JTG 2025 Poster Gallery
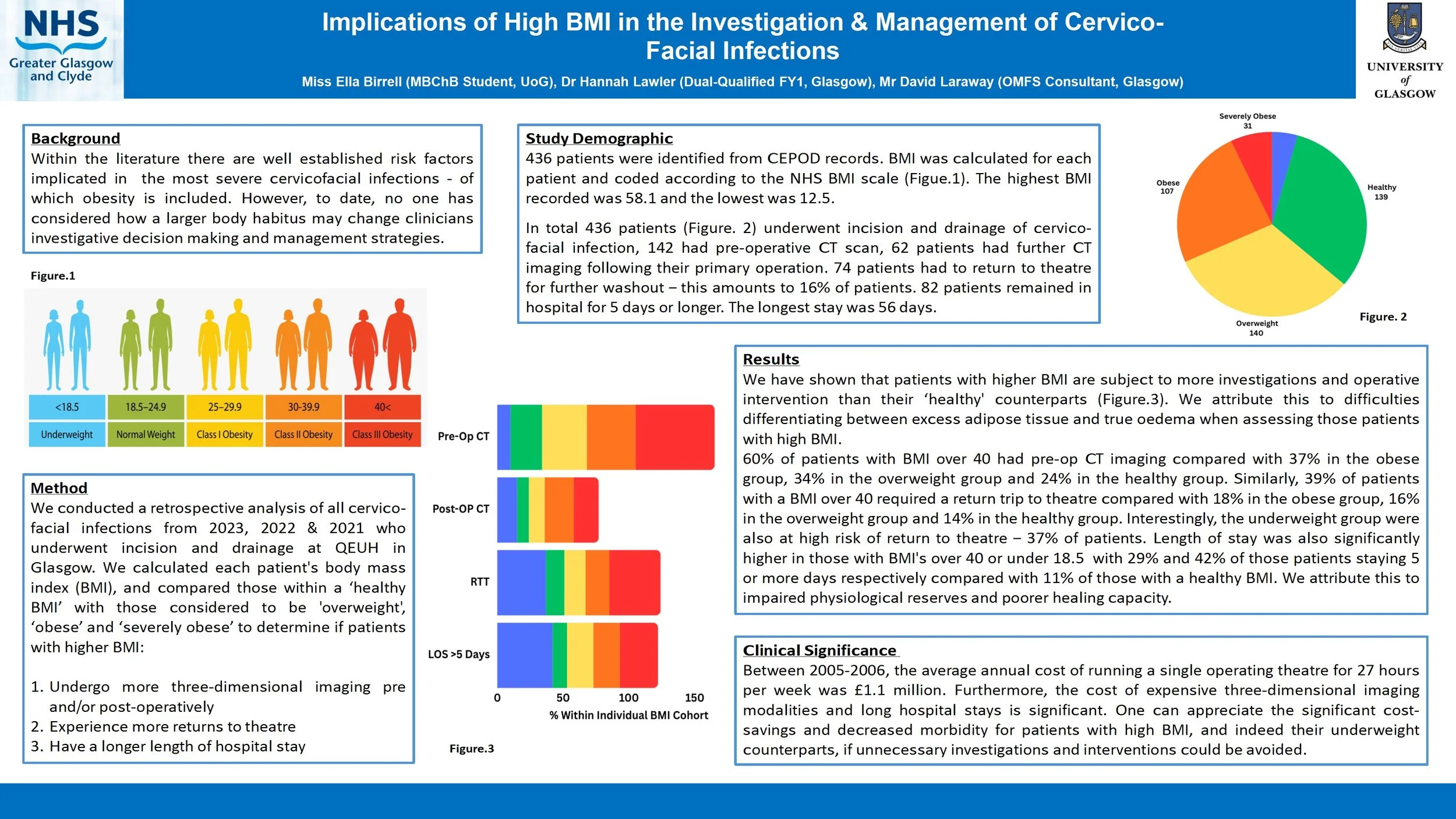
Implications of High BMI in the Investigation & Management of Cervico-Facial Infections
Introduction
Within the literature there are well established risk factors implicated in the most severe cervicofacial infections - of which obesity is included. However, to date, no one has considered how a larger body habitus may change clinicians investigative decision making and management strategies.
Method
We conducted a retrospective analysis of all cervico-facial infections over the last 6 years who underwent incision and drainage at QEUH in Glasgow. We calculated each patient's body mass index (BMI), and compared those within a ‘healthy BMI’ with those considered to be ‘obese’ and ‘morbidly obese’ to determine if patients with higher BMI:
Undergo more three-dimensional imaging pre/post-operatively
Experience more returns to theatre
Have a longer length of hospital stay
Are more likely to require a tracheostomy or intensive care stay
Results
We have shown that patients with higher BMI are subject to more investigations and operative intervention than their ‘healthy BMI’ counterparts. We attribute this to difficulties differentiating between excess adipose tissue and true oedema when assessing those patients with high BMI.
Conclusion
Between 2005-2006, the average annual cost of running a single operating theatre for 27 hours per week was £1.1 million. Furthermore, the cost of expensive three-dimensional imaging modalities and long hospital stays is significant. One can appreciate the significant cost-savings and decreased morbidity for patients with high BMI if unnecessary investigations and interventions could be avoided.
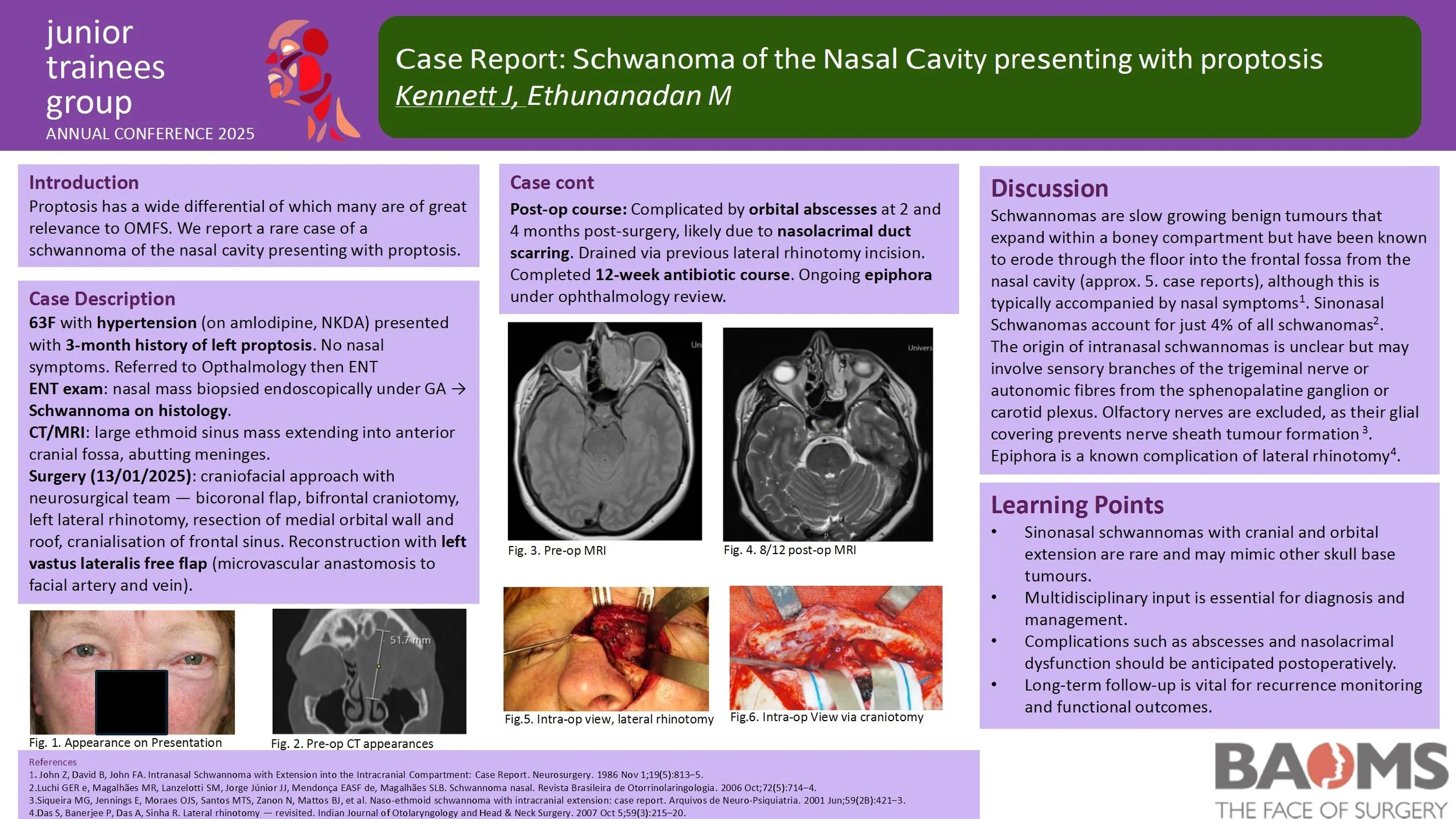
Case Report: Schwanoma of the Nasal Cavity presenting with proptosis
Introduction
Within the literature there are well established risk factors implicated in the most severe cervicofacial infections - of which obesity is included. However, to date, no one has considered how a larger body habitus may change clinicians investigative decision making and management strategies.
Method
We conducted a retrospective analysis of all cervico-facial infections over the last 6 years who underwent incision and drainage at QEUH in Glasgow. We calculated each patient's body mass index (BMI), and compared those within a ‘healthy BMI’ with those considered to be ‘obese’ and ‘morbidly obese’ to determine if patients with higher BMI:
Undergo more three-dimensional imaging pre/post-operatively
Experience more returns to theatre
Have a longer length of hospital stay
Are more likely to require a tracheostomy or intensive care stay
Results
We have shown that patients with higher BMI are subject to more investigations and operative intervention than their ‘healthy BMI’ counterparts. We attribute this to difficulties differentiating between excess adipose tissue and true oedema when assessing those patients with high BMI.
Conclusion
Between 2005-2006, the average annual cost of running a single operating theatre for 27 hours per week was £1.1 million. Furthermore, the cost of expensive three-dimensional imaging modalities and long hospital stays is significant. One can appreciate the significant cost-savings and decreased morbidity for patients with high BMI if unnecessary investigations and interventions could be avoided.
An Audit To Investigate Waiting Times For Patients Requiring Local Anaesthetic Procedures Under The Target Pathway
Introduction
Head and neck cancers represent a significant public health concern in the UK, with rising incidence, mortality rates and late diagnoses. Despite national efforts to streamline diagnostic pathways, delays persist for OMFS referrals. This audit evaluates the efficiency of the diagnostic pathway for suspected malignancies under local anaesthetic procedures (LASP), focusing on adherence to NHS England’s 28-day best-practice timeline, implemented from June 2024.
