prescribed; enucleation of the cyst and extraction of UL8 was carried out. The pathology result was in favour of Odontogenic Keratocyst. Infection reoccurred 1 month later which led to a washout of the cystic cavity, placement of a drain, extraction of a resorbed UL6 and additional antibiotic therapy. Gabapentin was then commenced due to associated neuropathic pain. 3 months following initial surgery, further enucleation of a 1x1cm residual cyst was carried out. 6 months later, a repeat CT scan revealed mildly progressive bony infill in line with ongoing healing and no evidence of recurrence.
This case highlights the aggressive nature of the OKC despite their slow growth. The presence of such an expansile lesion in the maxillary sinus with an associated ectopic tooth just below the orbital apex is rare. Close follow-up to detect recurrence is important.