JTG 2025 Poster Gallery
Keeping an Eye on Compliance: Post-Operative Observations After Orbital Fracture Surgery
Introduction:
Orbital fractures and the following reconstructive surgery carries a risk of sight-threatening complications, including retrobulbar haemorrhage (~0.3%).1 The Getting It Right First time (GIRFT) guidance2 and our regional protocol recommends mandatory postoperative eye observations to allow for early recognition and therefore intervention in case of developing sight‐threatening complications. This service evaluation assessed compliance of a regional Oral and Maxillofacial trauma service with requesting and documenting eye observations following orbital fracture surgery.
Method:
A retrospective review of 44 consecutive patients undergoing orbital fracture repair between 2020 and 2024 was conducted at University Hospitals of Liverpool Group. Information was recorded using an electronic data collection tool. The primary outcome was whether post-operative eye observations were requested and documented, with secondary outcomes including whether eye observation charts were completed fully and any complications identified.
Results:
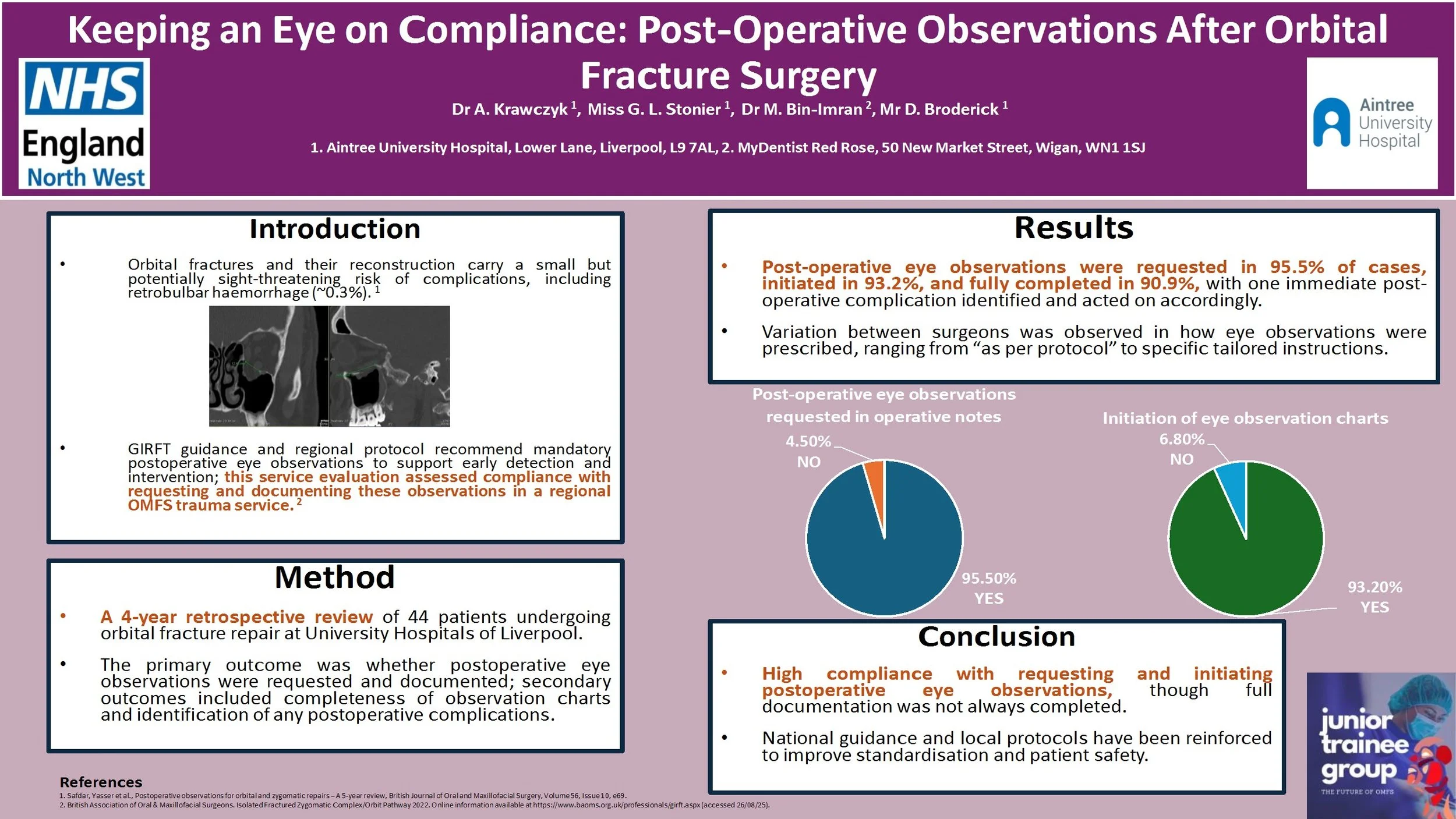
Of the 44 patients, post-operative eye observations were requested in operative notes in 95.5% of cases. Majority (93.2%) of patients had eye observation charts initiated, with complete documentation recorded in 90.9%. One case displayed an immediate post-operative complication. Variation in practice between surgeons was noted, with some prescribing eye observations ‘as per protocol’ and others outlining specific recommendation.
Conclusion:
Compliance with requesting and initiating documentation of post-operative eye observations was high but full completion was inconsistent. National guidance and local protocol have been reinforced to optimise patient safety.
References:
1. Safdar, Yasser et al., Postoperative observations for orbital and zygomatic repairs – A 5-year review, British Journal of Oral and Maxillofacial Surgery, Volume 56, Issue 10, e69.