Method
A retrospective audit was conducted from August to October 2024, reviewing 46 patients referred under the two-week wait (2WW) pathway to OMFS across two sites (BGH and CF). Data was extracted from scheduled LASP lists, patient's documentation, assessing time intervals from referral to clinic, LASP appointments, histology, and follow-up. Comparisons were made with the previous audit cycle to identify trends and areas for improvement.
Results
Only 1 out of 46 patients met the 28-day referral-to-diagnosis target. While 91% of referral forms were dated, just 43% met the recommended 3–6 day upload window. Weekend referrals and ENT triage contributed to delays. LASP was performed within 14 days for 48% of patients, and histology results were available within 21 days for 59%. Malignant diagnoses accounted for 6% of lesions, with a notable increase in dysplastic findings (22%) compared to the previous cycle (7%). Buccal mucosa remained the most commonly biopsied site.
Conclusion
Despite some improvements, significant delays remain in achieving timely diagnosis for head and neck cancer referrals. Key bottlenecks include referral upload times, ENT triage, and limited adherence to the 28-day pathway. Enhanced education for referrers, dedicated LASP slots, and improved triage protocols are recommended to streamline the diagnostic process and improve patient outcomes. Further cycles will aim to include additional sites and refine data collection to support targeted interventions. This audit is targeted for improving patient clinical outcomes, safety and effectiveness of quality care.
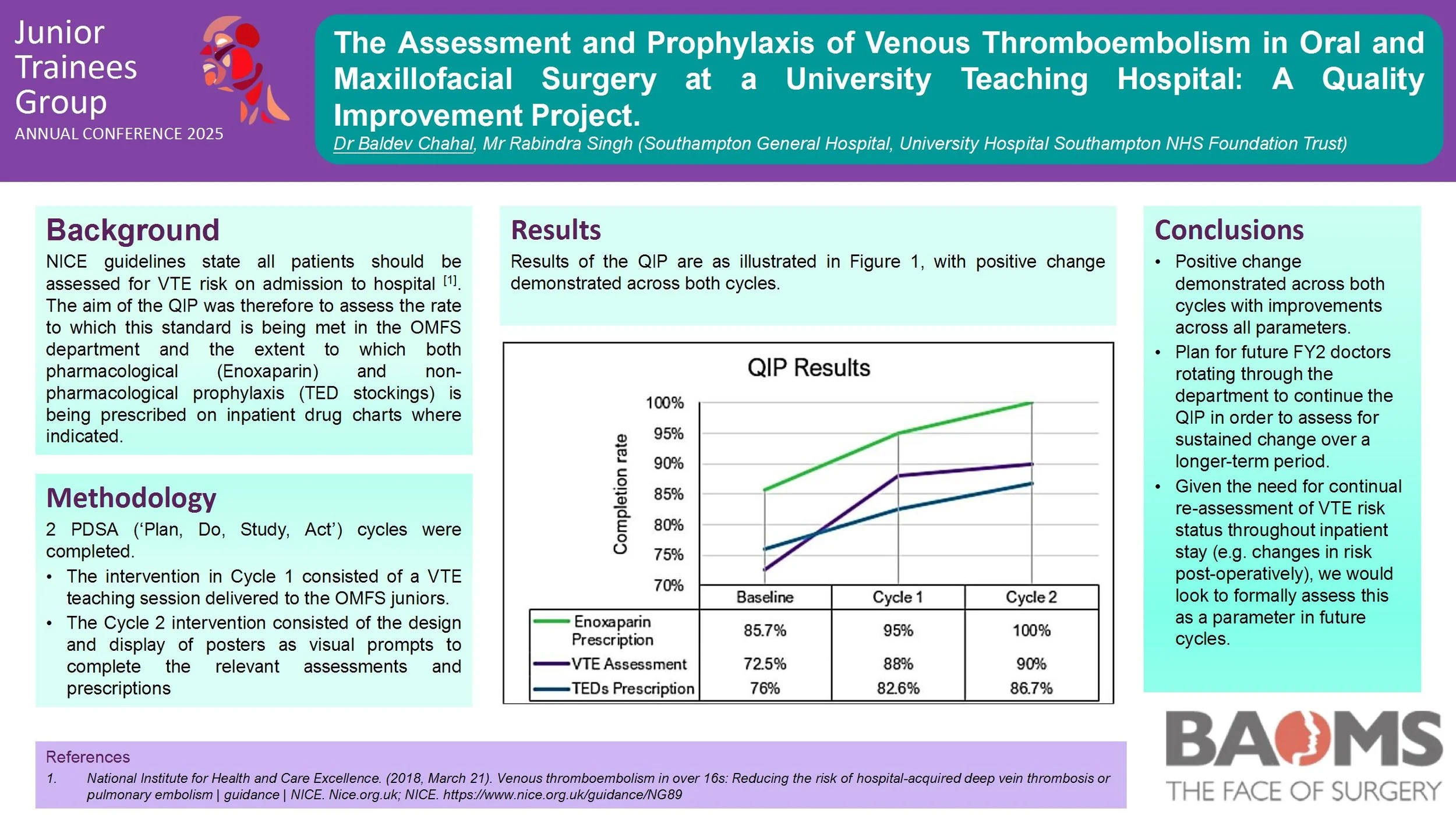
The Assessment and Prophylaxis of Venous Thromboembolism in Oral and Maxillofacial Surgery at a University Teaching Hospital: A Quality Improvement Project.
Introduction
The Oral and Maxillofacial Surgery (OMFS) department is unique in its composition of both medical and dental professionals, with the dental team often unfamiliar with the principles of venous thromboembolism (VTE) prophylaxis prior to commencing their placements. NICE guidelines state all patients should be assessed for VTE risk on admission to hospital. The aims of the QIP involved assessing adherence to this standard in the OMFS department and the extent to which both pharmacological (Enoxaparin) and non-pharmacological prophylaxis (TED stockings) is being prescribed on inpatient drug charts where indicated.
Methods
Baseline data collection was performed to identify areas for performance improvement. 2 PDSA (‘Plan, Do, Study, Act’) cycles were subsequently completed. The intervention in Cycle 1 consisted of a VTE teaching session delivered to the OMFS juniors. The Cycle 2 intervention consisted of the design and display of posters as visual prompts to complete the relevant assessments and prescriptions.
Results
The baseline data collection demonstrated a VTE risk assessment completion rate of 72.5% (29/40). Of the patients assessed to require enoxaparin prophylaxis, this was prescribed on the inpatient drug chart in 85.7% (18/21). Of the patients assessed to be suitable for TED stockings, these were only prescribed on the drug chart in 76% (22/29). Positive change was subsequently demonstrated in Cycle 1 with a risk assessment completion rate of 88% (23/26), enoxaparin prescription completion rate of 95% (19/20) and TEDS prescription rate of 82.6% (19/23). Cycle 2 demonstrated sustained change; risk assessment completion rate of 90% (15/20), enoxaparin prescription rate of 100% (15/15), and TEDS prescription rate of 86.7% (13/15).
Conclusion
Positive change demonstrated across both cycles with improvements across all
parameters. Plan for future FY2 doctors rotating through the department to continue the QIP in order to assess for and implement sustained change over a longer-term period.
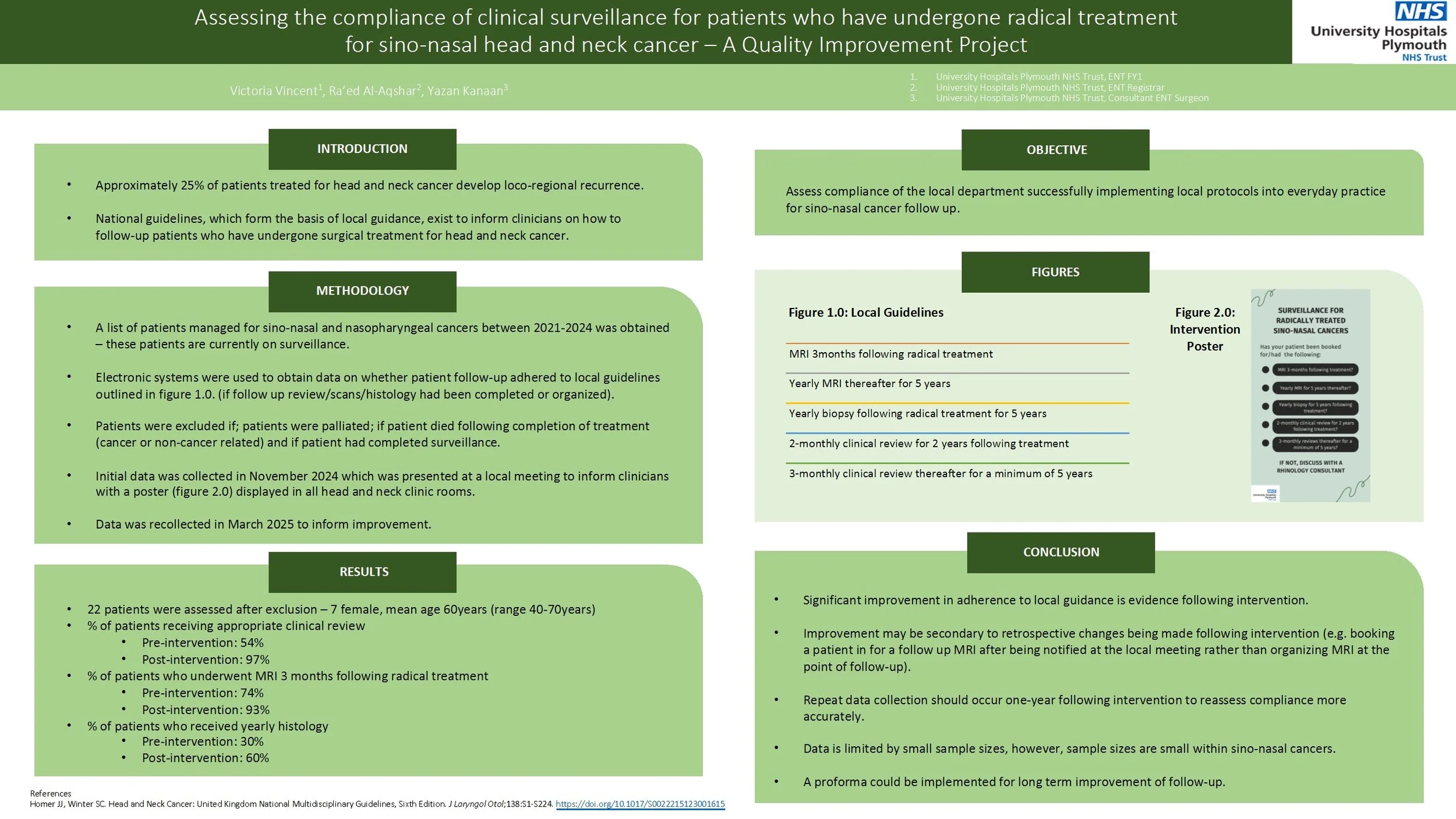
Assessing the compliance of clinical surveillance for patients who have undergone radical treatment for sino-nasal head and neck cancer – A Quality Improvement Project
Approximately 20% of patients treated for head and neck cancer develop loco-regional recurrence. National guidance, which forms the basis of local guidance, exists on how clinicians should follow-up patients following radical surgical treatment for head and neck cancer. The aim of the quality improvement project was to assess whether patients were being adequately followed up following radical management of sino-nasal cancers based upon local guidance.