2. British Association of Oral & Maxillofacial Surgeons. Isolated Fractured Zygomatic Complex/Orbit Pathway, 2022. Online information available at https://www.baoms.org.uk/professionals/girft.aspx (accessed 26/08/25).
Dental abscess or something more?
Introduction:
Necrotising fasciitis is a rare, rapidly progressive soft tissue infection with high morbidity and mortality, often polymicrobial (Type I) and associated with immunocompromised states. Prompt recognition and aggressive surgical management are essential.
Case report:
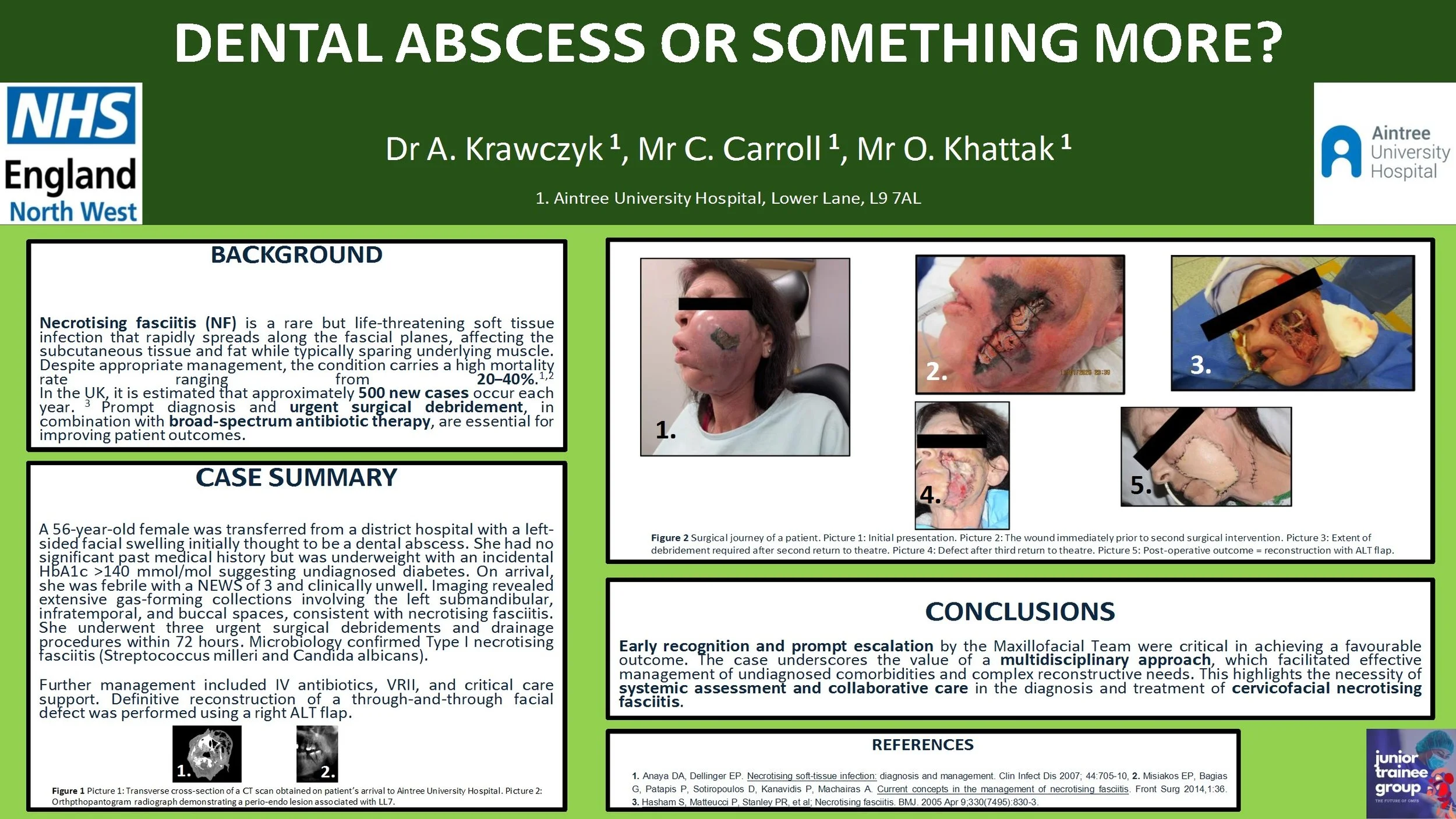
A 56-year-old female was transferred from a district hospital with a left-sided facial swelling initially thought to be a dental abscess. She had no significant past medical history but was underweight with an incidental HbA1c >140 mmol/mol suggesting undiagnosed diabetes. On arrival, she was febrile with a NEWS of 3 and clinical unwell. Imaging revealed extensive gas-forming collections involving the left submandibular, infratemporal, and buccal spaces, consistent with necrotising fasciitis. She underwent three urgent surgical debridements and drainage procedures within 72 hours. Microbiology confirmed Type I necrotising fasciitis (Streptococcus milleri and Candida albicans). Further management included intravenous antibiotics, variable rate insulin infusion, and critical care support. Definitive reconstruction of a through-and-through facial defect was performed using a right antero-lateral thigh free flap.
Discussion:
Early recognition and escalation by the on-call Maxillofacial team were key to successful outcomes. A multidisciplinary approach enabled management of complex comorbidities and reconstruction. This case highlights the importance of systemic evaluation and team-based care in managing cervicofacial necrotising fasciitis.