Patients who underwent radical management of sino-nasal and nasopharyngeal cancers between 2020-2023 at one South West Trust were assessed using available online databases. Compliance to local guidance regarding follow up was assessed. Patients were excluded if they were palliated or if the patient died during treatment. Following the first cycle, the data was presented at the local departmental teaching and a poster reminding clinicians of the follow up criteria was implanted within clinic rooms. Data was then recollected 3 months later.
40 patients were coded as having new sino-nasal cancers. 22 patients were assessed after exclusion. There was improvement in the percentage of patients who had clinical review arranged within the correct timeframe from 54% to 97%. Percentage of patients who had an MRI arranged improved from 74% to 93%. Percentage of patients who had a biopsy arranged improved from 30% to 60%.
Although improvement was achieved within this audit, there were limitations within the study. Namely, the leading clinician was able to identify the patients who did not have correct follow up arranged from the initial audit cycle and arranged this himself, thus not demonstrating a direct link between intervention and change. There were also small sample sizes, however, this reflects the nature of the cohort of patients with sino-nasal cancers. Recommendations would include re-auditing at 1-2years to assess for continued improvement and to obtain more data.
Improving Compliance with Anticoagulant and Antiplatelet Guidelines in Minor Oral Surgery: A Quality Improvement project
Introduction:
The Scottish Dental Clinical Effectiveness Programme (SDCEP) published updated guidance in 2022 regarding the management of patients taking oral anticoagulant and antiplatelets for dental treatment including biopsies.
The aim of this audit is to investigate the outpatient clinic’s current compliance with SDCEP 2022 guidance. This involves reviewing the documentation of dictated letters and communication of pre-operative advice related to anticoagulant and anti-platelet therapy. All patients should be receiving appropriate and documented advice regarding their medications prior to surgery.
Method:
20 consecutive patients were selected between 25/01/25 and 28/02/25 from the MOS clinics. Inclusion criteria comprised patients having a planned local anaesthetic dentoalveolar procedure, such as a dental extraction or intra-oral biopsy, and take anticoagulant and/or antiplatelet.
Results:
Of the 20 patients, 8 received correct and documented pre-operative information regarding their medication. However,12 patients had no documented medication advice. Assuming patients continued their medications as usual, 7 patients would have managed their medications appropriately, while 5 would have done so incorrectly.
The primary issue identified among patients not receiving correct advice was the failure to instruct patient to withhold their morning doses of DOACs for high-risk bleeding procedures, such as intra-oral biopsies. To address these gaps, a teaching session will be delivered for all clinicians.
Conclusions:
Accurate documentation of pre-operative instructions regarding anticoagulants and anti-platelets is essential to minimise risk of post-operative complications and to mitigate potential medico-legal risks. This audit has highlighted key areas for improvement.
To ensure sustained improvement, a third cycle audit is recommended in six months to reassess compliance with SDCEP guidelines and evaluate the effectiveness of implemented changes.
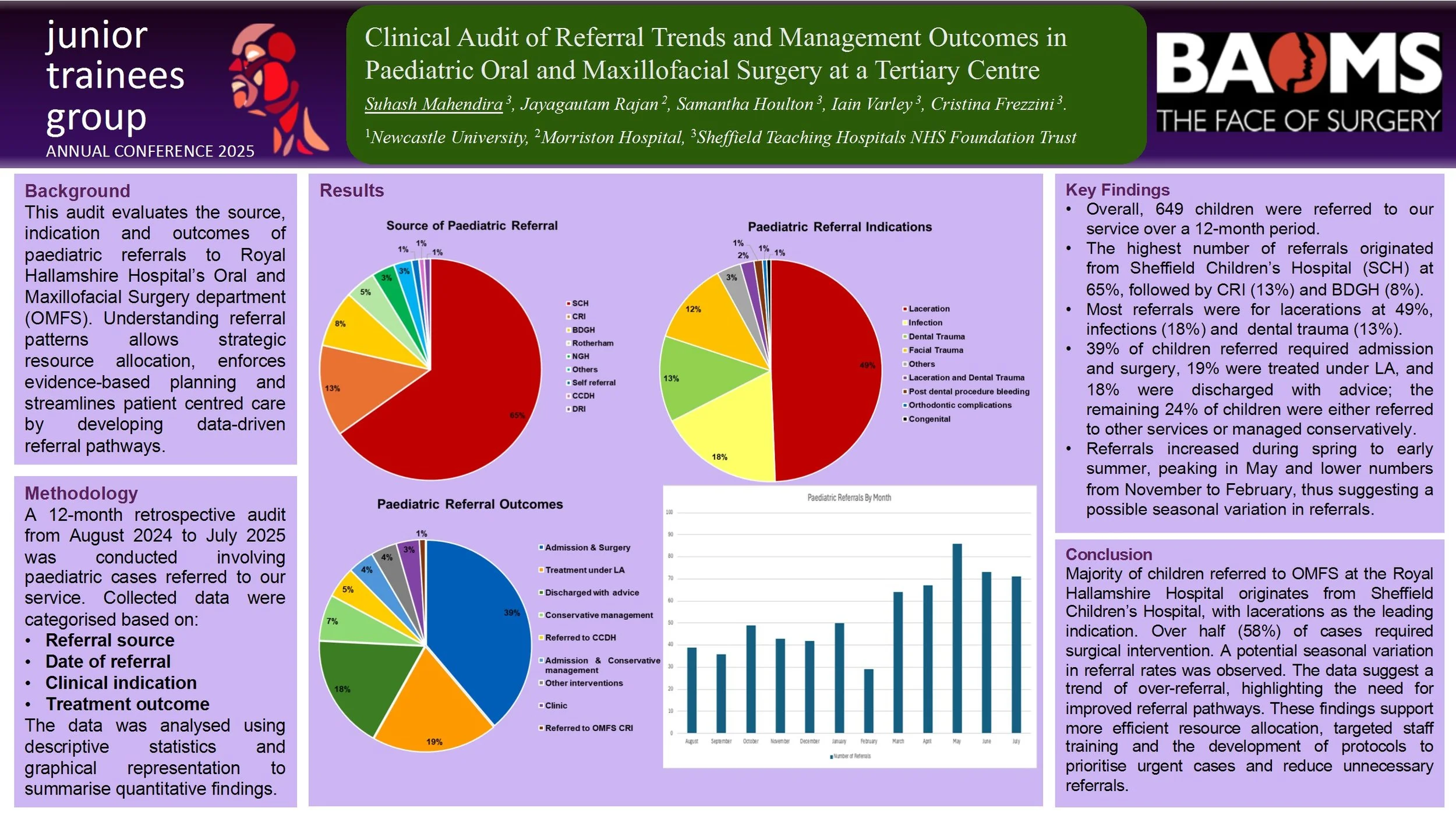
Clinical Audit of Referral Trends and Management Outcomes in Paediatric Oral and Maxillofacial Surgery at a Tertiary Centre
Introduction: Efficient referral pathways are crucial for prompt and exceptional paediatric surgical care. This audit evaluates the trend, demography and outcomes of paediatric referrals to Royal Hallamshire Hospital’s Oral and Maxillofacial Surgery department (OMFS). The understanding of referral patterns allows for strategic resource allocation, enforces evidence-based planning and streamlines patient centred care by developing data-driven referral pathways.
Methods: A retrospective audit was conducted involving 649 paediatric patients referred to our institution over a 12-month period (August 2024 to July 2025). The data was categorised according to referral source, date, clinical indication and subsequent management. The data was analysed using descriptive statistic and graphical representation for ease of interpretation.
Results: Preliminary analysis revealed a sizeable variation in referral sources and clinical indications. A notable portion of referrals originate from Sheffield Children’s Hospital (65%) with laceration (49%) being the major indication of referral. Majority of paediatric patients underwent admission and surgery at 39% followed by treatment under local anaesthesia (LA) at 19%. This audit also indicates the highest frequency of referrals are in the month of May at 86, inversely February reported the lowest frequency at 29.
Conclusion: The trend demonstrates significant seasonal variation and potential over-referral in certain categories. This audit emphasizes the need for closer cooperation and clear communication channels between primary care providers, district hospitals and other tertiary centres. The findings provide actionable insights to guide resource allocation, informed decision making and infrastructure development. Enhanced triage protocols, appropriate staff education, and adequate manpower could mitigate unnecessary hospital referrals and encourages timely interventions of high priority cases.
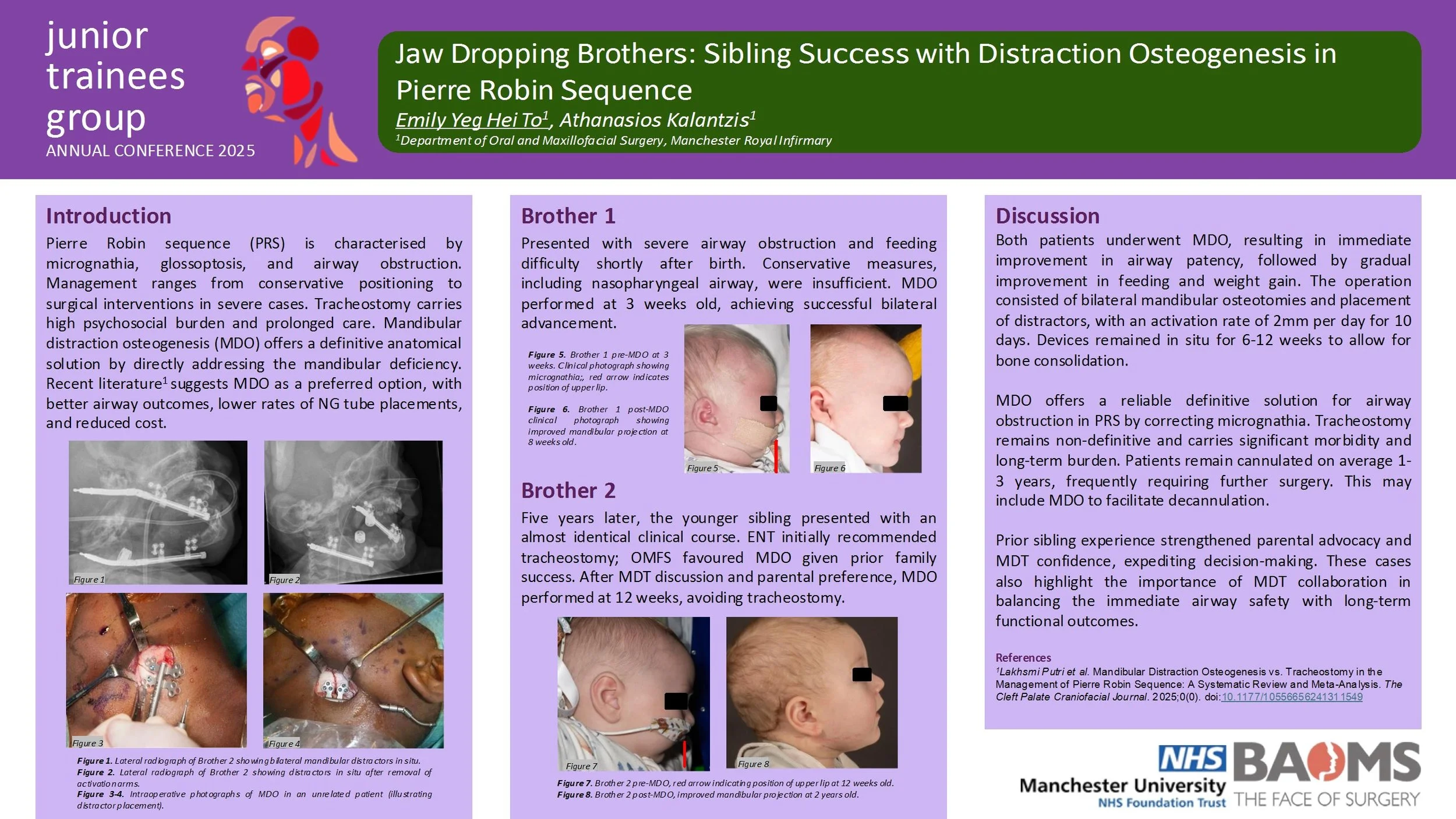
Jaw Dropping Brothers: Sibling Success with Distraction Osteogenesis in Pierre Robin Sequence
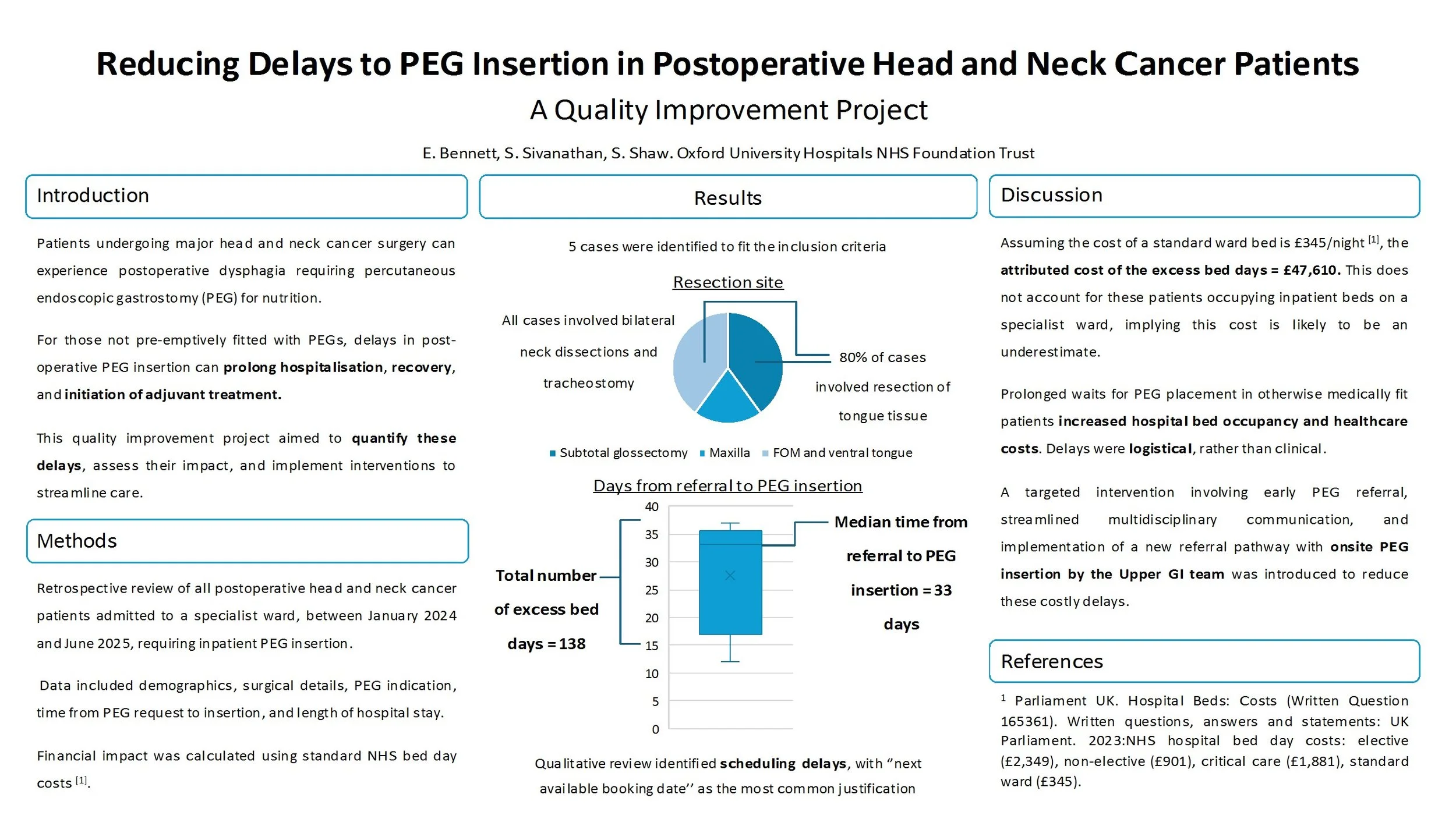
Reducing Delays to PEG Insertion in Postoperative Head and Neck Cancer Patients: A Quality Improvement Project
Introduction:
Patients undergoing major head and neck cancer surgery can experience postoperative dysphagia requiring percutaneous endoscopic gastrostomy (PEG) for nutrition. For those not pre-emptively fitted with PEGs, delays in post-operative PEG insertion can prolong hospitalisation, recovery, and initiation of adjuvant treatment. This quality improvement project aimed to quantify these delays, assess their impact, and implement interventions to streamline care.
Methods:
A retrospective review of all postoperative head and neck cancer patients admitted to a specialist ward, in a single centre, between January 2024, and June 2025, requiring inpatient PEG insertion was done. Data included demographics, surgical details, PEG indication, time from PEG request to insertion, and length of hospital stay. Financial impact was calculated using standard NHS bed day costs.
Results:
Five patients met inclusion criteria. All had extensive surgical procedures including bilateral neck dissections and tracheostomy. Median time from PEG request to insertion was 33 days (range: 12–37 days). Qualitative review revealed scheduling delays, with “next available booking date” as the most common justification. These delays accounted for 138 excess bed days, equating to an estimated cost of £47,610.
Discussion:
Prolonged waits for PEG placement in otherwise medically fit patients increased hospital bed occupancy and healthcare costs. Delays were logistical, rather than clinical. A targeted intervention involving early PEG referral, streamlined multidisciplinary communication, and onsite PEG insertion by the Upper GI team was introduced.
Conclusion:
Delayed PEG insertion in postoperative head and neck cancer patients leads to avoidable hospitalisation, financial burden, and may delay adjuvant treatment. Reasons for delay were specific to logistical factors within the unit. Results were presented and led to the implementation of an onsite referral pathway and improved interdepartmental coordination in order to offer a sustainable solution.
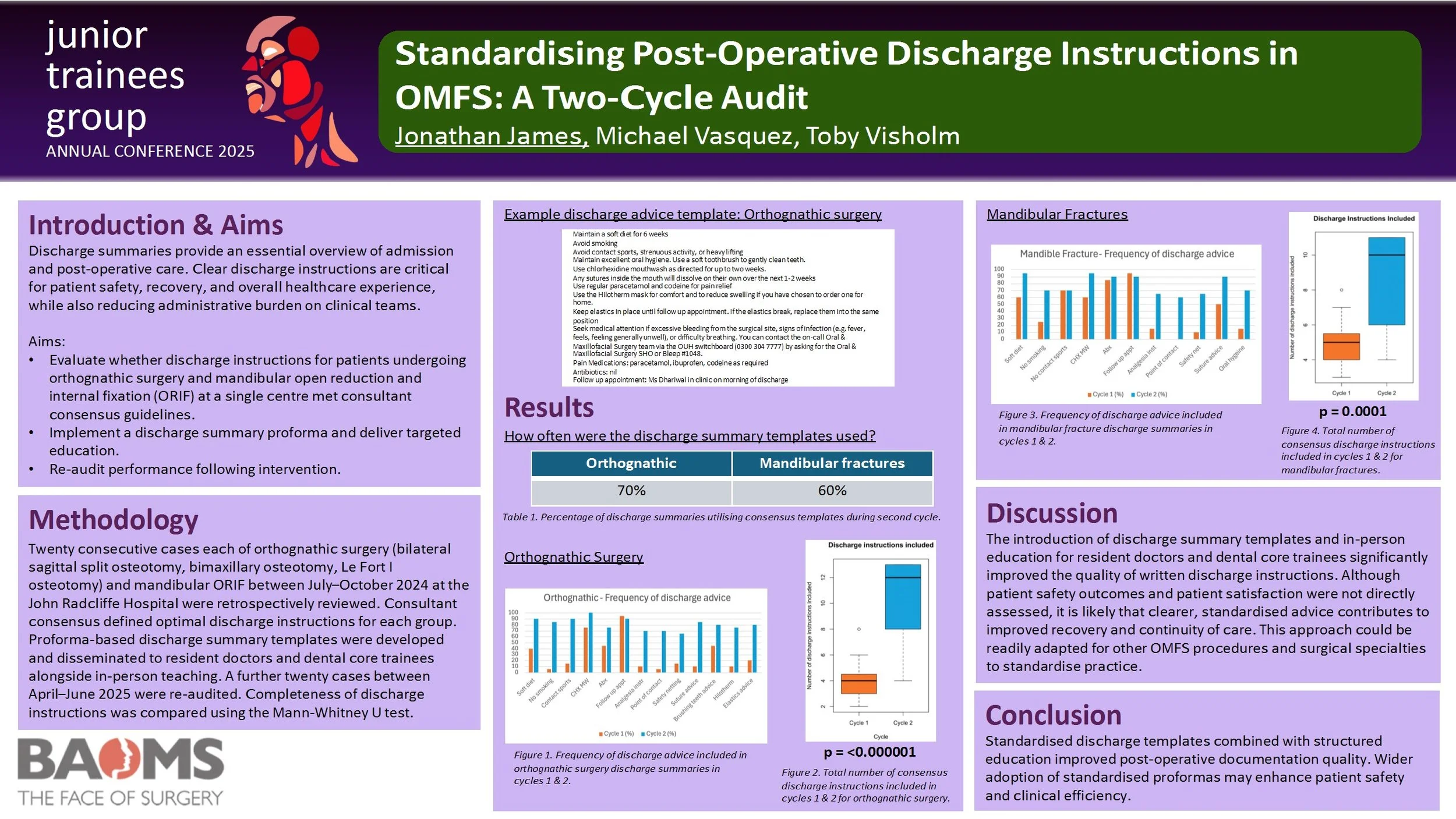
Standardising Post-Operative Discharge Instructions in OMFS: A Two-Cycle Audit
Introduction
Discharge summaries provide an essential overview of admission and post-operative care. Clear discharge instructions are critical for patient safety, recovery, and overall healthcare experience, while also reducing administrative burden on clinical teams.
Aims
1. To evaluate whether discharge instructions for patients undergoing orthognathic surgery and mandibular open reduction and internal fixation (ORIF) at a single centre met consultant consensus guidelines.
2. To implement a discharge summary proforma with targeted education.
3. To re-audit performance following intervention.
Methods
Twenty consecutive cases of orthognathic surgery (bilateral sagittal split osteotomy, bimaxillary osteotomy, Le Fort I osteotomy) and mandibular ORIF between July–October 2024 at the John Radcliffe Hospital were retrospectively reviewed. Consultant consensus defined optimal discharge instructions for each group. Proforma-based discharge summary templates were developed and disseminated to resident doctors and dental core trainees alongside in-person teaching. A further twenty cases between April–June 2025 were re-audited. Completeness of discharge instructions was compared using the Mann-Whitney U test.
Results
In the second cycle, templates were used in 70% of orthognathic cases and 60% of mandibular fracture cases. There was a significant improvement in the total number of relevant discharge instructions included for both orthognathic surgery (p = 0.0000006) and mandibular fractures (p = 0.0001).
Discussion
The introduction of discharge summary templates and in-person education for resident doctors and dental core trainees significantly improved the quality of written discharge instructions. Although patient safety outcomes and patient satisfaction were not directly assessed, it is likely that clearer, standardised advice contributes to improved recovery and continuity of care. This approach could be readily adapted for other OMFS procedures and surgical specialties to standardise practice.
Conclusion
Standardised discharge templates combined with structured education improved post-operative documentation quality. Wider adoption of standardised proformas may enhance patient safety and clinical efficiency.
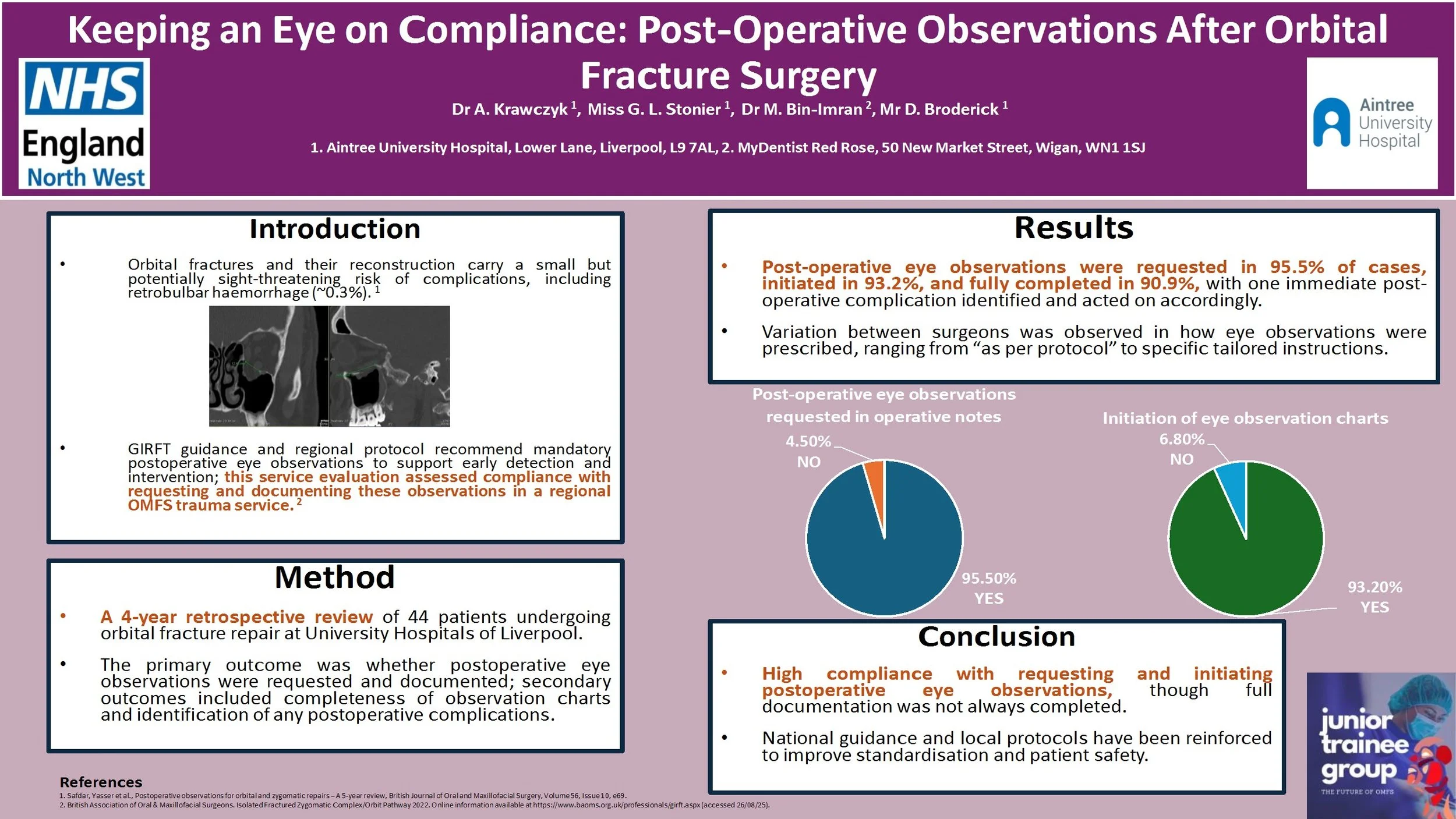
Keeping an Eye on Compliance: Post-Operative Observations After Orbital Fracture Surgery
Introduction:
Orbital fractures and the following reconstructive surgery carries a risk of sight-threatening complications, including retrobulbar haemorrhage (~0.3%).1 The Getting It Right First time (GIRFT) guidance2 and our regional protocol recommends mandatory postoperative eye observations to allow for early recognition and therefore intervention in case of developing sight‐threatening complications. This service evaluation assessed compliance of a regional Oral and Maxillofacial trauma service with requesting and documenting eye observations following orbital fracture surgery.
Method:
A retrospective review of 44 consecutive patients undergoing orbital fracture repair between 2020 and 2024 was conducted at University Hospitals of Liverpool Group. Information was recorded using an electronic data collection tool. The primary outcome was whether post-operative eye observations were requested and documented, with secondary outcomes including whether eye observation charts were completed fully and any complications identified.
Results:
Of the 44 patients, post-operative eye observations were requested in operative notes in 95.5% of cases. Majority (93.2%) of patients had eye observation charts initiated, with complete documentation recorded in 90.9%. One case displayed an immediate post-operative complication. Variation in practice between surgeons was noted, with some prescribing eye observations ‘as per protocol’ and others outlining specific recommendation.
Conclusion:
Compliance with requesting and initiating documentation of post-operative eye observations was high but full completion was inconsistent. National guidance and local protocol have been reinforced to optimise patient safety.
References:
1. Safdar, Yasser et al., Postoperative observations for orbital and zygomatic repairs – A 5-year review, British Journal of Oral and Maxillofacial Surgery, Volume 56, Issue 10, e69.
2. British Association of Oral & Maxillofacial Surgeons. Isolated Fractured Zygomatic Complex/Orbit Pathway, 2022. Online information available at https://www.baoms.org.uk/professionals/girft.aspx (accessed 26/08/25).
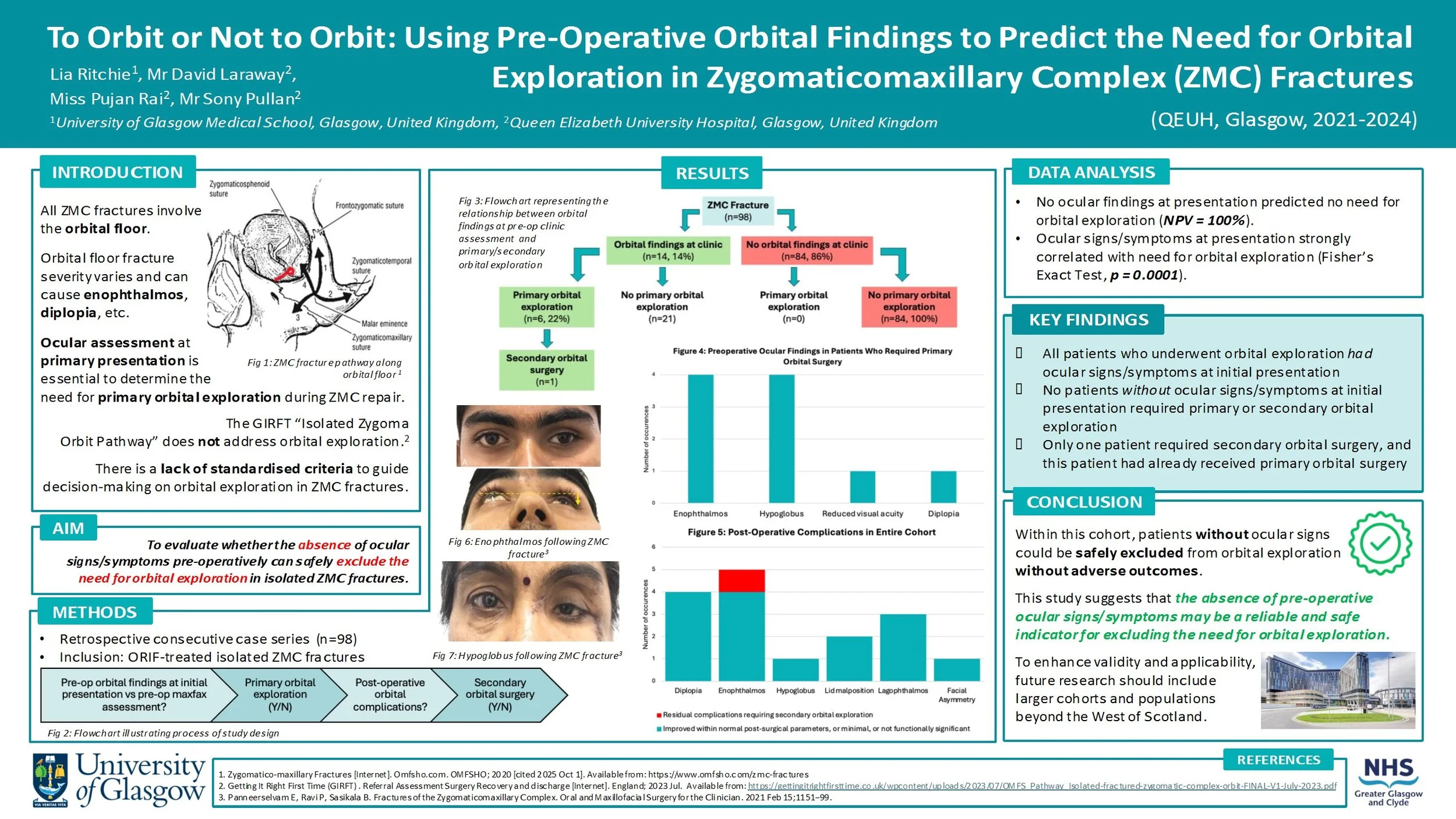
To Orbit or Not to Orbit: Using Pre-Operative Orbital Findings to Predict the Need for Orbital Exploration in Zygomaticomaxillary Complex (ZMC) Fractures
Introduction:
All ZMC fractures involve orbital fractures, with orbital floor fracture severity varying depending on the mechanism and energy of injury. Disruption of the orbital floor changes the orbital volume, increasing the risk of ocular signs/symptoms (e.g. enophthalmos, diplopia). This must be assessed at primary presentation to decide if primary orbital surgery should be performed alongside ZMC repair.
There is currently no standardised set of criteria to guide the decision-making process for orbital exploration in ZMC fractures. This study will evaluate whether the absence of ocular signs/symptoms pre-operatively can safely exclude the need for orbital exploration.
Method:
Data was retrospectively collected from a consecutive series of 98 patients who had ZMC fractures requiring ORIF intervention at the QEUH between 2021-2024. The presence/absence of ocular signs/symptoms at initial assessment was recorded. The cohort was then assessed to determine which patients underwent primary orbital exploration. Post-operative outcomes were reviewed, including whether any patients subsequently required secondary orbital surgery.
Results:
27 patients (28%) presented with ocular signs/symptoms, 6 of them underwent primary orbital surgery. Among the 71 patients (72%) who had no ocular findings at initial presentation, none required orbital surgery. Only 1 patient in the cohort required secondary orbital surgery, and this patient had also undergone primary orbital surgery.
Conclusion:
The absence of pre-operative ocular signs/symptoms may be a reliable indicator for excluding the need for orbital exploration. No patients who did not receive primary orbital exploration needed secondary orbital exploration, proving there were no late ocular complications from this approach.
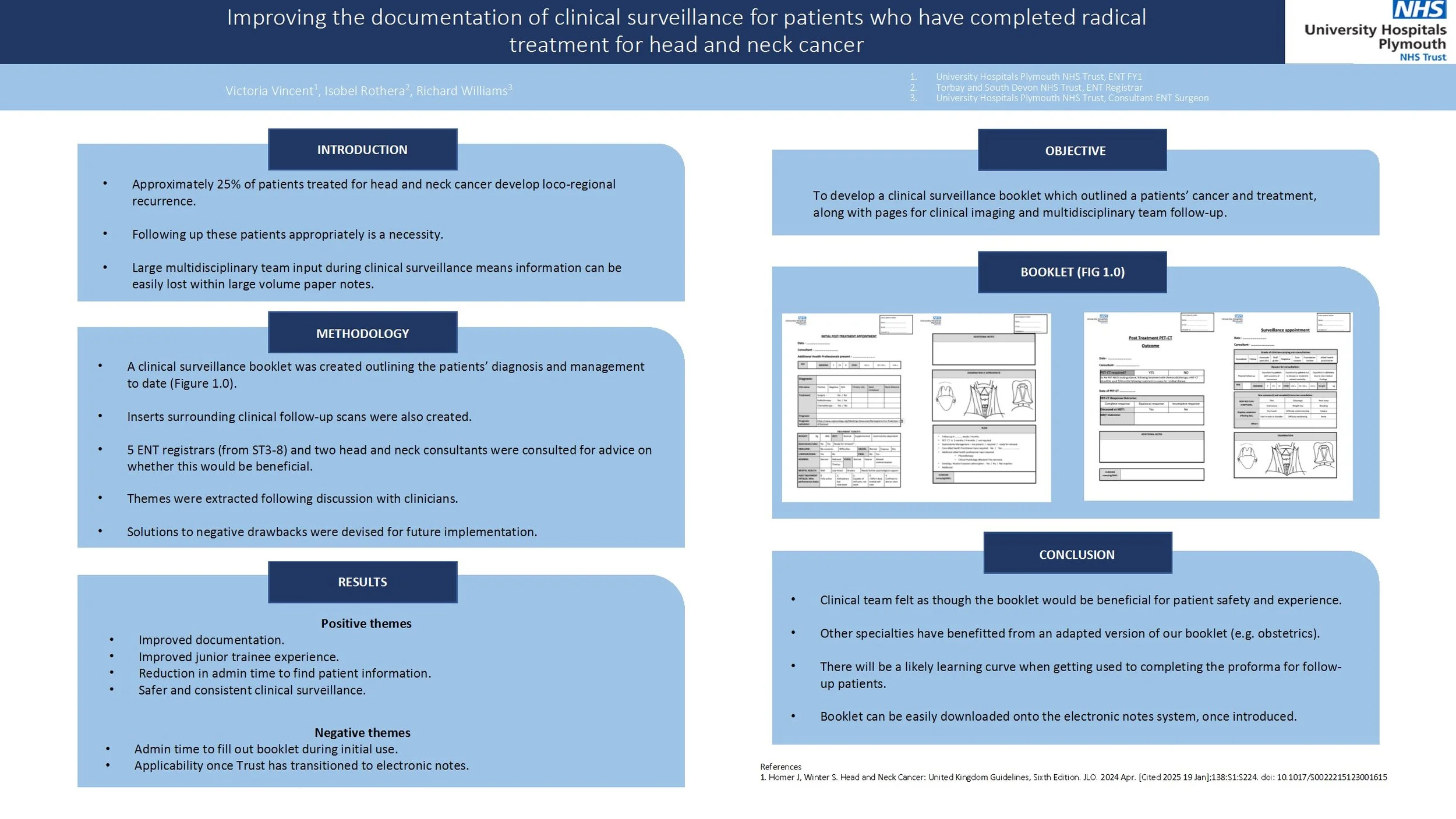
Improving the documentation of clinical surveillance for patients who have completed radical treatment for head and neck cancer
Approximately 25% of patients treated for head and neck cancer develop loco-regional recurrence. Therefore, ensuring that we are following up these patients appropriately is a necessity. With large multidisciplinary team input during clinical surveillance, it is easy for information to get lost within a large volume of paper notes. Therefore, the aim of this project was to develop a clinical surveillance booklet which outlined the patients’ cancer and treatment, along with pages for clinical imaging and MDT follow-up.
A clinical surveillance booklet was created outlining the patients’ diagnosis and management to date. Inserts surrounding clinical follow-up and scans were also created. Before printing, five ENT registrars ranging from ST3-8 and two head and neck consultants were consulted for advice on whether this would be beneficial.
The main positive themes from interview were surrounding improved documentation, improved junior trainee experience, reduction in admin time to find patient information and safer clinical surveillance.
Main positive themes were surrounding admin time to fill out the booklet and use once the trust has transitioned to electronic notes.
Overall, the clinical team feel as though a clinical surveillance booklet would be beneficial for patient safety and experience. Other specialties, such as obstetrics, have benefitted from an adapted version of our proposed booklet. There will likely be a learning curve when getting used to completing the proforma for follow-up patients. The booklet can be easily downloaded to the electronic notes system, once it has been introduced.
Quality Improvement Project – analysing compliance of Russells Hall Hospital OMFS department against SDCEP Anticoagulant guidelines
Introduction
The Royal College of Anaesthetists (RCA) highlights key considerations when selecting anaesthetic modalities, including operator experience, diagnosis severity, and peri-operative compliance. This Quality Improvement Project (QIP) aimed to assess anaesthetic use in secondary care against RCA guidance and develop a long-term strategy to reduce reliance on CEPOD where possible. Benefits include minimising risks of GA-associated mortality, enabling immediate management, reducing anticipatory stress for children and parents, and optimising resource allocation by alleviating CEPOD pressures.
Method
A retrospective pilot cycle was conducted at University Hospital Wales, followed by two prospective cycles at Dudley Group Hospitals and Royal Wolverhampton Trusts. Each cycle included 20 paediatric OMFS presentations from the emergency department. Data collected comprised age, gender, diagnosis, mechanism of injury, pre-operative compliance, management, anaesthetic modality, and peri-operative compliance. Between the second and third cycle, an action plan was presented to paediatric and OMFS teams.
Results
In the first cycle (mean age 4.75; 70% male), 90% were managed with GA, 5% with inhalation sedation, and 5% with LA. The second cycle (mean age 9.7; 75% male) showed 25% GA, 5% inhalation sedation, and 70% LA. In the third cycle (mean age 8; 70% male), 40% were managed with GA, 5% inhalation sedation, 5% ketamine sedation, and 50% with LA.
Conclusion
The QIP demonstrated varied anaesthetic modalities with increasing uptake of sedation between the second and third cycles. Future improvements include implementing a proforma for children undergoing GA to evaluate alternative modalities, ensuring safer, more efficient decision-making. Incorporating Patient Reported Outcomes from parents and children could further inform service development, providing insights into waiting times, cosmetic results, and anxiolysis during treatment.
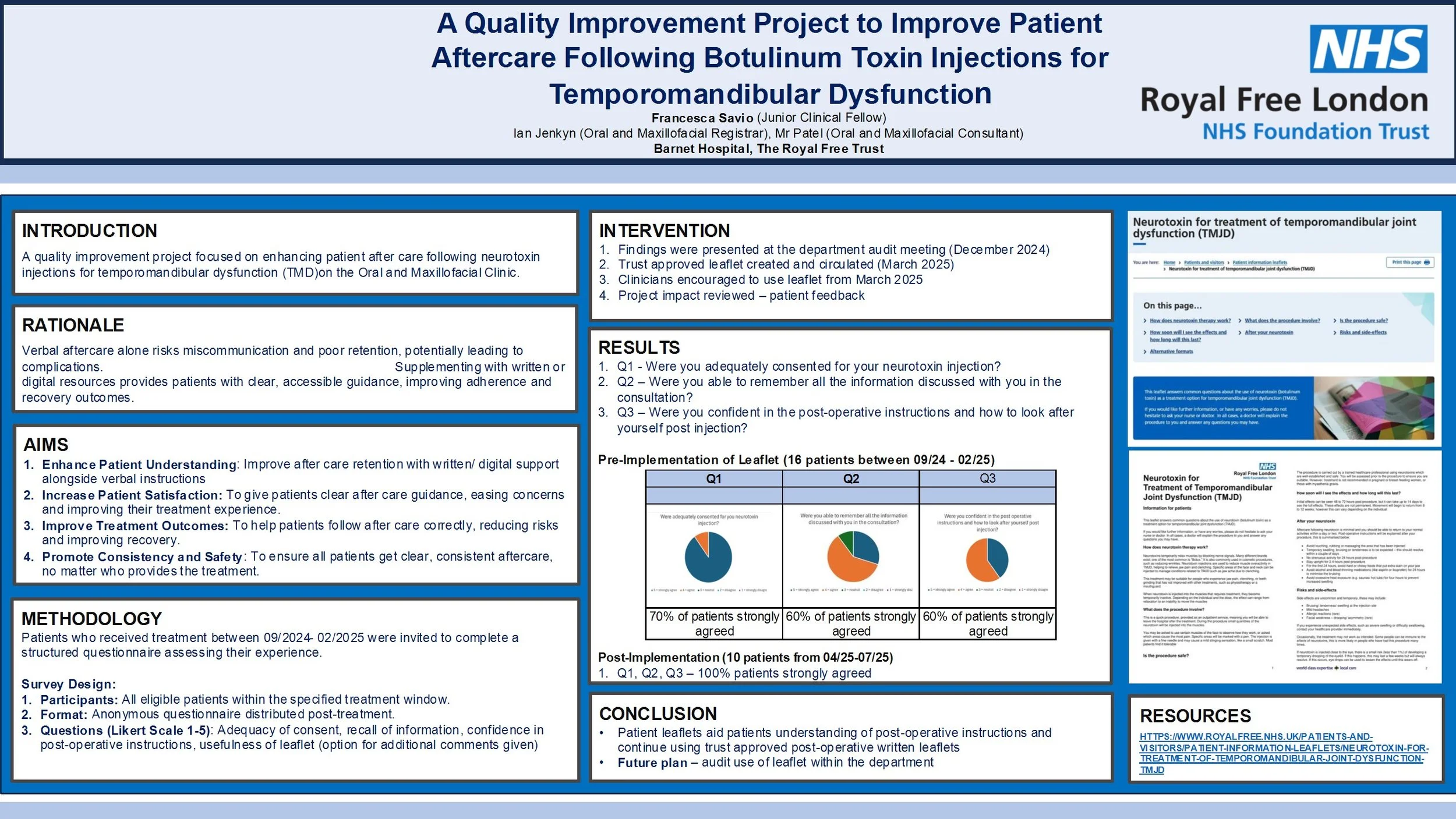
A Quality Improvement Project to Improve Patient Aftercare Following Botulinum Toxin Injections for Temporomandibular Dysfunction
Introduction
Temporomandibular dysfunction (TMD) is increasingly managed with botulinum toxin injections. However, current practice at the Royal Free London NHS Foundation Trust involves providing only verbal aftercare instructions, which may be insufficient for optimal patient understanding and recovery. This quality improvement project aimed to enhance patient aftercare by introducing written resources to supplement verbal guidance.
Method
Two audit cycles were conducted. In Cycle 1 (Feb 2025), patients who received botulinum toxin injections for TMD between Sept 2024 and Feb 2025 were surveyed via telephone using a structured questionnaire. Questions assessed consent quality, recall of verbal instructions, confidence in post-operative care, and interest in written materials. Following Cycle 1, a trust-approved patient leaflet was introduced. Cycle 2 (June 2025) repeated the audit for patients treated after April 2025, evaluating the impact of the leaflet.
Results
Cycle 1 included 16 patients (14 female, 2 male; average age 45). Of the 10 respondents, 90% strongly agreed they were adequately consented, 60% agreed they remembered the verbal instructions, and 100% expressed interest in written aftercare materials. In Cycle 2, patients were surveyed post-leaflet implementation. All respondents (100%) found the written instructions useful and agreed they improved their confidence in post-treatment care.
Conclusion
The introduction of written aftercare materials significantly improved patient satisfaction and confidence in managing post- injections care for TMD. The audit supports continued use of written leaflets as standard practice and highlights the importance of multimodal communication in clinical care. Future audits will monitor long-term outcomes and adherence to aftercare protocols.
An Audit on the Use of Physiotherapy Referral as Part of First-Line Management for Myogenic TMD In An OMFS Department
Title: A Quality Improvement Project on the Use of Physiotherapy Referral as Part of First-Line Management for Myogenic TMD in an OMFS Department
Background:
Myogenic TMD is a common condition managed primarily with conservative treatment, including physiotherapy. National guidance from Getting It Right First Time (GIRFT) highlights physiotherapy as a key first-line intervention. However, referral practices can be inconsistent, risking suboptimal patient outcomes.
Aim:
To assess whether new patients diagnosed with myogenic TMD were appropriately being diagnosed and referred for physiotherapy in an Oral and Maxillofacial Surgery department, and to evaluate the impact of targeted interventions.
Standards:
100% of new myogenic TMD patients should be considered for physiotherapy referral, in line with GIRFT and departmental guidelines.
Methods:
Two audit cycles (n=50 each) were completed. Inclusion criteria: new patients diagnosed with myogenic TMD. Exclusion criteria: arthrogenic or trauma-related TMD, or those beyond initial management. Data were collected retrospectively from electronic records.
Between cycles, a structured intervention was implemented, including:
• Creation of a dedicated Cerner physiotherapy referral pathway
• Departmental teaching and governance presentations
• Visual prompts and email reminders
Results:
Referral rates improved from 14% in Cycle 1 to 70% in Cycle 2. Patient demographics were comparable across cycles, with no significant gender or age-related differences in referral patterns.
Conclusion:
Initial referral rates were significantly below expected standards. Following simple, targeted interventions, compliance improved fivefold. This highlights the effectiveness of education and system-based changes in improving adherence to evidence-based TMD management.
Recommendations:
Further efforts should focus on standardising diagnosis documentation, embedding referral prompts, and re-auditing to ensure sustained improvement. Consideration should also be given to evaluating patient outcomes and physiotherapy attendance in future cycles.
Reducing Delays to PEG Insertion in Postoperative Head and Neck Cancer Patients - A Quality Improvement Project
Reducing Delays to PEG Insertion in Postoperative Head and Neck Cancer Patients: A Quality Improvement Project
Introduction:
Patients undergoing major head and neck cancer surgery can experience postoperative dysphagia requiring percutaneous endoscopic gastrostomy (PEG) for nutrition. For those not pre-emptively fitted with PEGs, delays in post-operative PEG insertion can prolong hospitalisation, recovery, and initiation of adjuvant treatment. This quality improvement project aimed to quantify these delays, assess their impact, and implement interventions to streamline care.
Methods:
A retrospective review of all postoperative head and neck cancer patients admitted to a specialist ward, in a single centre, between January 2024, and June 2025, requiring inpatient PEG insertion was done. Data included demographics, surgical details, PEG indication, time from PEG request to insertion, and length of hospital stay. Financial impact was calculated using standard NHS bed day costs.
Results:
Five patients met inclusion criteria. All had extensive surgical procedures including bilateral neck dissections and tracheostomy. Median time from PEG request to insertion was 33 days (range: 12–37 days). Qualitative review revealed scheduling delays, with “next available booking date” as the most common justification. These delays accounted for 138 excess bed days, equating to an estimated cost of £47,610.
Discussion:
Prolonged waits for PEG placement in otherwise medically fit patients increased hospital bed occupancy and healthcare costs. Delays were logistical, rather than clinical. A targeted intervention involving early PEG referral, streamlined multidisciplinary communication, and onsite PEG insertion by the Upper GI team was introduced.
Conclusion:
Delayed PEG insertion in postoperative head and neck cancer patients leads to avoidable hospitalisation, financial burden, and may delay adjuvant treatment. Reasons for delay were specific to logistical factors within the unit. Results were presented and led to the implementation of an onsite referral pathway and improved interdepartmental coordination in order to offer a sustainable solution.
Re-audit of time to surgery for mandibular fractures following implementation of the Head and Neck Assessment Hub (HANAH)
Introduction
Recent studies have shown that delays in the treatment of mandibular fractures are not associated with adverse outcomes, and this has challenged the common practice of recommending treatment within 24 hours. However, the BAOMS Trauma Special Interest Group advocates early operation to facilitate prompt discharge. We aim to analyse the time from admission to operation of mandibular fractures and identify any reasons for delays.
Method
Retrospective data was collected from records of all admitted mandible fractures over a 3 month period between May and July in 2022, 2023 and 2025 from a major trauma hospital. Time from admission to operation was measured and compared to the standard that 100% of mandibular fractures will undergo open reduction and internal fixation (ORIF) within 48 hours of admission. Data collected also included: patient demographics, other injuries, theatre type, complications and discharge time.
Results
77% (10/13), 79% (15/19) and 76% (13/17) of mandible fractures underwent ORIF within 48 hours of admission over the same 3 month period in 2022, 2023 and 2025 respectively. The mean, median and range of time to undergo ORIF from admission for: 2022 was 36.5 hours, 27 hours, 11-100 hours respectively; 2023 was 40.4 hours, 19 hours, 0-282 hours respectively; 2025 was 26.7 hours, 19 hours, 5-63 hours respectively. There were 0, 4 and 6 post-operative complications over the 3 month period in 2022, 2023 and 2025 respectively.
Conclusion
The set standard was not met and the proportion of mandible fractures that underwent operation within 48 hours of admission over the years is consistently around 76-79%. Unlike previous years, 3 of the cases that underwent operation over 48 hours in 2025 had post-operative complications. We will continue to monitor to see if a dedicated trauma list would be indicated.
Connecting Patients and Providers: A Quality Improvement Initiative in Head and Neck Cancer Care
Introduction
Patients with head and neck cancer are often treated across multiple hospitals, leading to confusion about appointments, treatment stages, and who to contact. This quality improvement project aimed to improve communication by introducing a clear, unified leaflet outlining the full treatment pathway. The project involved trusts in London and Essex, with UCLH as the central site for surgery.
Methodology
The leaflet was co-developed with input from consultants, clinical nurse specialists, and admin staff from UCLH, Queen’s, and the Royal London Hospital. It explained each step of the patient journey from diagnosis to surgery and follow-up and was translated into several languages to reflect local populations. Patients received the leaflet at pre-assessment and were asked to complete a six-question survey before and an eight-question survey after reading it.
Results
Survey results were on a scale from 1-5 and displayed marked improvements. Familiarity with the care process rose from an average of 2.3 to 4.2. Confidence in navigating appointments and services improved from 2.1 to 4.1. Understanding of treatment stages increased from 2.4 to 4.3. Clarity around locations and contact points also improved. More than 90% of patients rated the leaflet as clear and helpful. At £50 per 1000 copies, the leaflet was low-cost. Challenges included translation funding, legal permissions, and coordination between sites, though these were manageable.
Conclusion
This QIP offers a simple, scalable solution to a common communication gap in cancer care. By creating a multilingual, patient-friendly resource in both print and digital formats, the project has improved patient understanding and pathway navigation. Future work will assess long-term effects on patient satisfaction and whether the approach can be expanded to other specialties.
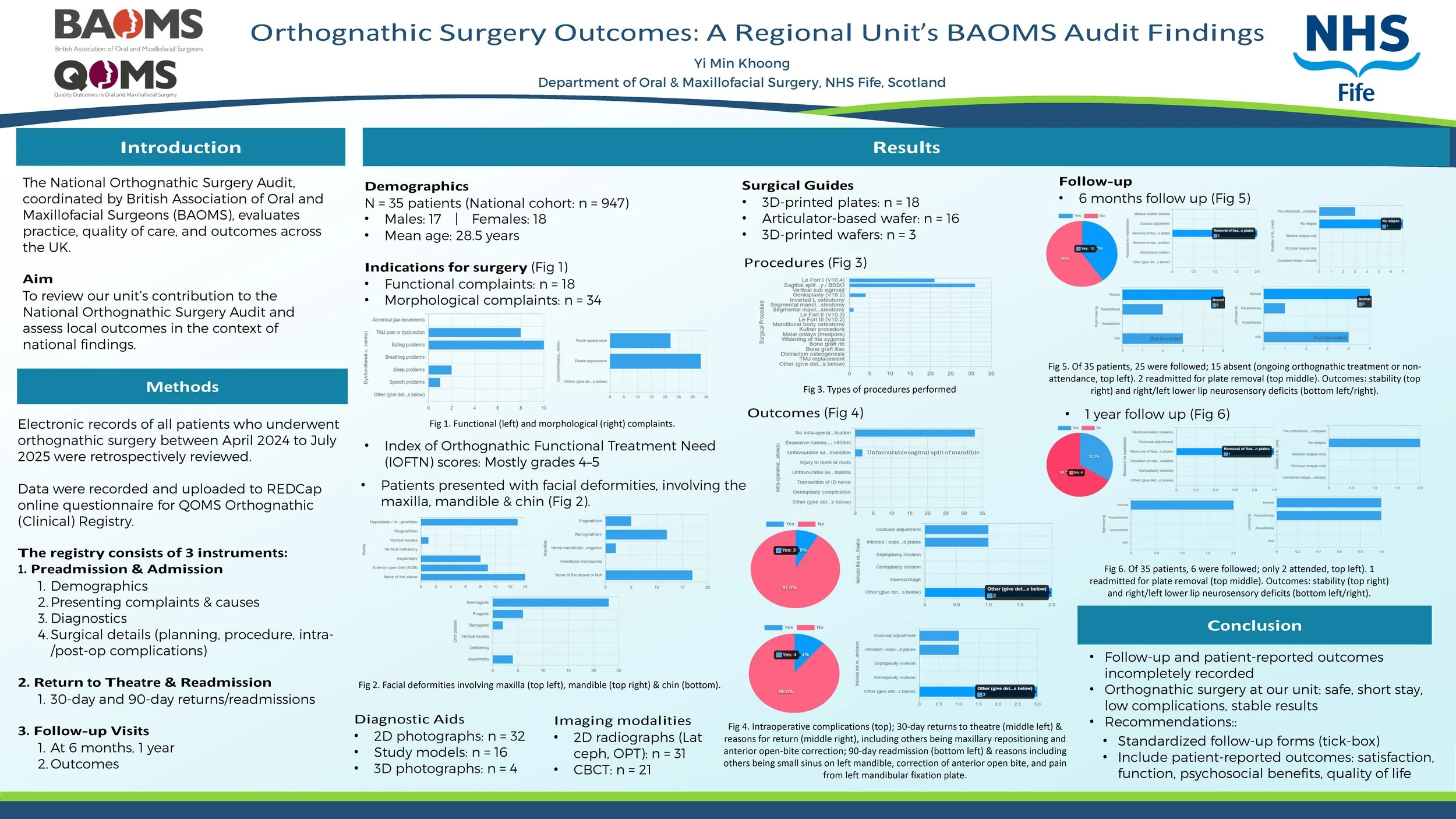
Orthognathic Surgery Outcomes: A Regional Unit’s BAOMS Audit Findings
Introduction
The National Orthognathic Surgery Audit conducted by British Association of Oral and Maxillofacial Surgeons (BAOMS) aims to assess practice, quality of care, and outcomes throughout the UK. This retrospective audit presents findings from a regional maxillofacial unit, which contributed 35 patients to the national cohort of 947 from April 2024 to July 2025.
Methods
A review was conducted of all patients who underwent orthognathic surgery at our unit during this period. Data was collected on demographics, presenting complaints, diagnoses, treatment plans, surgical procedures, and postoperative outcomes.
Result
The cohort included 17 males and 18 females, with a mean age of 28.53 years. Indications encompassed functional issues (e.g., masticatory difficulties, TMJ dysfunction), and morphological deformities (facial, dental appearance). IOFTN scores were predominantly 4–5, reflecting high need.
The majority underwent combined procedures, most commonly Le Fort I osteotomy and bilateral sagittal split osteotomy, with a smaller proportion receiving genioplasty. Planning methods included both traditional and digital approaches, ranging from standard articulator-based techniques and wafers to advanced 3D planning with 3D-printed wafers.
The median inpatient stay was 1 day (range 0–2), with 10 patients discharged within 24 hours. Intraoperative complications were uncommon, with 2 cases of unfavourable sagittal split of mandible. A minority (5 patients) returned to theatre within 90 days, primarily for fixation plate-related problems and occlusal adjustments.
At follow-up, outcomes were stable with minimal relapse rates and acceptable neurosensory deficit. One readmission occurred within 1 year for plate removal. Documentation of follow-up and patient-reported outcomes was inconsistent across cases.
Conclusion
Orthognathic surgery at our unit demonstrates safe practice, short inpatient stay, low complication rates, and stable results. Follow-up documentation could be improved using a standardized tick-box, and patient-reported outcomes (e.g., satisfaction, functional and psychosocial benefits, quality of life) should be incorporated to better capture treatment impact.
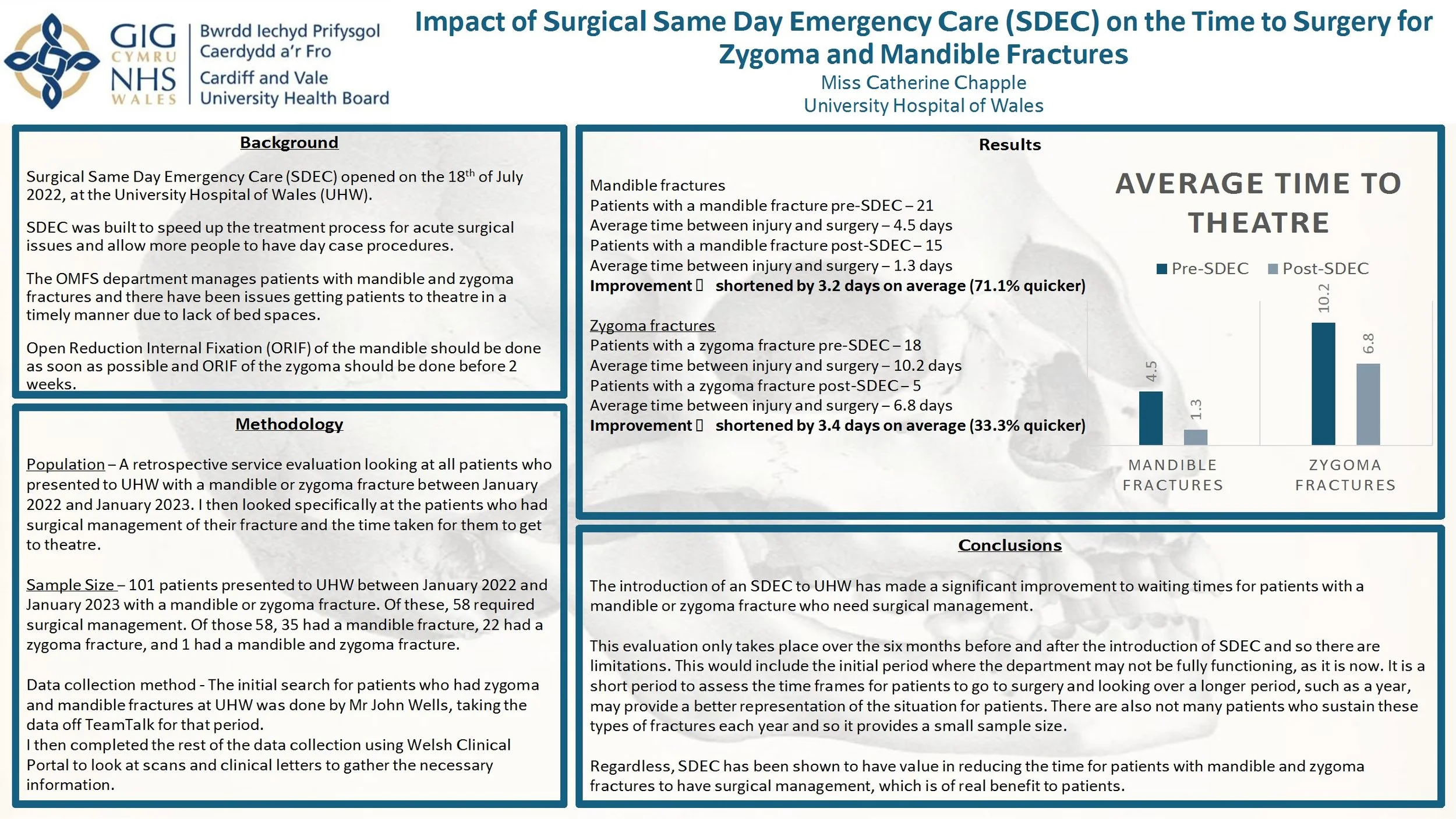
Impact of Surgical Same Day Emergency Care (SDEC) on the Time to Surgery for Zygoma and Mandible Fractures
Introduction: Surgical Same Day Emergency Care (SDEC) opened on July 18th 2022 at the University Hospital of Wales (UHW). It aimed to accelerate the treatment process for acute surgical procedures and allow more day case procedures. The OMFS department manages patients with mandible and zygoma fractures and there were delays to surgical management due to lack of bed spaces. Open reduction internal fixation (ORIF) of the mandible should be done as soon as possible and ORIF of the zygoma should be done before 2 weeks. This service evaluation investigates whether the opening of SDEC had an impact on the waiting times for patients with mandible and zygoma fractures to have surgery.
Method: This is a retrospective service evaluation looking at all patients who presented to UHW with a mandible or zygoma fracture between January 2022 and 2023. I looked specifically at patients who had surgical management. The initial search for patients was done by taking data from TeamTalk and the rest of the data collection was from Welsh Clinical Portal.
Results: 101 patients presented to UHW between January 2022 and 2023 with a mandible or zygoma fracture. Of these, 58 required surgical management. Patients with a mandible fracture had their surgery 3.2 days earlier on average and patients with a zygoma fracture had their surgery 3.4 days earlier on average, after the implementation of SDEC.
Conclusion: The introduction of SDEC to UHW has made a significant improvement to waiting times for patients with mandible or zygoma fractures who need surgical management. However, this evaluation only looks at the management of patients 6 months before and after the implementation of SDEC and it is important to investigate over a longer period. Regardless, SDEC has been shown to have value in reducing the time taken to achieve surgical management.